When it comes to a disease as complex as Alzheimer’s, scientists have found a number of factors that can contribute to your risk, from genes to circulatory issues, inflammation, and lifestyle behaviors.
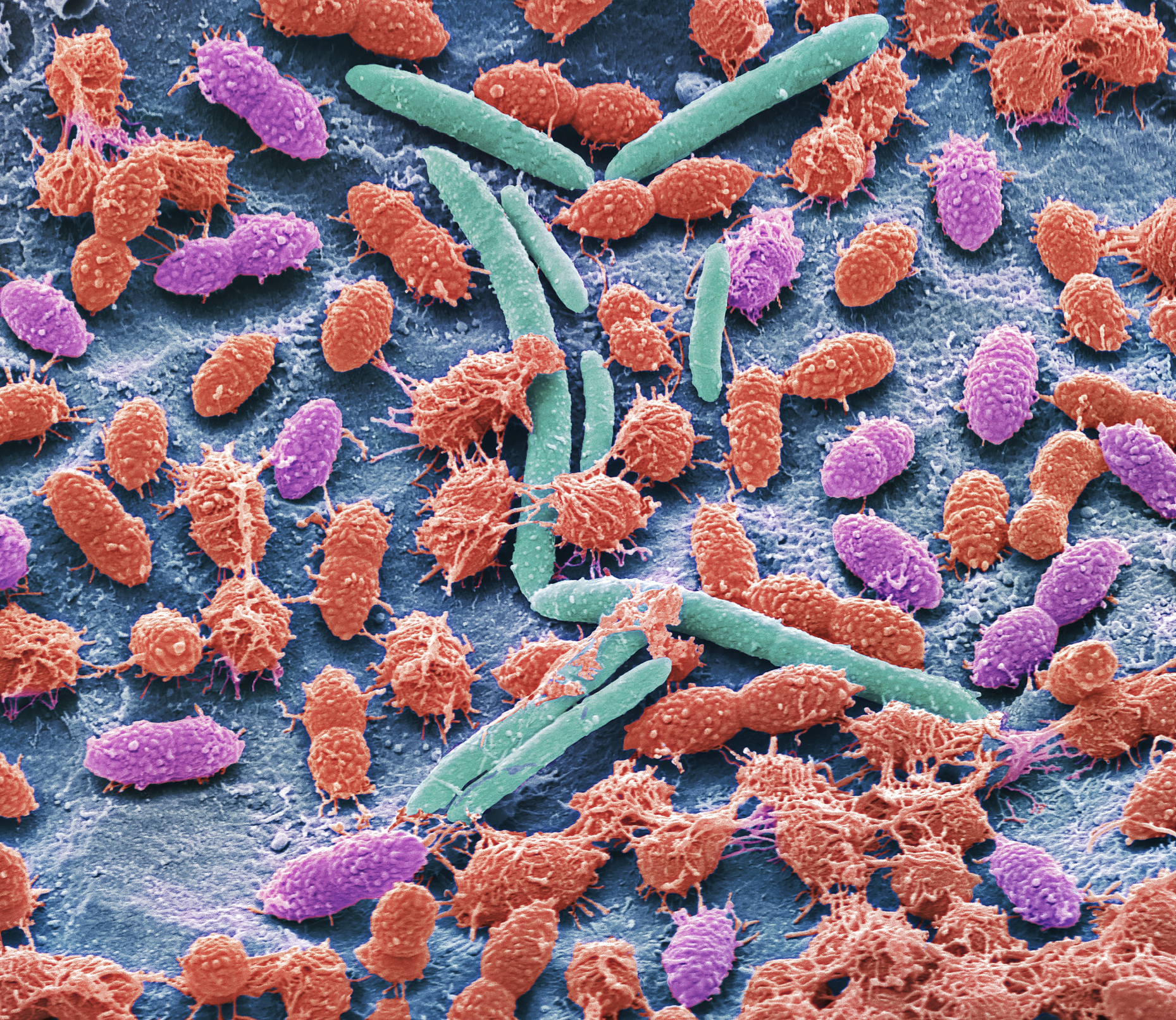
In a new study published in Science Translational Medicine, researchers from Washington University in St. Louis report on another possible factor: the types of bacteria living in the gut. Experiencing changes in gut bacteria populations may be an early marker for developing the disease, the scientists found. These differences can often begin years before the first symptoms of cognitive decline, such as memory loss and confusion, appear.
