Toward the end of the 19th century, a New York City surgeon named Dr. William Coley purposely injected one of his patients with streptococcal bacteria. Coley wasn’t crazy. He hoped the bacterial infection would stimulate an immune response that would slow the spread of his patient’s cancer, which was inoperable. The experiment worked; the patient’s tumor shrank.
For the next 40 years, Coley and his research collaborators would test similar remedies on more than 1,000 cancer patients. They had failures but also many successes, especially among people with bone or soft-tissue cancers. Today, Coley is sometimes called the father of immunotherapy, which is a branch of medicine that attempts to activate or modify a person’s immune system in ways that help treat disease.
Cancer remains one of the most active areas of immunotherapy research, and people with bladder cancer are among those who stand to benefit most from these medicines. “Bladder cancer is one of the cancers—along with melanoma, head and neck cancers, and kidney cancer—that are highly responsive to immunotherapy,” says Dr. Joaquin Bellmunt, director of the Bladder Cancer Program at the Harvard-affiliated Beth Israel Deaconess Medical Center in Boston.
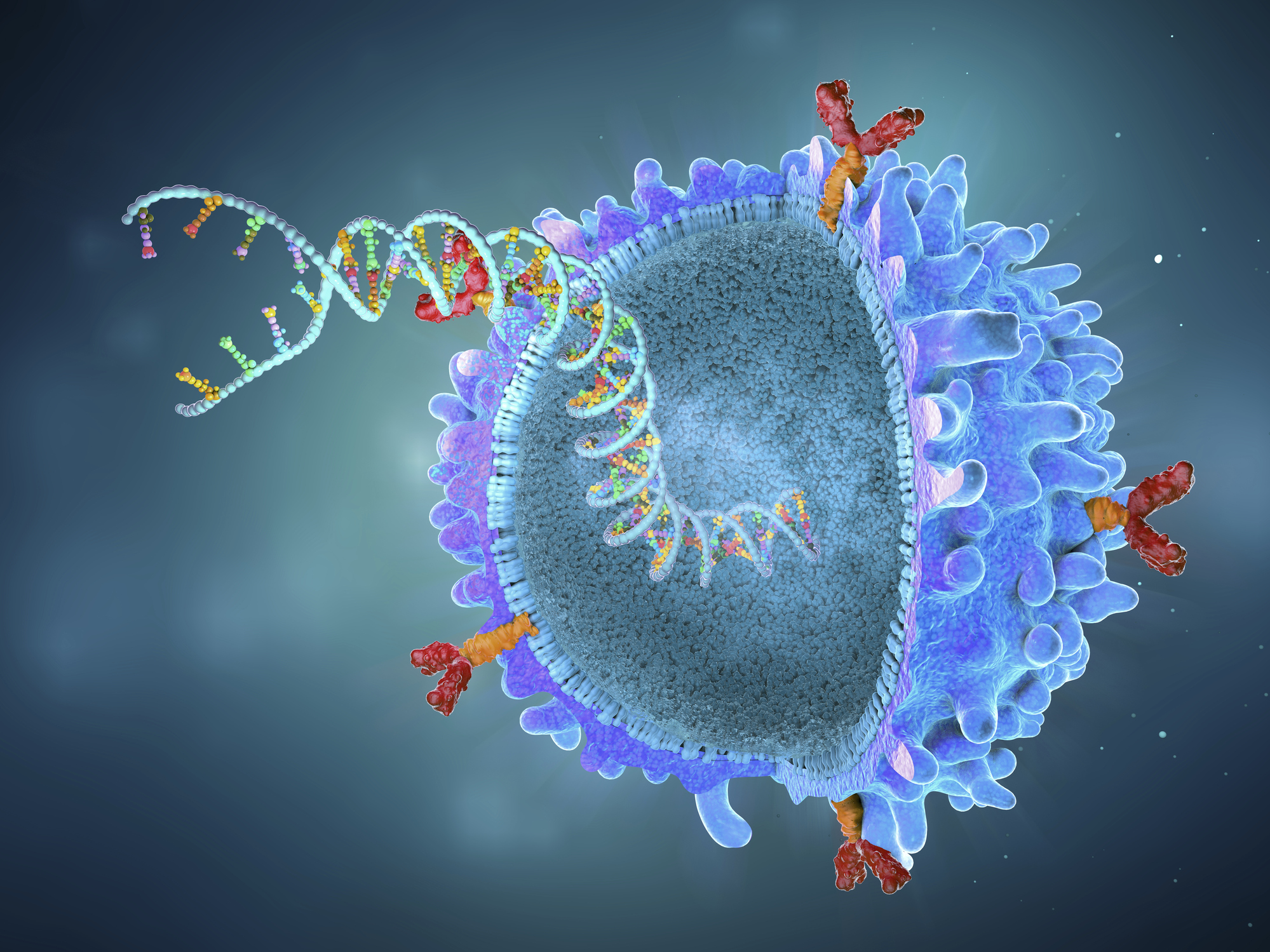
Bellmunt says that bladder cancer is characterized by a high number of tumor mutations. The human body tends to regard these sorts of mutations as “antigens”—meaning unwelcome threats that would normally instigate an immune response. However, cancer cells have features that allow their mutations to fly under the radar and evade the immune system’s antibodies. Immunotherapies work in part by counteracting these defenses. In Bellmunt’s words, they “release the brakes” that prevent the immune system from launching a more formidable attack.
