The cleverest of enemies thrive on surprise attacks. Viruses—and coronaviruses in particular—know this well. Remaining hidden in animal hosts for decades, they mutate steadily, sometimes serendipitously morphing into more effective and efficient infectious agents. When a strain with just the right combination of genetic codes that spell trouble for people makes the leap from animal to human, the ambush begins.
Such was the case with SARS-CoV-2, the coronavirus behind COVID-19, and the attack was mostly silent and insidious at first. Many people infected with SARS-CoV-2 remained oblivious as they served as the virus’s new home and allowed it to establish a foothold in the global human population. These hosts were the perfect base camp for launching the attack that has upended social norms, economies, political systems and more all across the world.
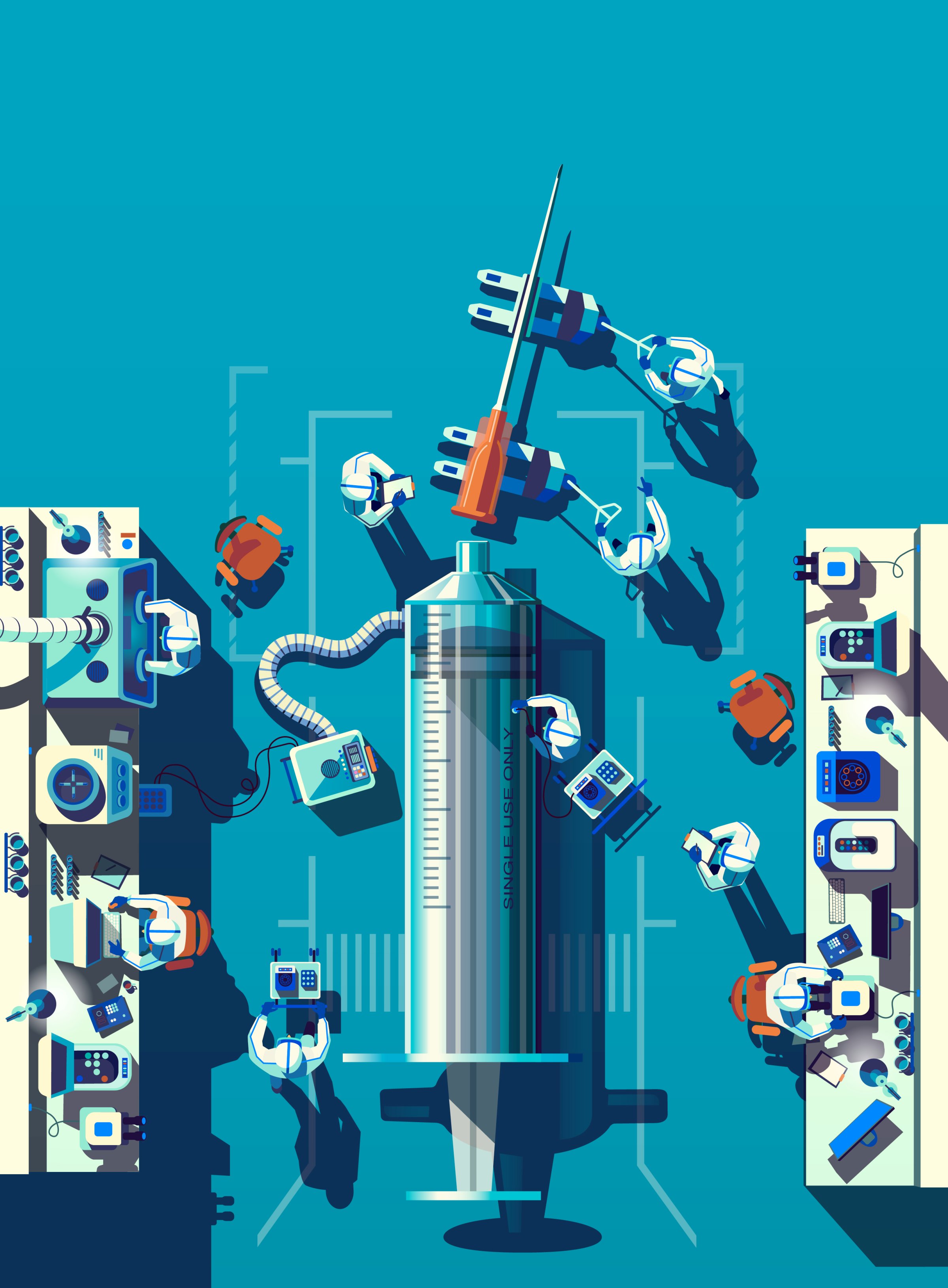
The best hope for confronting this onslaught is a vaccine—if the furious research efforts underway yield effective shots, if manufacturers can distribute them to enough people and if enough of those people actually get immunized.
