Alanna Badgley wakes up with a sense of doom. Her alarm goes off at 4:45 a.m., but she lies there breathing until 5:15: in through her nose, out through her mouth. Then she throws off the covers, splashes some water on her face, brushes her teeth and puts on her uniform.
Before all this, the Westchester County, N.Y., paramedic religiously ate an Eggo waffle with peanut butter and nutella for breakfast. But lately her stomach’s been in knots, and she’s too nervous to eat in the mornings. Her boyfriend, Rudy Green, has made her lunch—a jar of cut fruit and a Ziploc baggie of veggies and hummus, which is pretty much all she can stomach these days. Badgley stuffs it into her multicolored Jansport backpack and walks to the Empress Emergency Medical Services base in Yonkers, N.Y., clocking in just before 6 a.m. on April 1.
She checks her gear: intubation kits, an oxygen pressure mask, an alternative airway device to help get air into ailing lungs. Someone squawks over the loudspeaker, calling for “Medic 61.”
“That’s me,” she says.
Badgley, 28, is small and sharp, with the quick, sure movements of a paramedic who knows exactly what she’s doing. She responds to 911 calls with emergency medical technicians (EMTs), but typically gets the cases that require more advanced medical help. Lately, that means patients with COVID-19. She can do much of what ER doctors do, often in less optimal conditions. She’s dug through hoarders’ homes to reach her patients, responded to car accidents and sudden births, and once intubated a man while lying on her belly on his bedbug-infested carpet.
These days, paramedics like Badgley are the first line of defense. On March 3, there was one coronavirus case in Westchester County. By April 6, there were nearly 14,000, including 197 deaths, according to the New York Times. Even though her department is not yet out of personal protective equipment (PPE), Badgley has been wearing the same N95 mask for two weeks, protecting it with a surgical mask during the day and disinfecting it at night.
In this global pandemic, with doctors overwhelmed and hospitals forbidding visitors, paramedics like Badgley also take on another role: they are often the first medical professional seen by the patient in distress, and the last one seen in person by their family. The moment she arrives can be, for some patients, the last time they see the people they love.
It’s often up to her to tell patients’ families that they can’t ride in the ambulance and can’t come to the hospital, and to stand there as they slowly realize that her arrival could mean a permanent goodbye. “Whoever would normally be there with you isn’t going to be there,” she says. Badgley tries to make up for it in the ambulance by holding the patient’s hand, rubbing their back, and providing the one-on-one comfort she knows they’re unlikely to get once they get to crowded hospitals. “I’m there to talk to them,” she says, “and to provide some level of empathy and humanity in the moment in which they are truly terrified.”
The first call of the day comes in at 6:58 a.m: a car accident on Sprain Brook Parkway. At 7:28, the radio squawks again: this time, the dispatcher says “screening positive,” indicating that the patient is exhibiting high fever, shortness of breath, or cough, all symptoms of Covid-19. As Badgley puts on the siren to head to the location, she hears a second call, for 30 Alpha 2— Green’s identifier. She smiles when she hears it, the paramedic version of running into your boyfriend at the office.
She and Green met on the job three years ago, and they’ve spent most of their working hours over the last three weeks responding to 911 calls for coronavirus patients. Nine of their coworkers have tested positive for Covid, she says, and many others have called out sick but haven’t been officially diagnosed. At this point, Badgley and Green figure they both have the virus already, and if they don’t, they will soon. “We had a conversation about, ‘how would you want to be buried? Do you want to be cremated?’” she says. They’re millennials, without enough savings to worry about a will, but she told him she’d like to be buried under a tree in a biodegradable bag. “Those are things I never thought I’d have to think about.”
At 7:41, Badgley arrives at a brick apartment building across from a boarded-up church in northern Yonkers. She puts on goggles and her N95 mask, hooks her surgical mask over her ears, grabs her big blue bag and heads inside. The patient is a woman in her 70s who speaks only Spanish. She has severe abdominal pain, a high fever and low oxygen levels. As Badgley and the EMTs get the patient onto the stretcher, she looks over and sees the Spanish language news channel airing footage of paramedics responding to COVID-19 patients.

