In May 2020, Dr. Francis Collins, the longtime head of the National Institutes of Health (NIH), was called to the White House to meet with Jared Kushner, the then President’s son-in-law and adviser, and Dr. Deborah Birx, the head of the White House Coronavirus Task Force. A few weeks earlier, Congress had given the NIH $1.5 billion to try to speed up the process of developing new diagnostic tests for COVID-19, and the White House, which was dubious about increasing the rate of testing, wanted to know more about what the NIH was doing.
Collins is technically the boss of Dr. Anthony Fauci, but during the pandemic he has mostly taken a back seat to America’s most prominent epidemiologist when it comes to media. It’s not that Collins is not a great communicator; he’s known for his ability to talk about science at any level. But he did not wish to become an object of White House attention. So when he met with Kushner, “I did my best to try to describe what we were doing in a way that it wouldn’t attract a lot of desire on their part to interfere,” says Collins. “It was really technical and really geeky.”
In June, Kushner visited the NIH to hear about the new plan, known as RADx (Rapid Acceleration of Diagnostics), from other points of view. This time Collins’ engineering staff went into nerd-overdrive detail. “And that was the last we heard of White House interest in what we were doing for diagnostics,” says Collins. “To this day I have never done a briefing about RADx in the White House task force. And that was just fine.”
Collins believes in God and science, probably in that order, but in the past 12 months, science has been hogging his attention. (To get in time for prayer and Bible study, he says, he has been waking up before 4 a.m.) As the head of the U.S. government body responsible for funding biomedical research, he’s the guy who has to figure out where to put the considerable resources of the U.S. purse to most effectively keep Americans healthy. The NIH runs 27 agencies and funds tens of thousands of research projects in universities around the country. As far as health research is concerned, the buck starts with Collins.
Bureaucrats are hardly ever the heroes of stories. It is hard to extol the virtues of the person who, when faced with a looming societal problem, figures out which of the many processes and regulatory frameworks available to him or her is the appropriate place to start. We understand the appeal of the guy who reinvents the wheel. We get the triumph of she who surpasses overwhelming odds. But the soul who liaises with stakeholders, who wields acronym-laced organizational charts, who crafts carefully worded and completely understandable memos, who knows whom to contact for the details of another contact? That soul is hard to romanticize. Is there anything less cinematic than forming a committee and sending a punishing number of emails?
Collins is known, however, for having an unusual combination of abilities. He’s a well-respected scientist (he helped decode the human genome) as well as an impressive administrator (he has run the biggest biomedical funder in the world for 11 years and overseen a budget increase of 40% to, in 2020, $41.68 billion). “There’s not too many scientists that are very gifted at what they do in the laboratory and can do the kind of public articulation of science with politicians from across the political spectrum,” says Nobel laureate biochemist Jennifer Doudna. He’s also one of the few scientists who can speak credibly to people of faith, who in some circles have come to regard science as hostile to their beliefs.
Keeping exactly the right height of profile is one Collins’ less-appreciated talents, the kind that has kept him at the head of a government agency through three presidential administrations, including the current one, to which he was reappointed in January. Republican Congressman Tom Cole of Oklahoma calls him “the best politician in D.C.”
Collins has had to use every one of those abilities as he has tried to manipulate the levers of scientific mastery and money to confront the pandemic in the U.S. at a time of political instability. If Fauci and his team have been at the forefront of the fight against the coronavirus, Collins has been their staunchest supporter, championing Fauci as he kept hammering the scientific facts home, and creating battle plans that may become the blueprints for the way the U.S. addresses its most besetting diseases in the future. He’s drawn criticism for both his methods and his priorities, as well as his refusal to publicly challenge the Trump Administration, but his hope is that when COVID-19 is finally put in the column of things we know how to manage, alongside TB, measles and HIV, the U.S. will have a new set of tools and processes to more quickly mobilize around the next threat. “It would be really poor planning to imagine that this is the last coronavirus epidemic that we will ever see,” says Collins. “We need to be prepared for whatever COVID-24 is going to look like. And along the way we might even cure the common cold.”