The study involved 164 older people, from ages 68 to 94, who were tested for the presence of the Alzheimer’s proteins amyloid and tau in their brains. Participants also completed cognitive tests so that the researchers could identify people with preclinical Alzheimer’s: those who did not yet show signs of cognitive decline but did have signs of amyloid or tau. Using fecal samples, the scientists then compared the bacteria found in the guts of the 49 preclinical Alzheimer’s patients to people who did not have signs of the Alzheimer’s proteins to see if their microbiomes were different.
More from TIME
“We were starting to see changes in different organisms in people with preclinical Alzheimer’s,” says Dr. Beau Ances, professor of neurology at Washington University in St. Louis and one of the co-authors of the paper. “This finding is important because it might lead to different interventions that could be done to alter the gut microbiome that affects Alzheimer’s risk.”
People in the preclinical stages of Alzheimer’s tended to have higher populations of bacteria involved in breaking down arginine and ornithine—two amino acids that are involved in protein buildup—while those without preclinical Alzheimer’s tended to have more bacteria involved in glutamate degradation, which may protect neurons. To test how powerful or useful these changes in the gut microbiome could be in detecting preclinical Alzheimer’s, the team then created different models including existing risk factors, such as family history of the disease, age, diabetes, brain images, and genetics to see if the information about the microbiome increased the ability of those factors to accurately predict who was in the early stages of the disease and who was not. Adding the information on the gut microbiome, says Ances, “led to pretty good sensitivity and specificity for predicting preclinical Alzheimer’s.”
Ances says the stool samples could provide yet another important piece of data in triaging Alzheimer’s patients in the future. “It’s like looking at an elephant: if one person sees the trunk, and one person sees the leg, and another person sees the tusk, if you take all of that information together, then you can say with more certainty that what you’re looking at is an elephant—or in this case, that the person might have Alzheimer’s.”
Read More: Eli Lilly’s Alzheimer’s Drug Shows Greatest Benefit Yet
Finding a connection between the gut and the brain isn’t too surprising, as previous research has suggested the two organs may interact. Previous studies of people with more advanced Alzheimer’s, for example, showed that their guts contained higher ratios of bacteria called Bacteroidetes, which are known primarily for their ability to fight off other pathogens, compared to a type called Firmicutes which are associated with obesity and diabetes. Ances says his study did not find a similar difference in this ratio, but that may be because his study is sampling people from a much earlier stage of disease, and that particular change in the microbiome may not happen until more neurodegeneration occurs. Other evidence implicating the gut in Alzheimer’s comes from animal studies; changing the composition of the gut bacteria reduced the amount of amyloid in the brains of animals.
Additional studies inspired by these results could also shed light on how the gut affects the brain when it comes to Alzheimer’s risk. Ances suspects it may have to do with inflammation in the gut, promoted by certain species of bacteria, that lead to broader changes in the inflammatory response that also affects the brain. “The gut-brain axis is mysterious right now,” says Aura Ferreiro, the study’s first author who was a postdoctoral fellow at Washington University in St. Louis while the trial was conducted, and is now R&D director at Tiny Health, a company that provides at-home gut tests for moms and babies. “We hope this study encourages people to keep studying how the two interact.”
The next step in confirming these findings is to take fecal samples containing bacteria from people with no amyloid or tau in their brains and transplant them in animals who do have these protein buildups, to see how much the microbiome can change the progression of disease.
The researchers also plan to continue following participants with preclinical disease, analyzing their stool samples every two years or so to track changes in their microbiomes along with any progression of Alzheimer’s symptoms. Those studies could eventually lead to adding stool samples to the suite of tests used to identify people with early Alzheimer’s and guiding them toward appropriate treatments such as the newly approved drugs that target amyloid in the brain. “If these results are validated, then we could consider a future where someone gets a routine gut test, their doctor tells them their microbiome looks like that of someone who might have preclinical Alzheimer’s disease, and then they are followed up with more established tests for the disease [such as PET imaging for amyloid or tau],” says Ferreiro.
She and Ances say it’s important to develop more accessible and inexpensive ways to identify Alzheimer’s patients earlier in their disease, since evidence shows that intervening early may slow the progression of the disease and buy patients precious months and even years in a cognitively functional state where they can remain independent and perform the tasks of daily life. While brain images using PET technology can detect the presence of amyloid and tau in the brain and diagnose the disease, these services cost $5,000 to $7,000, and Medicare currently only covers one PET amyloid per lifetime for patients enrolled in a clinical trial researching new Alzheimer’s treatments.
“We need more tests to identify people with preclinical Alzheimer’s,” says Ances. “If we could look at stool samples, staging people would become much more accessible to the masses compared to some of the techniques currently out there.”
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com