Most of your internal organs are comfortably well protected from the outside world. But the gastrointestinal tract—or more precisely, the inside of the gastrointestinal tract—comes in contact with items from the outside world every day.
The foods you eat enter the body via the mouth, travel to the stomach, where they’re partially digested, and move on to the intestines, where the real work of extracting the nutrients and energy we need to live and thrive takes place.
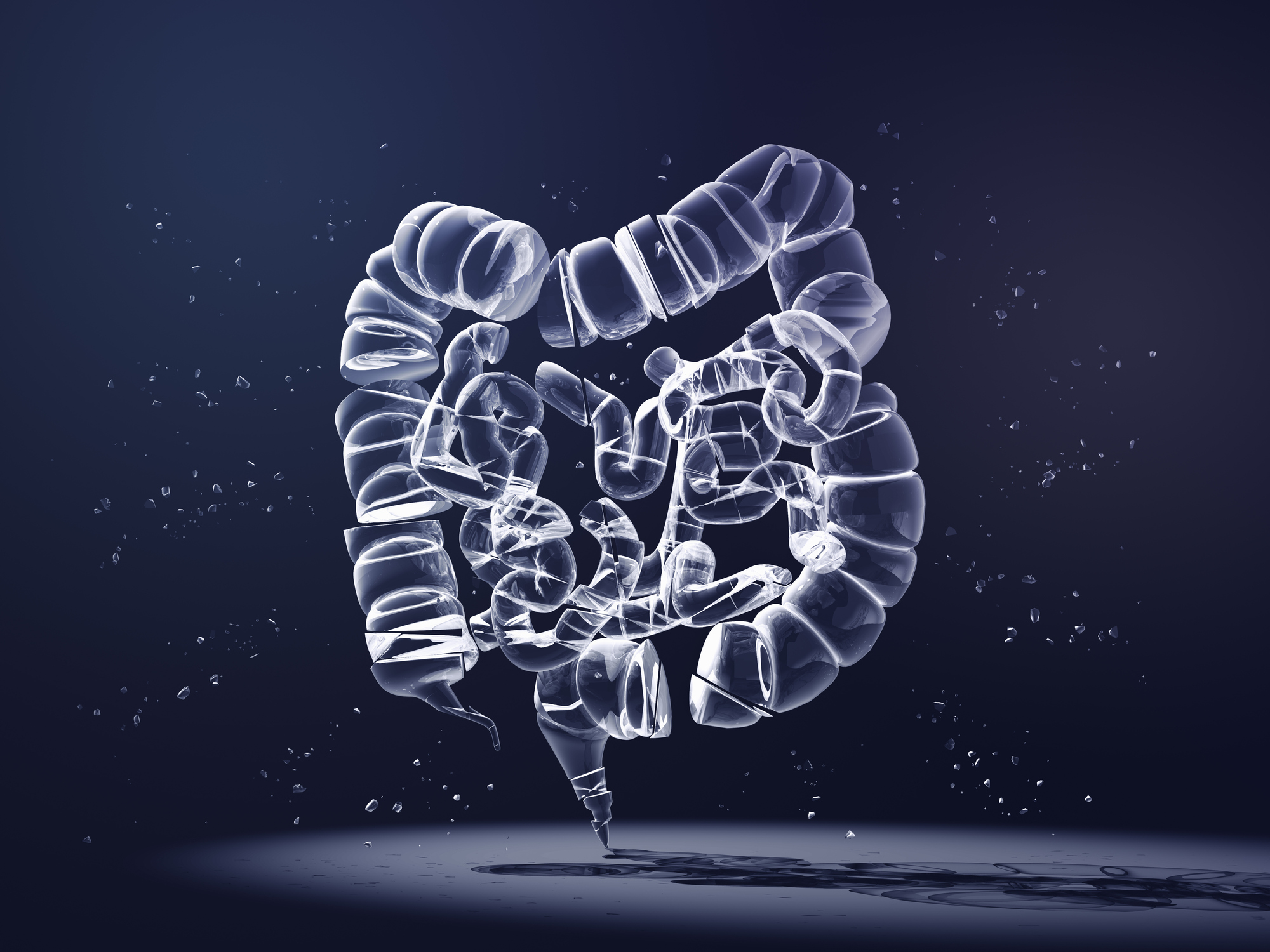
The system usually works quite well, but for some folks, it can spring leaks—just as any well-used plumbing system might. These tiny leaks can become an ongoing problem and develop into a condition called leaky gut.