An hour later, there’s another squawk over the radio: a patient at a nursing home, not verbally responsive, “screening positive.” It’s a moaning woman in a green top, nearly unconscious, her lips and fingers blue. “Can you tell me your name?” Badgley asks. “Can you tell me where you are?” The only sound from the woman is a groan of pain. She needs to be intubated, but it won’t be easy to do here, and besides, an intubation is an aerosolizing procedure, which means it sprays tiny virus-laden particles into the air that can spread the infection. You’d want to wear a Tyvek suit and face shield for a procedure like that.
Badgley knows the woman needs oxygen fast, but she doesn’t want to do anything that could spray the virus and infect others. She gives her nasal oxygen as she wheels her to the ambulance, and then an oxygen mask once they get inside the bus: she knew the nurses would probably intubate her at the hospital. As soon as her oxygen levels come up in the ambulance, the woman starts to improve enough to mumble her name. “Hold my hand, hold my hand, hold my hand,” Badgley says. “It’s okay.” When they get her inside the hospital, nearly everyone they see is on a ventilator.
At 10:05, another radio call: “Patient screening positive.” When Badgley arrives at the cream-and-yellow house, there’s a tree blossoming outside. The patient speaks only Spanish: he’d had a fever for five days, and shortness of breath and chest pain (“straight-up COVID,” Badgley says.) He’s conscious, and strong enough to walk slowly to the ambulance with a pulse oximeter attached to his finger to see if his oxygen level drops as he walks. (It does.) His cough sounds like a barking seal.
Radio call at 10:57: “Screening inconclusive.” It’s an older man who felt weak and dizzy, and fell and injured his arm. “But why was he weak?” Badgley asks rhetorically. Probably COVID. At 11:58: “Screening positive,” an unresponsive patient in Mount Vernon.
By 6pm—the end of her shift—Badgley has taken 11 calls, nine of them for suspected coronavirus patients. The patients are middle-aged and old, black and white, living everywhere from Victorian houses to nursing homes. Most have fever and shortness of breath, but the symptoms can vary. Badgley has noticed only one common thread: “The identifying feature is fear.”
The starting salary for EMTs in Badgley’s unit is $15 an hour. As a paramedic, she has more medical training, so she makes $27 an hour, which with her schedule comes out to about $50,000 a year. “Firefighters make a lot more than us, police officers make a lot more than us, nurses make a lot more than us,” she says. Since January, Badgley has been the president of IAEP Local 20, their chapter of the International Association of EMTs and Paramedics. As union president, she fields questions from paramedics and EMTs about what will happen if they die. “Am I at least going to be considered a line-of-duty death?” they ask her. “Am I at least going to go down as a hero?’”
These days, death is on everyone’s mind. “In 26 years, I’ve never seen anything like this,” says Mount Vernon EMT Sande Mazzariello. “And I was at 9/11.” Mazzariello, 49, doesn’t like to talk about that day, and when asked about it she tends to shake her long black hair and look in a different direction. But she says the coronavirus pandemic causes an even deeper kind of fear. “The chaos was there, but that was all in one day,” she says. “This is every day. It’s scary to get up in the morning to go to work. I’ve never really been afraid of my job.”
Everyone from the New York Governor to President Trump has described the fight against Covid-19 as a war, but EMTs on Badgley’s team say that the shortages of masks and gowns make them feel like they’re being sent out to battle without proper ammunition. “We all signed up for this,” says Marvin Martinez, a 33-year old EMT working with Badgley that day. “But we didn’t sign up for doing it without the equipment we need.”