Vaccines rely on the idea of herd immunity, a type of biological fortress in which the vast majority of the population is protected against infection. One way to get there is via natural infection, which involves enough people getting infected and recovering without serious consequences. But many public-health experts say pushing to open businesses and schools, so healthy people who might not get seriously ill if infected can develop this immunity, is a dangerous strategy that leaves too much to chance; there is no way to predict how much time it will take, and along the way the virus will keep harming and killing people until enough people become immune.
Vaccines have been the scientific detour around natural immunity—offering the benefits of protection without the suffering and unpredictability—since Edward Jenner, in the 1790s, discovered that exposing people to small amounts of the cowpox virus could give them immunity to the smallpox. Today, pharmaceutical and biotech companies are developing or testing more than 100 COVID-19 vaccine candidates and governments are pumping billions of dollars into a massive global effort the likes of which we haven’t seen since the polio epidemic of the 1950s. Everything about this vaccine endeavor could be history-making, from the speed with which shots are developed, to the way they are tested and authorized, to how they are doled out to people around the world. Months after scientists first identified the new coronavirus, Chinese teams are already testing nearly 10 potential vaccines. Fueled by President Donald Trump’s Operation Warp Speed, which will provide at least $10 billion in federal funding for research and testing of promising COVID-19 vaccine candidates, the U.S. is conducting three late-stage trials in healthy volunteers. Other countries—including Italy, Russia, Japan, Singapore, South Korea, Australia and India—have all launched human tests of their own vaccines.
Operation Warp Speed promises to deliver an ambitious 300 million doses by January 2021; to do so, manufacturers including Moderna, AstraZeneca, Pfizer, Sanofi and Johnson & Johnson have already begun to produce their vaccine candidates, before ongoing studies show they are effective. And the U.S. Centers for Disease Control and Prevention (CDC) alerted governors in early September of the government’s plan for how initial doses can be ordered and shipped when they are available.

These are all calculated risks, made more fraught by growing tensions between the political need to restart economies and educational institutions, and the requirements of the rigorous scientific and regulatory process that mandates a threshold of data proving that a new vaccine is safe and effective before it can be released to the public. Russia’s announcement in August that its Ministry of Health had approved a vaccine developed by scientists in Moscow that was still being tested was widely criticized by the scientific community as premature and potentially dangerous to the high-risk groups that would receive it first. In September, soon after major vaccine makers pledged in an unusual show of solidarity to conduct full safety studies on their vaccines before submitting them for regulatory review, AstraZeneca put its trial on hold so researchers could investigate an unexplained illness in one of the study participants.
These actions serve as reminders that the development and testing period for these vaccines is already strained to the stretching point. Massachusetts-based Moderna Therapeutics, along with scientists from the government’s National Institute of Allergy and Infectious Diseases (NIAID), already set records by developing and readying one candidate for human testing in 42 days—a process that in the past has taken years.
And that’s why the accelerated schedule must come with a dose of humility. The quest to develop a vaccine for a new infectious disease is a gamble at best; nearly four decades after HIV was discovered, there is still no effective vaccine against that virus. SARS-CoV-2 is so new to the scientific community that it’s not even clear yet what the human body needs to prevent infection—or if such a thing is even possible. The urgency of the pandemic means doctors will have only about a month’s worth of information from studies on how long the immunity from the shots might last. Given that, some experts, including those developing the vaccine candidates, say we should at best expect a vaccine that can minimize the effects of the disease, rather than provide the “sterilizing immunity” that would protect people from infection entirely. “For many respiratory pathogens, it’s a challenge to achieve a sterilizing immune response,” says Dr. Evan Anderson, associate professor of medicine at Emory University School of Medicine and the lead researcher on one of the Moderna trials. “We don’t know whether that will be the case with SARS-CoV-2.”