Any discussion of new treatments for bladder cancer must highlight the newest immunotherapies, which have been game changers. But experts say that other recent advancements—including refinements in chemotherapies, radiation treatments, and surgery—are improving prognoses for people diagnosed with bladder cancer.
Here, oncologists and other bladder-cancer specialists describe the newest breakthroughs, as well as areas of research that could yield greater improvements in the future.
The latest in immunotherapy
Immunotherapy for the treatment of bladder cancer is not new. Since the 1970s, doctors following closely in Coley’s footsteps have given some bladder-cancer patients injections of bacillus Calmette–Guérin, or BCG, a bacteria that triggers a helpful kind of inflammation. “BCG has been standard treatment for non-invasive bladder cancers”—meaning early-stage cancers that have not spread beyond the bladder—“for the last 40 years,” Bellmunt says. “But when BCG failed, we had nothing left but cystectomy,” or bladder removal surgery.”
The situation was much the same for people with advanced bladder cancers that had metastasized to other parts of the body. If chemotherapy didn’t work, there were few alternatives. (Even when these therapies do work, the median survival time tends to be measured in months, not years.)
The newest immunotherapies are helping rewrite the script for people with both early-stage and later-stage bladder cancers. “2016 is the year the newer immunotherapies show up, and immediately some of these drugs were conditionally approved based on Phase 1 and 2 trials,” Bellmunt says.
Many of these relatively new immunotherapies are known as checkpoint inhibitors. They prevent (or inhibit) the action of certain immune pathways that would otherwise block a more robust immune response. Also known as anti-PD-1 or anti-PD-L1 drugs, these medications have “changed the treatment landscape” for people with advanced bladder cancers, according to a 2020 study in the New England Journal of Medicine (NEJM).
“With immunotherapy, if you actually look at the overall benefits, it’s pretty modest,” says Dr. Simon Crabb, a bladder-cancer specialist and associate professor in medical oncology at the University of Southampton in the U.K. To his point, that 2020 NEJM study found that, compared with standard treatment (like chemotherapy), immunotherapy lengthened average overall survival duration by about seven months. “But in a minority of patients, maybe 20% to 30%, you see exceptional responses,” Crabb says. “I’ve got people who’ve been on these drugs for four or five years.”
Figuring out why this happens—why some respond so much better than others to immunotherapy—is a focal point of current research efforts. “Something we’ve come to understand is that this isn’t one disease, it’s a subset of diseases that can be divided up based on genetic subtypes,” he explains. By mapping the genetic characteristics of different bladder cancers, experts hope to gain a -stronger understanding of how each responds to the current therapies—whether that involves a single immunotherapy medication or, as is becoming more common, immunotherapies mixed with chemotherapies or other drugs.
Researchers are also actively exploring the use of immunotherapies in earlier-stage bladder cancers. For example, there’s some hope that administering these drugs before bladder-removal surgery may be beneficial. “A long time ago, we found out that you can improve survival by giving chemotherapy before surgery, but it’s quite toxic,” says Dr. Yair Lotan, chief of urologic oncology at UT Southwestern Medical Center at Dallas. “Now we’re looking at using immunotherapy, or a combination of immunotherapy with targeted therapies, to avoid the need for systemic chemotherapy.”
Immunotherapies, like all drugs, have their downsides. The side-effects of the treatment can be hard to predict. “If the immune system is overstimulated, almost any organ system can be impacted,” Bellmunt says. Skin reactions—dry or itchy skin, rashes—are the most common complaint among people on these drugs. A smaller percentage of patients, 5% or less, develop inflammation of the bowels, lungs, or thyroid. This inflammation can cause symptoms like diarrhea, shortness of breath, or weight gain. “In rare cases we’ve even seen cardiovascular toxicity where patients developed myocarditis [heart inflammation] and died,” he says. Here again, researchers are working to better understand—and better predict-—how a person will respond to these treatments.