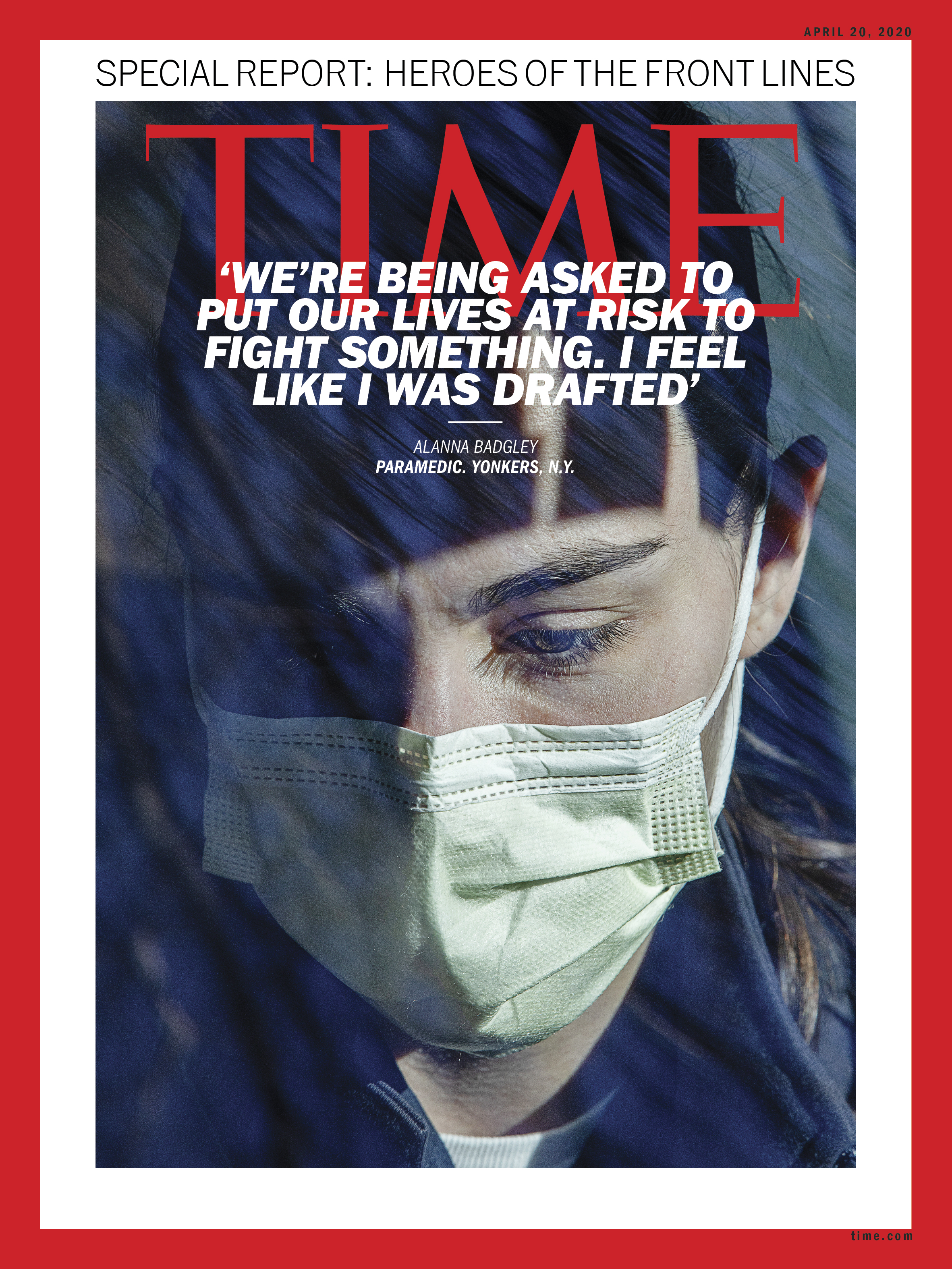
Covid-19 has thoroughly transformed the stakes of the job. “I do feel like we’re being asked to put our lives at risk to fight something,” says Badgley. “I feel like I was drafted.”
EMTs and paramedics are trained to respond to disasters like bus accidents or house fires or terrorist attacks, to trot fearlessly towards scenes of sudden catastrophe. They’re prepared for emergencies, but emergencies don’t usually last this long. It’s upended Badgley’s sense of space and time.