Another challenge: just one vaccine likely won’t be enough. From a manufacturing and distribution perspective, immunizing the world’s population will take several different vaccines and probably contributions from all of the companies currently pushing to produce a product. “This is a global problem, and no one company is going to have the solution,” says John Shiver, senior vice president for global vaccine research and development at Sanofi, a French pharmaceutical company. “Because we don’t know what will work, what will work best or what will best serve the need in really, really stopping the pandemic, more shots on goal are important.”
Even with multiple vaccines, it won’t be easy to ensure they get to the right people at the right time. Nearly all of the candidates require two shots, spaced up to a month or so apart. Some vaccines need to be maintained at below-freezing temperatures from the manufacturing plant until close to when they’re injected into a person’s arm. And once the vaccines are shipped to hospitals and medical clinics, who should get immunized first? The most aggressive manufacturing schedules still won’t produce enough vaccines to inoculate everyone, especially in the first few months. Health experts will have to make tough decisions about how to distribute those first precious doses, and are turning to ethical principles such as risk and social utility. These put health care workers, people with existing health conditions and the elderly in group living facilities toward the top of the list, as well as first responders and others working in essential occupations such as teachers, law-enforcement officers and those in waste management.
But, notes Dr. Ezekiel Emanuel, vice provost for global initiatives at the University of Pennsylvania, such discussions haven’t addressed the practicalities. Up to 40% of the U.S. population have existing health conditions that would qualify them for priority vaccination—far more than the number of doses that will likely be available in the first manufacturing runs. “We haven’t really thought it through because it’s a hard problem and therefore we’ve avoided it,” he says. As several of the most promising vaccines barrel toward the final stages of testing, however, avoidance won’t be possible, and decisions will have to be made about the global lottery for this prized resource, choices that could mean the difference between allowing the pandemic to continue its deadly and tragic assault on human life, and finally slowing it down.
How to decide who will get a coronavirus vaccine first
At the broadest level, the distribution question starts with how much vaccine each country should receive. Any hope of benefiting from herd immunity conferred by vaccines dissolves if not enough of the world’s population—the “herd”—is immunized and protected against infection. Researchers at CUNY Graduate School of Public Health and Health Policy used a computer simulation to calculate that if 75% of the world’s population were immunized, the vaccines would need to be 70% effective in protecting against infection in order to control the ongoing pandemic. If only 60% were vaccinated, then that efficacy threshold would jump to 80%.
And manufacturing a safe and effective batch of vaccines, even by deeply experienced pharmaceutical companies with a track record of producing millions of doses of other vaccines, isn’t a slam dunk. “In making vaccines, there is research, development, then implementation,” says Dr. Paul Offit, director of the vaccine-education center at Children’s Hospital of Philadelphia, who serves on the U.S. Food and Drug Administration (FDA) committee that will advise the agency’s director on COVID-19 vaccine approvals. “The hardest of those three is implementation. Mass production is not trivial; mistakes get made, and you learn as you go.” During the U.S. polio-immunization campaign in the 1950s, he notes, one manufacturer failed to properly inactivate the polio virus used in the vaccines and 40,000 children became infected.
The challenges to achieving such widespread immunization aren’t just about reaching manufacturing targets. Dozens of nations are investing in or developing their own vaccines, and there are nationalist arguments for funneling the end products of these investments back to those who financed them, which would lock out countries with fewer health resources from the doses they need. Even in industrialized nations that may produce enough vaccines, uptake could be difficult, given anti-vaccine sentiment in general (stemming largely from unsubstantiated links between certain vaccines and autism) and concerns about the safety of any COVID-19 vaccines in particular. In a recent Ipsos poll commissioned by the World Economic Forum, one-third of Americans said they would not get vaccinated if a COVID-19 shot became available.
While some degree of nationalism is reasonable from a social-justice perspective, says Emanuel, in a global health crisis, allowing the virus to percolate anywhere poses a threat to people everywhere. To stress the need for international unity, the World Health Organization partnered with the vaccine-focused public-private alliance Gavi and the Coalition for Epidemic Preparedness Innovations, a group of philanthropists and governments focused on providing resources needed to respond to infectious-disease threats, to form the COVAX Facility, a mechanism that would allow nations to purchase vaccines at reduced prices by pooling their buying power. The initiative is helping to fund nine vaccine candidates, and countries can sign up to make commitments to buy the shots that end up being effective at volume discounts.