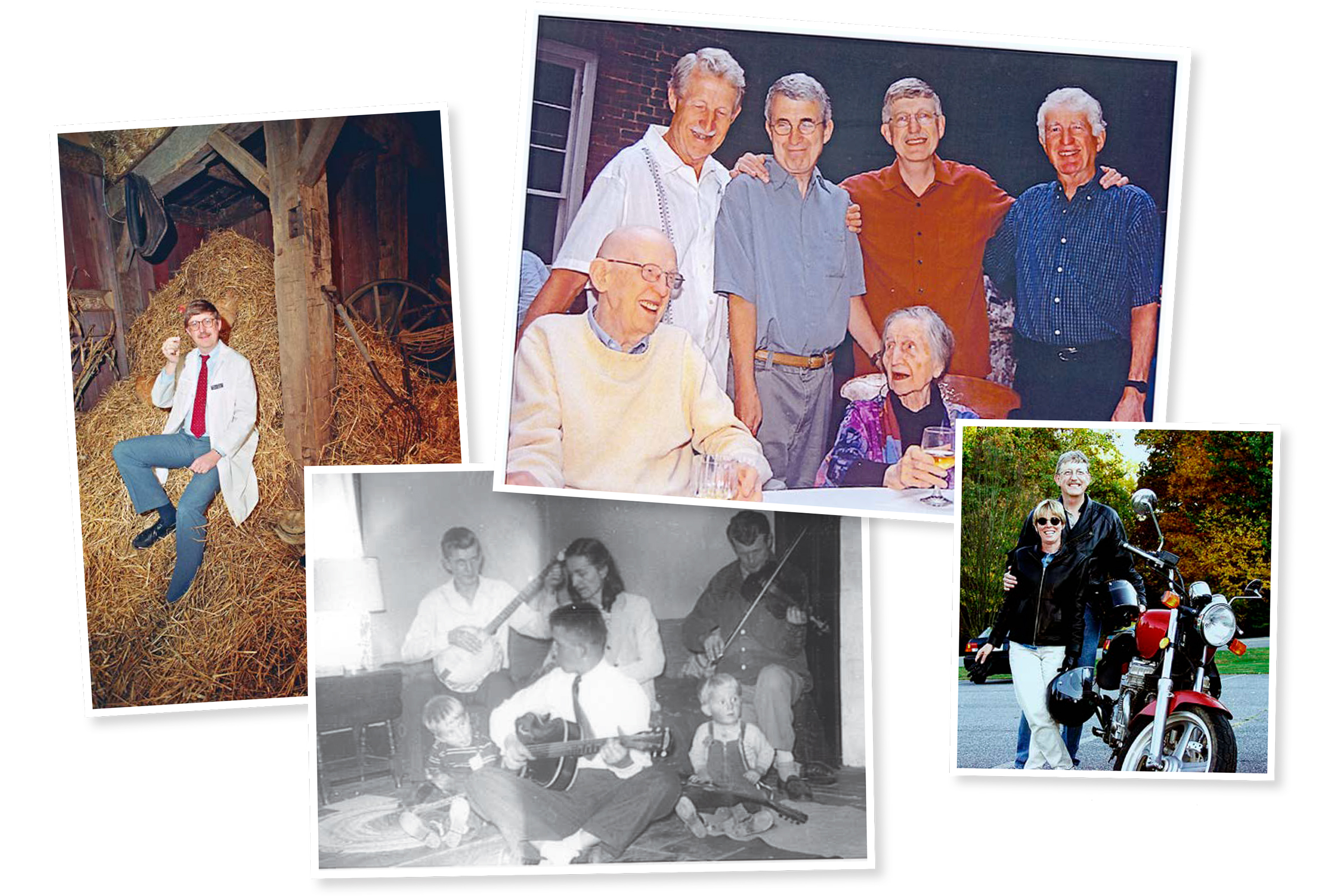
Collins, 70, had an unconventional upbringing for a scientist. His parents were theater people who lived in a farmhouse in Virginia’s Shenandoah Valley. His father, a drama professor, and his mother, a playwright, would put on performances in a grove of oak trees behind the house every summer, in which young Francis performed. Collins was homeschooled by his mother until sixth grade, and what she lacked in training she made up for in enthusiasm. “I learned to love the experience of learning new things,” says Collins. “That has served me very well as NIH director, and particularly well this year,” when he might have two days to make a decision about an area of science “that was not exactly my sweet spot.” Collins had to dive into studies on subjects like immunology that before the pandemic he confesses he regarded as a “little bit woolly.”