“In some ways you’re looking into the future: you’re looking at Italy and China, you can see where we’re headed,” says Badgley. “But in some ways, because of the lag of the data in the testing, you’re also looking into the past.” The patients they treat today were likely infected a week ago. Next week, they’ll be responding to calls for people infected today. Fighting COVID is like racing towards a star that actually may have burned out centuries ago, but whose light is only just now reaching the eye.

Whenever she needs to take a bathroom break, Badgley goes into St. Joseph’s Hospital in Yonkers. That afternoon, the reception area is crowded with gurneys, and she has to maneuver around people lying on beds in the halls. The gurneys are lined up together so tightly that they’d look like beach chairs if it weren’t for the ventilators. On her way to the bathroom, she runs into an acquaintance, an orderly tasked with putting the dead into body bags. They had both been planning vacations to Jamaica. Instead, they are doing this.
Another call comes through at 2:42 p.m. for a man with difficulty breathing. “Screening positive,” the voice says over the radio. Badgley hangs her head, takes a deep breath, and then turns on her siren. At 2:46, she arrives at a brick apartment building with a big glass door. The patient is a 45-year-old man with a high fever and chest pain. He can’t walk from one room to another without getting winded. He has no appetite and can’t keep food down. He tested positive for COVID, he says. His wife has symptoms, too.
“I know you’re in a lot of pain, okay? But the most important thing is just try to focus on breathing as much as you can,” Badgley tells him. “So, slowly in through your nose, slowly out through your mouth, okay?”
While the EMTs get the man onto the stretcher, his wife pulls Badgley aside. “Please, I want him to be okay,” she says. He had already been to St. Joseph’s and doesn’t want to be sent back there—they want him to go to a hospital in the Bronx. But Badgley’s team is only authorized to take him to an in-county hospital.
“Please don’t let him die,” the woman says.
“We won’t let him die in our ambulance,” Badgley says. Can she guarantee that? Of course she can’t.
This is the part that’s the worst. Badgley is used to seeing her patients as a set of organs that needs urgent transport. “You can remove yourself from the patient: a set of lungs and a heart,” she explains later. “You’re showing empathy of course, but you’re focusing on treating the lungs and the heart.” That’s because until now, she could take a family member in the ambulance, or instruct them to meet the patient at the hospital. She’d know that the family would get to visit, sit by the bedside, direct their questions to the doctor. Before this, she’d be bringing the family along, not separating them. Now, she’s not only treating the patient, but managing their goodbyes.
The woman is crying as the EMTs are wheeling her husband away. “I’ll pray for you,” Badgley says. “You pray for you. And breathe.” Normally, she would hug this woman, but hugs aren’t allowed anymore. Instead, she grips both of her hands in her gloved fingers. She knows the woman is realizing that this may be the last time she sees her husband.
Or maybe not. Maybe he’ll get better, and he’ll be back in a few days. He’s young, and young patients tend to recover more easily. But many of the EMTs and paramedics have a fairly pessimistic view: if you’re sick enough with COVID to be taken to the hospital, they say, things aren’t going well. “To be blatantly honest, they’re all gonna die,” says Martinez.
For now, Badgley focuses on the woman in front of her, who is melting in panic. “You breathe, he breathes, everybody focuses on breathing, okay?” she says. The woman tries. Her symptoms aren’t as bad yet. “There you go. Exactly,” Badgley says. “All right. This is the most important time to focus on breathing. Okay. All right. That’s the first thing. Breathing.”
Breathing, Badgley thinks, is the beginning of it all. The very first thing any of us ever did in our lives was breathe: every life starts with a breath. The woman has calmed down, and the patient is already downstairs at the ambulance with the EMTs. Badgley grabs her bag, heads to the elevator, and presses the button to go down. The elevator doors close, and Badgley stands there in silence, wearing her two-week old mask after her 9th coronavirus patient of the day. She has two hours left on her shift. Tomorrow, she will come back to work, clock in, put on the same mask, and lose two patients before they even make it to the ambulance. But she doesn’t know that yet. For now, she’s just focused on breathing: in through her nose, and out through her mouth.
- Inside Elon Musk’s War on Washington
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Cecily Strong on Goober the Clown
- Column: The Rise of America’s Broligarchy