So far, 172 countries have expressed interest in joining, including 80 developed nations and 92 lower- and middle-income countries. The Trump Administration has declined to join COVAX, citing ongoing tensions with the WHO, but even without the U.S., COVAX now represents 70% of the world’s population. International experts have proposed two broad strategies for deciding how much vaccine countries should receive—one that relies on a country’s population and another that uses the proportion of health care workers as a guide—both of which Emanuel believes will fall short of equitable allocation. “People want to be ethical but don’t know what ethical means in this context,” he says. In his view, it involves principles such as reducing harm, premature death and economic hardship, as well as limiting community spread of disease that would put more people in harm’s way.
Even once countries receive their allotted doses, deciding which people should be immunized first raises additional ethical and practical challenges. In the U.S., the National Academies of Sciences, Engineering and Medicine released a draft of prioritization guidelines in September, proposing four tiers of vaccination groups. The first wave of vaccinations would be for high-risk populations including health care workers, people with existing health conditions such as obesity, asthma and heart disease, and the elderly in group living conditions. Next come “critical risk” workers, teachers, older adults, people in group homes, and the incarcerated; then young adults and children; and finally, the rest of the nation. A final draft reflecting public comments on these proposals will be given to the CDC committee responsible for making immunization recommendations for COVID-19 vaccines.
In anticipation, Dr. Nancy Messonnier, director of the National Center for Immunization and Respiratory Diseases at the CDC, in early August informed the health departments of four states (North Dakota, Florida, California and Minnesota) and one city (Philadelphia) that they would be part of a pilot program for rolling out vaccines. The CDC and Operation Warp Speed would collect data from the pilot sites to refine plans for allocating vaccines to the rest of the country. “Our goal,” said CDC director Dr. Robert Redfield in August, “is to ensure no delay in the handoff between FDA authorizing a vaccine and implementation of vaccination programs nationwide.” That all depends, of course, on whether the tens of thousands of volunteers receiving COVID-19 vaccine candidates in current studies develop strong immune responses to SARS-CoV-2 without serious side effects.
How innovation is speeding up the COVID-19 vaccine-development process
When Carol Kelly, an associate nutrition director at Emory University Student Health, saw a request on her NextDoor app in April seeking volunteers to participate in a nearby study for a COVID-19 vaccine candidate, she was immediately intrigued. She called up and found out that this particular study would test a vaccine based on a new genetic technology. No vaccine using this technology has been approved, although a handful, for diseases like respiratory syncytial virus and influenza, are in trials. “They said that it contains the genetic code of the virus. That kind of gave me pause,” Kelly says. But she signed up anyway. “I felt helpless seeing the health care providers working so hard … I thought, If there is one little thing I can do to hurry and help the advancement of a solution, why not?”
The Emory study is testing a vaccine co-developed by scientists from NIAID and Moderna. If successful, it could pioneer a new way of churning out vaccines that would be the fastest in history. Some existing vaccines, including shots for influenza, require manufacturers to grow, over a period of weeks, massive amounts of virus or bacteria, then disable them in the lab so they can’t cause disease but are still foreign enough to alert and activate human immune systems to mount defenses against them.
A major reason Moderna has been able to move so fast is that it bypasses this process and relies instead on mRNA, the genetic material that codes for proteins. On Jan. 10, Chinese scientists posted the first complete genome sequence of SARS-CoV-2; just 42 days later, the Moderna and NIAID teams had used that code to identify which parts of the viral genome would make good targets for building a vaccine—specifically, the code for the spike protein that defines SARS-CoV-2. Encircling the virus’s outer shell like a crown, the spike protein also serves as the lockpicker for breaking into healthy human cells. Once inside, SARS-CoV-2 hijacks those cells’ machinery to pump out more copies of itself to spread throughout the body and continue its mission of infecting and replicating. The way Dr. Stephen Hoge, president of Moderna, sees it, “mRNA is really like a software molecule in biology. So our vaccine is like the software program to the body, which then goes and makes the [viral] proteins that can generate an immune response.”