While plenty of work remains, these drugs have provided a life-saving step forward for some. “Once you boost the immune system, there are patients whose immunologic memory prevents the tumor from recurring,” Bellmunt says. “These patients have a clear improvement in survival.”
Read More: Changing Cancer Care, So Patients No Longer Feel Like a Number
New improvements in targeted therapies
Despite the excitement and advancements involving immunotherapies, chemotherapy remains the first-line treatment for advanced bladder cancers. There, too, medical researchers are making progress.
The cells of bladder-cancer tumors contain a high number of surface antigens, which are molecules capable of triggering an immune response. These antigens are the reason immunotherapies can be effective for the treatment of bladder cancer, and these antigens also assist the action of newer chemotherapy medicines known as antibody-drug conjugates. “These drugs use these quite clever molecules that have an antibody on one end—something that will hopefully bind onto the antigens on cancer cells in a selective manner—and a chemotherapy agent on the other,” Crabb says.
The big problem with conventional chemotherapy, he explains, is that it struggles to differentiate between normal cells and cancer cells. Fast-growing cells that resemble cancer cells—such as those of the bone marrow, digestive tract, mouth, and scalp—typically draw friendly fire. This is why people on chemo often experience multiple severe side-effects, including hair loss, fatigue, nausea, and sores. Antibody-drug conjugates, by selectively binding to antigens on bladder cancer cells, can reduce this kind of collateral damage. “What it does is lock the chemotherapy onto this molecule that exists on top of the cancer cells, which hopefully spares the normal cells the direct exposure to chemotherapy,” Crabb says.
Bellmunt likens these drugs to -microscopic taxis that have a bomb strapped into the passenger seat. “The taxi drives to the cancer cell, which internalizes it, and then it releases the bomb,” he says. “This is a new way of delivering chemotherapy that helps avoid side effects, and some trials have also shown a survival advantage compared to standard chemotherapy.” Right now, he says these drugs are used as a “third-line” treatment, or only in cases where standard chemotherapy and immunotherapy fail. But there’s hope that improvements in these drugs may soon push them higher up in the pecking order.
Antibody-drug conjugates are just one of several new “targeted” treatments for bladder cancer. Another is a type of drug called a tyrosine kinase inhibitor. “This is a drug that’s able to switch off a genomic trigger identified in the tumor,” Bellmunt explains. Switching off this trigger is helpful because, in some cases, it may be contributing to the growth or progression of that tumor.
Researchers are looking at tyrosine kinase inhibitors and related precision drugs alongside chemotherapy or immunotherapy treatments. Combining these drugs may lead to treatment breakthroughs in the years to come. “We all hope that the right combination might change the future,” Bellmunt adds.
Read More: 4 Important Steps to Take After a Cancer Diagnosis
What’s next in bladder-cancer treatment?
The advancements mentioned here are among the most promising, but there are plenty more.
For example, new imaging techniques may soon make radiation treatments more precise. Genetic sequencing of cancer cells is also a hot area of research. “We’re getting better at identifying biomarkers of the disease that allow us to tailor our approaches,” Lotan says. “In just the last three or four years, we’ve moved forward in identifying underlying signatures of cancers and gene expressions that can help us personalize treatment options.”
Lotan notes that many in his field are also hopeful that the future will yield accurate screening protocols for bladder cancer. “From a detection standpoint, there hasn’t been any major advancement,” he says. “Newer detection methods use panels of RNA or DNA, which are more sophisticated, but so far we have not done the large scale studies needed to demonstrate clinical utility.” Those trials involve thousands of people and “a lot of money,” he adds, and will hopefully happen soon.
“It may be possible to use urine as a screening approach, and there’s quite a lot of work going on in that area,” Crabb adds. He’s optimistic this work will eventually bear fruit. “I think urine screening is the way forward,” he says. “It’s all well and good to develop these expensive new treatments, but prevention, or at least early detection, would be better.”
There was a time when cancer experts hoped for a single breakthrough cure that would, by itself, eradicate any and all cancers. As their understanding of the disease has broadened, those hopes have faded. Today, most affirm that cancer is too variable to succumb to any silver bullet, and so the path forward will be paved with a diverse array of tailored remedies. The good news for people with bladder cancer is that each new year seems to yield meaningful strides in medical science’s ability to fight the disease. The picture now is radically changed from what it was 10 or even five years ago. People with bladder cancer are living longer and with fewer side effects than ever before. There’s reason to expect more improvements in the near future.
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com