The theater training has helped him in other ways too. Collins can read a room and adjust his level of discourse according to his audience. For academics, he uses more pure science. For politicians, it’s all about clearly articulated deliverables. “Everyone on our health committee—and they’re 23 different members from Elizabeth Warren to Rand Paul—trusted him,” says former Republican Senator Lamar Alexander. “He has a very plainspoken way of talking about the medical miracles that could happen over the next eight to 10 years if we properly funded the work.”
There’s a folksiness to Collins, who has an old-fashioned and formal way of speaking, in perfectly grammatically correct sentences punctuated by an occasional “oh boy” or “by golly.” He looks like the kind of distinguished elderly gentleman that The Simpsons’ next-diddly-door neighbor Ned Flanders would grow into if cartoon characters aged. This geniality, however, does not mask his drive. Even during the pandemic, he still has a research lab with postdocs, and in November the FDA approved a drug for a premature aging condition known as progeria that was built on his research. He also plays guitar well enough to have at least once sat in at Nashville’s Bluebird Cafe, the jumping-off venue for such notables as Garth Brooks and Taylor Swift.
Despite the guitar chops, and his fondness for motorcycles, nobody is going to accuse Francis (never Frank) Collins of being anything but the squarest of the quadrilaterals. The hobbies are a way of disarming people. He often composes ditties to play at the farewell parties of staff members. At a meeting of the NIH advisory committee in 2020 (held online), he played guitar while the Gates Foundation’s Chris Karp played piano and sang a song about the virus to the tune of the Beatles’ “In My Life.” With this virus all around us, through the whole world, our lives have changed …
Collins studied chemistry at University of Virginia and did a Ph.D. at Yale before switching lanes to medicine and landing in the then nascent field of genetic decoding in the early ’80s. He developed an innovative method of gene finding, which led to the identification of the genetic sequences responsible for cystic fibrosis, Huntington’s disease and neurofibromatosis, among others. In 1993, he was asked to lead the government group that contributed to the Human Genome Project, creating a map of the 3 billion DNA base pairs that make humans human.
After he was made NIH director in 2009, he set about making the agency more focused on translational science—finding ways to convert scientific discoveries into medical advances. When Collins submitted his resignation letter to President Trump, as the NIH director generally does for each Administration, he got a one-line email stating that it was rejected. “He is my nominee for Most Unsung Valuable Player in health care during the last dozen years,” says Alexander, who advocated for the Trump Administration to make him one of the few Obama-era appointees who kept his job.
It may have been hydroxychloroquine that set Collins on the path he’s taken during the pandemic. Trump was touting its efficacy in March, based on a small French study later more or less disowned by the scientific journal in which it appeared, and what the then President said was “a feeling.” “I was frustrated, as was anybody in the scientific community, about the ways at times that science was neglected or overshadowed by political comments or just personal anecdotes,” Collins says.
Before he was a research scientist, Collins was a physician, and so as the need for COVID-19 treatments became more urgent, he diagnosed the country as in need of some scientific rigor. “It looked as if there were hundreds of trials on hydroxychloroquine, most of which were probably too small to give you a credible result,” he says. “And there were lots of other very small trials on compounds that people thought, ‘Well, maybe that will work,’ but there was relatively little in the way of systematic evidence and there was no prioritization going on.”