Moderna produced and shipped its first vial of vaccine for human testing at the end of February. Three months later, it had its first batch of data from a few dozen healthy volunteers in a small, early-stage trial. The vaccine appeared safe and seemed to prompt the immune system to generate antibodies against SARS-CoV-2 in amounts similar to those found in people who had recovered from COVID-19. Kelly kept a diary of her temperature and any unusual symptoms for seven days after the first shot, which she says didn’t affect her much, and the research team took weekly blood samples until her second shot around three weeks later. That injection hit her harder; “Oh my golly, the next day I was exhausted,” she says. “I was just wiped out, had a little bit of vertigo and had a headache, and I never have headaches. I also had a little fever. But the next day I was fine.”
Kelly takes her symptoms as a sign that the vaccine did its job and that her immune system is now primed to defend against SARS-CoV-2. Data from a subset of volunteers in the first phase of the studies seem to support that: the new antibodies they formed after getting vaccinated appeared to neutralize lab-based versions of SARS-CoV-2. Buoyed by these early studies, Moderna began a study in June to identify the ideal dosage, and at the end of July it launched the final stage of testing, which will include 30,000 volunteers who will receive either that dose or a placebo.

The speed with which Moderna was able to develop and start testing was a tantalizing lesson in possibility for other vaccine developers. Major players in the pharmaceutical industry began prioritizing mRNA programs they had been developing with smaller biotech firms with expertise in the technology. For example, Pfizer, the New York–based pharma giant, took advantage of a two-year collaboration with German immunotherapy company BioNTech and, in April, poured $185 million into a joint effort to explore four potential mRNA-based vaccines. The two companies had been working on using mRNA to create a flu vaccine, and when COVID-19 struck, says Philip Dormitzer, vice president and chief scientific officer for viral vaccines at Pfizer, “it was relatively straightforward to swap out the influenza-coding antigens in the vaccine candidate and put in COVID-19 antigens instead.”
Such substitutions are one of the mRNA technology’s strongest features; rather than requiring copious amounts of live virus, all researchers need is the virus’s genetic sequence, which they can then edit to find the right code for antigens to alert the immune system of the virus’s intrusion. Pfizer and BioNTech scientists exploited this and quickly developed four promising candidates for testing; early studies identified one, containing the entire genetic sequence of the virus’s spike protein, as producing the fewest side effects with the most robust immune response. At the end of July, the companies started a combined Phase 2 and Phase 3 trial of this candidate with 30,000 people.
Pfizer isn’t the only company to fast-track stakes in the mRNA technology. In June, Sanofi increased its investment in Translate Bio, which could total up to $1.9 billion and give Sanofi access to the technology and manufacturing know-how to develop mRNA-based vaccines against infectious diseases—with COVID-19 the obvious priority. The companies are working on starting clinical trials in people sometime this year.
But while the mRNA platform may give vaccine makers a jump-start in development, more familiar vaccine approaches have well-established manufacturing and storage methods behind them. For one thing, mRNA is notoriously unstable and sensitive to temperature, so vaccines made with this technology need to be stored and shipped at anywhere from –94°F (–70°C) to –4°F (–20°C), far below temperatures required for most existing vaccines. That’s why companies like Sanofi, Johnson & Johnson and AstraZeneca are relying on their experience with another innovative but promising vaccine-making method to solve that problem—one that involves another virus.
Because viruses are adept at infecting cells, they can be a useful vehicle for transporting other viruses to prime the body’s immune cells, as long as they are disabled first. Drug companies are building and testing vaccines against Ebola, influenza and RSV, among others, by Trojan-horsing genetic material from one virus inside the shell of another that isn’t able to cause disease, but questions remain about how safe such double–virus vaccines might be.
At Johnson & Johnson, based in New Brunswick, N.J., scientists are counting on a weakened form of adenovirus, which is responsible for the common cold, to deliver COVID-19 material. Its team hopes that its shot, unlike many of the other COVID-19 vaccine candidates, will require just one dose. The company plans to test both single and double doses of its vaccine in beginning in September.
In the U.K., scientists at the University of Oxford are using a similar approach for their vaccine, which will be developed, manufactured and distributed by AstraZeneca. They inserted the genetic code for SARS-CoV-2’s spike protein into a weakened cold-virus vector that normally infects chimpanzees. The cold virus transports the viral genetic material to human cells and “infects” them in the same way SARS-CoV-2 would, and therefore prepares the immune system to attack it in much the same way a natural infection does. In early human studies, the vaccine produced good immune responses against SARS-CoV-2.
