When it comes to avoiding COVID-19 in the U.S., it’s increasingly everyone for themselves. The Biden Administration announced it will end pandemic emergency declarations in May 2023, which will affect the availability of free tests, treatments, and vaccines.
But even now, nobody has fewer tools to protect themselves than immunocompromised people.
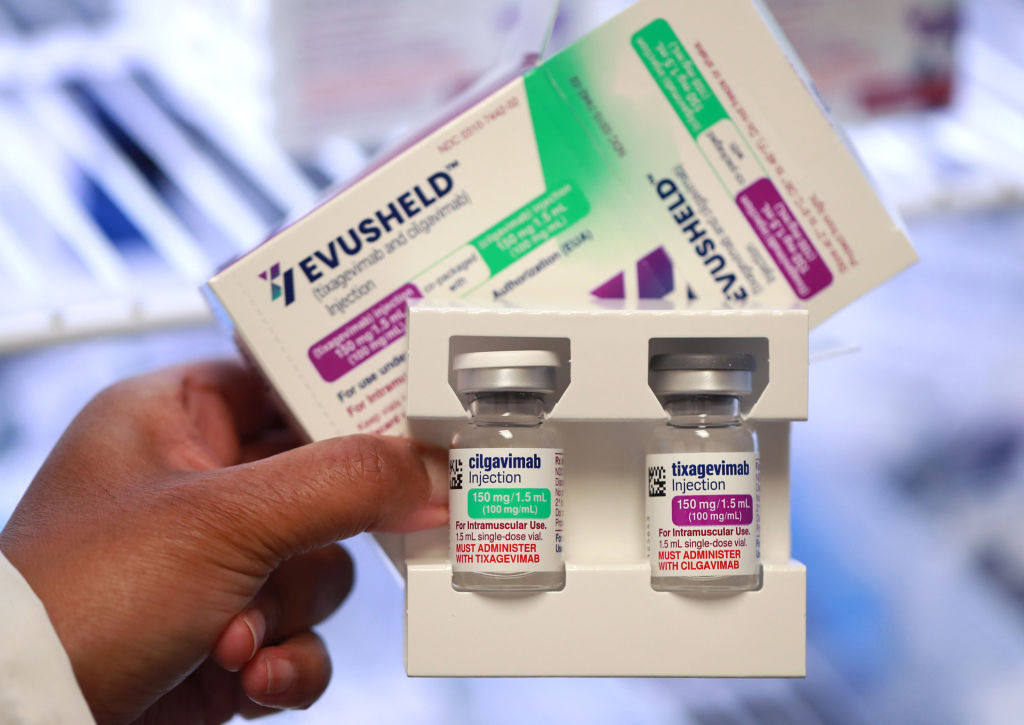
On Jan. 26, the U.S. Food and Drug Administration (FDA) revoked emergency-use authorization for Evusheld, a therapy first authorized in December 2021. Evusheld was meant to be used preventatively as an alternative to COVID-19 vaccines for people have a medical reason not to get the shots, or who are immunocompromised and do not mount strong immune responses after being vaccinated. But the therapy—a monoclonal antibody, or a lab-made protein meant to mimic the immune system’s natural response to the virus—has waned in efficacy as the virus has mutated.
The FDA pulled Evusheld’s authorization after concluding that it isn’t effective against the newer circulating variants. It could be re-authorized if it’s shown to be effective against future variants. But for now, one of the only COVID-19-prevention tools meant for the roughly 3% of Americans who are immunocompromised—albeit one that was never widely used—is off the table. “Immunocompromised Americans are screwed,” says Matthew Cortland, a senior fellow at the progressive think tank Data for Progress whose work focuses on disability, and who is immunocompromised.
AstraZeneca, the pharmaceutical company that makes Evusheld, is currently testing a new version of the therapy that is meant to work across viral strains, but there’s no way to know yet if it works or when or if it will be available to patients, says Erin McCreary, director of infectious diseases improvement and clinical research innovation at the University of Pittsburgh Medical Center.
Evusheld’s demise is “devastating to these patients,” McCreary says. “It made them more comfortable doing daily tasks and going out into the world to run errands and going out to dinner with their friends.”
Read More: It Isn’t Just Long COVID. Post-Viral Illnesses Are More Common Than You Think
Now, many people who are not well-protected by vaccines are in a dangerous and isolating situation—especially because the arsenal of effective COVID-19 treatments is shrinking for everyone as the virus evolves. In recent months, the FDA also pulled authorization for monoclonal antibodies that were used as treatments. Antiviral drugs including Paxlovid and remdesivir are still available, and research suggests that antivirals can help prevent hospitalization and severe disease among immunocompromised people. But “it’s really sad” to see the array of treatment options get smaller, McCreary says.
Following the Evusheld decision, the U.S. Centers for Disease Control and Prevention (CDC) recommended that immunocompromised people abide by old guidance: staying up-to-date on vaccines, masking, social distancing, and seeking out well-ventilated or outdoor areas. But to some people, those tips are a poor replacement for effective preventive therapies.
“Basically they have nothing to offer,” says Dr. Eric Topol, founder of the Scripps Research Translational Institute. “They should be honest and say there’s a hole in supporting people who are immunocompromised now.”
Topol and his colleagues recently launched a study that provides immunocompromised people with access to at-home tests, telemedicine services, and antiviral drugs if they test positive. In addition to gathering data about disease outcomes among immunocompromised people, Topol hopes the program will help prevent serious cases. Still, he’s disheartened that the federal government hasn’t undertaken similar efforts and isn’t pushing harder for the development of new monoclonal antibodies that work against newer strains. Without that push, he says, pharmaceutical companies have little incentive to do the work themselves.
Cortland called the CDC’s guidance “pathetic” and an “abject failure,” arguing that it does little to protect immunocompromised people in a country without adequate systemic COVID-19 mitigation measures. (CDC representatives did not respond to TIME’s comment request before publication.)
Now that most mask mandates are gone, less than half of American adults had worn a mask in the three months leading up to January 2023, according to Harris Poll data collected for TIME. While wearing a high-quality mask does help reduce the risk of infection for the wearer, it’s not as protective as if everyone in a space were wearing one. There are also aren’t enforceable ventilation requirements in most public spaces.
There is some hope on the horizon, Cortland says. The Occupational Health and Safety Administration is working on permanent COVID-19 safety standards for health-care facilities. And some drug makers are testing new therapies that may benefit immunocompromised patients. In addition to the potential updated version of Evusheld, a small number of new monoclonal antibody treatments are in development, as is a vaccine that may better protect people who don’t respond to the currently available ones.
But for the moment, immunocompromised people are essentially on their own. “Immunocompromised Americans have been forgotten and ignored,” Cortland says. “We have been left behind.”
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Write to Jamie Ducharme at jamie.ducharme@time.com