Over the next few weeks, Collins contacted the chief scientific officers of many of the pharmaceutical companies and began to float the idea of creating an emergency public-private partnership, like the ones that had been first created for HIV, then cancer, and were bubbling along for such diseases as diabetes and lupus, but bigger and faster. This network, which came to be called ACTIV (Accelerating COVID-19 Therapeutic Interventions and Vaccines), aimed to streamline and bring discipline to the creation of treatments and vaccines for the virus. “It seemed like what we really needed to do was to get the academics and the government and industry all together and decide we’re going to do something that we’ve never quite done before in a crisis like this, and that is prioritize what needs to be done and then do it and not worry about who’s going to get the credit.”
Mikael Dolsten, chief scientific officer of Pfizer, got a call about it while his wife was in the hospital with COVID-19. Even though Pfizer was going to run its own Phase 3 vaccine trials outside of the Collins plan, he encouraged his longtime friend to do it, he sat on the executive committee and another Pfizer executive co-headed the vaccines working group. “Francis really brought the world of academia together to seriously look at how you do best practice for COVID pandemics,” says Dolsten.


On April 4, nine pharmaceutical companies—including Moderna, which was the second drugmaker to get emergency-use authorization from the FDA for its vaccine, and Johnson & Johnson, which hopes to apply for it soon—and five government agencies met to hash out the details. Within two weeks, they had mapped out the four areas that needed the most intense effort and set up teams for them all, each led by a representative of industry and of either academia or the government. “We had a hundred people who basically agreed they’re going to put their lives on hold for everything except this,” says Collins.
One of the groups worked on the vaccine, ensuring the trials were efficient while also being rigorous. It was decided, for example, that each trial needed to have at least 30,000 participants and they would be observed for negative side effects for at least 60 days. The same data-safety board monitored all of the trials from the different vaccine makers, so the standards for measuring safety and efficacy were consistent.
Another group was looking at possible treatments, both existing medicines that might be adapted and new approaches that could be supercharged with funding. That group also had to establish the protocols for all the drug development. Dolsten says Pfizer is considering collaborating with the network on its antiviral treatments. “We have never run an antivirals study against coronavirus,” he says. “The spirit of ACTIV and what we have learned from all the trials now will be invaluable.”
The third group was tasked with figuring out how to do the staggering amount of testing it would take to get these drugs and vaccines to market, including finding specialized labs, technicians, volunteers and equipment. “You needed very quickly to set up clinical trial networks that can enroll thousands of people,” says Collins, “and we don’t have that capacity ready to go unless you pull things together including networks that haven’t worked on infectious disease before.”
The fourth group was a kind of advance guard, which gathered and disseminated all the information that the other groups would need to get going before human trials began: any animal studies that had been done, how to gain access to the right sort of laboratories—those that can work with highly contagious viruses—and making sure the laboratories had cleared their decks and were ready to go.
While all this was under way, there was still the problem of diagnostic testing. You can’t fight a virus if you don’t know who has it. RADx required Collins and his colleagues to add a new skill set to their résumés: venture capitalist. At the time, the U.S. was performing about 150,000 tests a day; to effectively monitor the population for the virus, the NIH estimated it would need 6 million.
Collins dispatched Bruce Tromberg, director of the National Institute of Biomedical Imaging and Bioengineering (NIBIB), to help lure in businesses, tech companies and academic labs, and they created a kind of Shark Tank where those with ideas would get speedily reviewed by a team of experts, who would evaluate not just the science but also their capacity to scale it. Those candidates spent a week in virtual intensive collaboration with industry experts, who tweaked and refined their innovations. Other projects that were further along were given an influx of cash.
“Within eight months they attracted proposals from 700 different people and pushed two dozen of them into the marketplace,” says Alexander, who was one of the champions of the project when the White House was skeptical about the benefits of testing. “That’s an incredible engineering and scientific achievement.” The first over-the-counter home test approved by the FDA, from Ellume, was developed using that process.