The Oxford-AstraZeneca team believes its manufacturing process for this sort of shot will make it easy to scale up production. “Hopefully, if it’s successful, this vaccine will be relatively inexpensive to make in terms of dollars per dose, and it’ll be relatively easy to do at scale,” says Mene Pangalos, executive vice president of bio-pharmaceutical research and development at AstraZeneca.
There may be a price for that manufacturing ease, though: relying on vectors like the one for the common cold can cause problems down the road. First, the exposure to two viruses, even if one is weakened, could trigger an excessive immune response that ends up causing more inflammation that could be harmful rather than helpful. Second, while cold viruses are, at first, adept at infecting cells, human immune systems are also adept at learning to rebuff them. So while a cold-virus-based vaccine may be effective at initially generating an immune response against SARS-CoV-2, if someone is exposed again, that immune response might not be as robust the second time. This is a real public-health concern, since most officials are bracing for a wave of new cases in the fall and winter when flu cases also peak.
The trial, which AstraZeneca was expanding to include 50,000 people in the U.S., U.K., Brazil and South Africa, is currently suspended as researchers investigate whether an illness experienced by one of the study volunteers is related to the vaccine. The unexplained illness was reported as part of routine safety monitoring done by independent review boards that are part of each major vaccine trial to ensure that the new vaccines don’t cause more harm than good.
Building on previous vaccine successes
In some ways, the pause in the trial may also serve as a testament to the value in sticking with more proven strategies that have a legacy of success. Researchers also know from experience that another gene-based approach, one that relies on DNA, can generate not only antibodies against a virus like SARS-CoV-2 but also T cells and B cells, which help the body establish a longer-lasting memory of previous infections and better prepare it to recognize and target viruses and bacteria should they invade again. While antibodies generated against SARS-CoV-2 proteins are likely to be an important ingredient in the ultimate alchemy of immunity, there are hints from recovered COVID-19 patients that those antibodies may not always be enough. Recent analysis of convalescent plasma from recovered COVID-19 patients in New York, for example, shows that their levels of antibodies vary widely and that most of these antibodies have only moderate powers to neutralize SARS-CoV-2, at least in the lab. In addition, some studies suggest that the level of antibodies can wane as quickly as three months after infection.
For a more durable and lasting protection against future infections, the body needs to enlist the help of its cell–mediated immune response, including T and B cells, which have the ability to remember, recognize and reactivate against previous foes. While Moderna has reported that its mRNA vaccine generated good T-cell responses, DNA-based vaccines against other diseases have already proven adept at this job.
In part, that’s what attracted Sanofi to partner with GlaxoSmithKline (GSK) for another potential COVID-19 shot called a recombinant protein-based vaccine. The approach involves taking the genetic code for parts of SARS-CoV-2’s spike protein and, in Sanofi’s and GSK’s case, inserting them into insect cells that then serve as the factory for producing the viral protein. Researchers then extract and purify this protein and combine it with a GSK compound that, when injected, prompts the human immune system to generate defenses, specifically antibodies, against it. It’s a reliable technique, and responsible for the HPV and hepatitis-B vaccines that were approved in 2006 and 1986, respectively. It’s also the technology that Sanofi uses to make Flublok, its influenza vaccine, which means that if its COVID-19 vaccine made with this method is safe and effective, the company could ramp up production quickly. The companies began human testing in September and anticipate providing up to 1 billion doses annually if their vaccine is effective. Australian scientists at Novavax are also using an insect-cell-based system to deliver the genetic code of the SARS-CoV-2 spike protein in its vaccine, and reported encouraging results in September.

Meanwhile, at Inovio, based in Pennsylvania, researchers have conducted studies on primates using an experimental DNA-based vaccine for MERS, and the results suggest that animals with strong T-cell responses were better able to neutralize the MERS virus. “I believe that the level of T-cell response is going to be very important in providing protection [against SARS-CoV-2],” says Dr. J. Joseph Kim, president and CEO of Inovio. The company vaccinated the first of 40 volunteers in a Phase 1 trial for its COVID-19 vaccine in April and reported in June, without providing deeper details, that 94% of participants generated an immune response. Inovio plans to continue testing its vaccine into the fall.
The next step: manufacturing and distribution
Even if vaccine manufacturers are able to find just the right viral sparks to catalyze an immune response against SARS-CoV-2, they face another, equally daunting task: manufacturing enough of these vaccines in a short amount of time to throw the brakes on the runaway pandemic. AstraZeneca’s CEO has pledged to produce 2 billion doses of the vaccine by year’s end—an ambitious timeline. But even typically circumspect experts note that there is a chance, however remote, that ongoing tests of the vaccines could show dramatic effectiveness and be stopped early, by the end of the year. Whether that’s possible will depend in large part on how widespread COVID-19 is as more of the vaccines reach the last stages of testing. Such studies are focused more on efficacy than on safety and require tens of thousands of participants. If there aren’t enough cases of COVID-19 still circulating by the time these final trials begin, scientists won’t have the statistical power they need to compare, among those exposed to the virus, the people who were vaccinated with those receiving a placebo, and quickly see if the vaccine is working.
Such was the fate of the SARS and MERS vaccine programs governments and pharmaceutical companies launched in 2003 and 2012, respectively. As soon as cases waned, the urgency for vaccines did as well, along with investments in research and testing. Some public-health experts believe that if that work had continued, what researchers would have learned about coronaviruses and how to protect against them might have given scientists a jump start on a vaccine against SARS-CoV-2.
To avoid losing that momentum again, some epidemiologists have floated the idea of intentionally infecting volunteers for COVID-19 vaccine trials. Known as “human-challenge” research, it’s a controversial strategy and has been done only with diseases like flu and malaria for which there are good safety-net treatments that people can take if they get severely ill after getting intentionally exposed to the disease. For now, the ethical questions such an approach raises aren’t urgent, as new hot spots continue to emerge around the world.
The bigger and more immediate problem, if vaccines are authorized, is how they will make it to the people who need them most. In the U.S., public-health systems are already overwhelmed with testing for cases and tracking the pandemic, and desperately need guidance “yesterday,” according to one state health official, on how to plan for a massive immunization campaign, how many doses they can expect and how they should decide who gets those first doses. “Our public-health system is highly fragmented, under-resourced, overlooked and underappreciated,” says Dr. Howard Koh, a professor at Harvard T.H. Chan School of Public Health and former assistant secretary for health and human services. “To make this happen, the local and state public-health infrastructure has got to be very strong, and right now it’s not.” The situation is similarly dire in lower-resource countries like India, where a lack of hospital beds and medical equipment amplifies the burden and toll of the disease.
No matter which vaccines are successful in trials, coverage will be key to achieving herd immunity. A linchpin of coverage is access, and access hinges on price. Moderna has said its vaccine will be priced depending on the volume of doses ordered, with smaller volumes costing at most around $32 to $37 per dose, while AstraZeneca says its collaborative vaccine with Oxford will be developed and distributed at cost to meet the needs in lower-resource countries. Ahead of final results from its trials, AstraZeneca signed agreements with companies in South Korea, Japan and Brazil to manufacture and provide up to 3 billion doses of its vaccine. “This isn’t about us winning and somebody else losing. It’s about us making a difference on this disease,” says Pangalos from AstraZeneca.
Even if the COVID-19 vaccines don’t provide 100% protection against infection, they could provide a huge boost toward that return to normality. But how quickly that happens will depend as much on the science behind them as on the humanity that determines where those vaccines go. What’s being tested is more than the new technologies and the latest virus-fighting strategies encased in each injection. It’s also our willingness to be blind to the physical as well as social and economic borders that divide us to combat a virus that holds no such biases. “With COVID-19, there is a chronic fear,” says Kelly. “To be relieved of that is so important. It’s so important to trust that the vaccine is going to help us have a healthier society that’s not fear-based, so we can enjoy our lives again.”
—With reporting by Ciara Nugent/London, Leslie Dickstein, Mariah Espada and Simmone Shah
Correction, Sept. 22
The original version of this story misstated the details of Edward Jenner’s work in developing the concepts behind virus vaccination. Jenner found that exposing people to small amounts of the cowpox virus could provide immunity to smallpox, a virus in the same family; he did not expose people to the smallpox virus itself.
More Must-Reads from TIME
- Where Trump 2.0 Will Differ From 1.0
- How Elon Musk Became a Kingmaker
- The Power—And Limits—of Peer Support
- The 100 Must-Read Books of 2024
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- FX’s Say Nothing Is the Must-Watch Political Thriller of 2024
- Merle Bombardieri Is Helping People Make the Baby Decision
Contact us at letters@time.com