Has it been enough? Not nearly. Collins wishes he had included convalescent-plasma studies in ACTIV, to clarify if the blood of people who had recovered from COVID-19 could help those struggling with it. “I take that as a failure of our whole academic clinical research effort, and a failure of NIH, that we didn’t jump in and make sure that this was organized in a fashion that would give a rigorous answer,” he says. “It may help most with people who just got infected who haven’t made their own antibodies yet, but we don’t know for sure.” And there is only one FDA-approved COVID-19 medication, remdesivir— a repurposed Ebola drug. That’s not surprising to Collins—it takes three to five years to develop a new antiviral drug—but it still haunts him. “I think we have actually moved at unprecedented speed in everything we’ve done,” he says, “but I’ve still felt this sense every day that people are losing their lives as a result of this, and I wish we could have gone faster.”


Collins came to faith during the period when he worked as a physician. He noticed how many gravely ill people seemed to draw strength from their beliefs, and when one patient eventually asked him what he believed, he was disturbed that he didn’t have an answer. “Atheism for a scientist is really hard to defend because it’s the assertion of a universal negative,” he says. “And scientists aren’t supposed to be able to do that.” A minister directed him to every brainiac Christian’s favorite writer, C.S. Lewis. Eventually, Collins wrote a best-selling book of his own, The Language of God, in which he uses scientific phenomena as evidence of a Deity. In 2020, he won the $1.3 million Templeton Prize, which is given to those who investigate the metaphysical aspects of science.
One standing appointment Collins has kept during the pandemic is with his book club, made up mostly of members of the Christiantelligentsia. Theologians such as Russell Moore and Tim Keller, columnists such as Pete Wehner and David Brooks and the conservative author Yuval Levin meet monthly, usually to discuss books about weighty matters of faith. The theologian N.T. Wright, who’s also a friend of Collins’, visits when he has a new book out.
While Fauci has been medicine’s public face, Collins has been hitting the faith-based circuit, toting his “favorite pet rock,” a baseball-size 3-D printed model of a spiked protein, and preaching science to believers. One of his life goals is to address the “long-standing tension between evangelicals and rigorous science.” He insists that for a believer, science is a form of worship. “It’s a glimpse of God’s mind,” he says, “when you do a scientific experiment.” His foundation, BioLogos, tries to bridge the two. The pandemic has shown how much work it has to do.
For all Collins’ accomplishments and accolades—including the Presidential Medal of Freedom in 2007 and the National Medal of Science in 2008—he is not immune from criticism. “What I think was disappointing is that science leaders did not step up to challenge the President more publicly,” says Lancet editor in chief Richard Horton. “The failure of the science community to act more robustly led to a collusion between scientists and politicians, a collusion that has needlessly cost the lives of hundreds of thousands.” Collins says Fauci did a better job at speaking out about this than anyone could and didn’t need anyone else to speak for him.
Under Collins’ watch, the NIH has established the position of Chief Officer for Scientific Workforce Diversity and invested in outreach to underrepresented communities in science, yet a recently published analysis by two researchers argues that the NIH’s own studies show little improvement has been made in funding bias. “What I’d blame Francis Collins for is his lack of taking [the NIH studies] seriously,” says professor Michael Taffe of the University of California, San Diego, psychiatry department, one of the authors of the paper. Not only does the NIH fund proportionally fewer Black-led research projects, the study suggests, but it funds fewer projects that look at health issues that are more likely to affect Black communities. “Everything that’s not majoritarian culture is secondary,” says Taffe.
“I will be the first to say we have failed for the most part to have our workforce look like our country,” says Collins. With the lifting of Trump’s Executive Order banning training on structural racism in government agencies, he says he hopes as soon as February to begin meetings on the series of actions the NIH will be taking to address the imbalance.
The bigger problem, he says, is the racial disparities in the health of Americans. The coronavirus threw those into sharp relief. It was clear early on that people from underserved neighborhoods and communities of color were infected by the virus at a much higher rate and were more likely to be hospitalized and to die of it than those in wealthier and white communities. Collins notes that as a geneticist, he knew this had nothing to do with biology. So the NIH undertook a bunch of programs to redress the balance, including trying to figure out how to get more tests into minority communities, ensure that vaccine trials were testing as representative a cross section of the country as possible and, once the vaccines were approved, make them available and welcome in every neighborhood.
Given the history of medical interventions into communities of color, the NIH decided it needed to be proactive about building trust and communication before the vaccines arrived. Dr. Gary Gibbons, the director of the National Heart, Lung and Blood Institute at the NIH, co-led an initiative called CEAL (Community Engagement Alliance), which built relationships and networks in minority communities to both hear their concerns and try to address misinformation about the vaccine and encourage participation in trials. “The NIH overall makes quite an investment in health-disparities research,” says Gibbons, “but it’s a work in progress.” Initial figures suggest that Black Americans are getting vaccinated at much lower levels than white Americans.
Taffe’s solution for the disparity within NIH—to fund a more diverse range of scientists—is echoed in other corners of academia. Because Collins has always favored big, bold plans, like curing diabetes or Alzheimer’s, some scientists say he overlooks the key ingredient for breakthroughs, which is funding innovative scientists. “He’s moved increasingly toward a command-and-control kind of model for science, specifying more than I think is healthy for the community what people are going to work on what kind of projects,” says Michael Eisen, a professor of genetics, genomics and development at the University of California, Berkeley. “It’s sucked the lifeblood out of American science in the process.” Eisen argues that the emphasis on moon shots erodes the foundation that makes those advances possible, which is long-term stable support of pure research.
Collins expresses a rare hint of impatience about these criticisms. “The vast majority of what NIH is doing is not those large-scale projects,” he says. “They get attention because if they achieve something they tend to make a splash.” He also points out that there are simply many projects, like his own Genome Project, that a single investigator could not take on. Currently about 1 in 5 projects submitted to the NIH gets funding. If he wasn’t able to sell Congress on those moon shots, the NIH would receive less money overall, he suggests, and that number would surely go down.

The catastrophic events of the past year have not shaken Collins’ beliefs. The wall next to the desk that he has rarely left is peppered with verses, and he has been hitting the Psalms pretty heavily. “As a Christian I don’t have to explain to God that suffering is a terrible thing because the God I worship suffered on a cross,” he says. But they have shaken his belief in some of his fellow Christians, who have insisted the virus is a hoax designed to take away their religious liberty. “It’s a source of great heartache for me as a person of faith to see in a circumstance where I would have hoped that people of faith would be rushing to try to help, that some of them seem to have adopted views that are actually accomplishing the opposite,” he says. “People are dying because of our failure in this country to effectively utilize proven methods of stopping the spread of the disease, particularly mask wearing and not gathering in large crowds indoors.”
He is, however, optimistic about the moves the new Administration has made so far. “All of the efforts that relate to COVID have been much appreciated,” he says. “The requirement of masks in federal facilities and airports is long overdue.”
In bringing together the medical resources of the U.S. to fight COVID-19, Collins and his partners may have established a new route to treating all sorts of diseases. It’s not that the NIH had never thought of any of these ideas before. It built RADx on an existing program within the NIBIB. The ACTIV network is the latest iteration in a decades-long series of collaborations. But the pandemic supersized the idea, and in the process made clear what was possible. “We have to plan ahead and be ready for this sort of family of viruses that we think might be the next big one,” he says.
Collins toys with the idea of leaving public service and returning to his other skill, working in a lab, but it seems obvious he’s not fooling even himself. “Overall, 2020 was a terrible year for our planet,” he said from his book-lined Chevy Chase, Md., office on New Year’s Eve. “It’s been a terrible year for our country. It’s been a tragic year for those people who lost their lives. But for science it’s been a phenomenal year of doing things.” The lab can probably wait.
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com