“Leaky gut is a great visual term for patients, but it isn’t a true medical diagnosis,” says Dr. John Whyte, a board-certified internist based in the Washington, D.C., area. Rather than being a precise diagnosis, the term “describes the fact that your intestines aren’t working properly.”
Also sometimes referred to as heightened or increased intestinal permeability, leaky gut “is a condition in which the lining of the intestines become inflamed, damaged, or irritated, allowing microbial toxins and undigested food particles to flood into the bloodstream,” says Lacey Dunn, a functional medicine dietitian and author of The Women’s Guide to Hormonal Harmony.
The tight connections between the cells that line the intestines, called enterocytes, weaken and become more permeable than they should be. This means undigested food particles and the enzymes your body produces to break down and absorb nutrients from food end up outside the gut, where they don’t belong. “Think of your gut lining like your front door. You want the good guys (vitamins and minerals) to come in, but the bad guys (toxins and pathogens) to stay out,” Dunn says. “This is the same with your intestinal tract.”
Read More: Here’s Everything You Need to Know About Gut Health
The cells that line the inside of the gut are dynamic, says Dr. Dawn Beaulieu, director of the functional medicine IBD clinic at Vanderbilt Inflammatory Bowel Disease Clinic in Nashville. They slough off and are replaced every four to seven days. “This constant turnover presents an opportunity for ‘holes’ to form in the barrier,” says Beaulieu, who’s also a GI educator at the Institute for Functional Medicine. “The intestinal barrier is not impenetrable, and it shouldn’t be.” But it’s a Goldilocks proposition: some permeability is required for the body to function, but too much can lead to problems.
Symptoms
This leaking of matter from the gut into the bloodstream can cause infections and widespread inflammation, and it may even increase the risk of certain autoimmune disorders. Plus, it can have implications for nutrition. “It’s a double whammy, since you aren’t absorbing important vitamins and nutrients, and harmful substances that pass through are disrupting your hormones and immune system,” Whyte explains.
Symptoms often include bloating, nausea, and cramping, but “because the gut impacts our entire body, it can also cause headaches, rashes, fatigue, and joint pain,” Whyte says.
A wide variety of other symptoms, including mood disorders such as anxiety and depression, chronic fatigue, brain fog, arthritis, and allergies may result from increased intestinal permeability, Dunn says. In some cases, “leaky gut can manifest without gut-related symptoms,” she notes. “In many cases in my clinical practice, I’ve seen individuals with just skin issues or anxiety have gut infections such as parasites alongside a leaky gut.”
Such broad symptoms can make pinpointing the problem challenging, says Dr. Anil Singh, a gastroenterologist with Orlando Health in Florida. “There’s no one particular symptom” that defines leaky gut: “Some will have diarrhea or constipation, abdominal bloating, or they could feel tired. Sometimes they have nutritional deficiencies.”
All of these symptoms overlap with other GI conditions and ailments. “You have to rule out other conditions like celiac disease, irritable bowel, or colitis” before a diagnosis of leaky gut is made, Singh says.
Unfortunately, while the barrier function of the intestinal lining has been studied extensively, this hasn’t yet translated into a precise way to diagnose leaky gut. “Even after decades of scientific investigation, we currently do not have an accurate test for diagnosis,” says Dr. Kaunteya Reddy, medical director of the department of gastroenterology at the Redlands Community Hospital in Redlands, Calif.
One noninvasive test that’s sometimes used measures the ratio of lactulose to mannitol—a marker of mucosal intestinal function—but Singh says it isn’t widely available. Testing for nutritional deficiencies can also be a good idea, whether those deficiencies have resulted from leaky gut or another condition.
Who gets leaky gut?
Anyone can develop increased intestinal permeability, though “there are some people whose genetics may predispose them to a more sensitive digestive tract,” Beaulieu says. For example, people with first-degree relatives who have IBD, gluten sensitivity, celiac disease, frequent GI infections, or IBS may be at higher risk of increased intestinal permeability. However, “genetics isn’t the main factor,” Beaulieu says. “The food that we eat and how we live in the world around us is likely the main driver for our intestinal-barrier dysfunction.”
The standard American diet is high in saturated fat, sugar, and processed foods, while low in fiber. Increasingly, studies are showing that this type of eating “is a big driver in our impaired intestinal function,” Beaulieu says. Heavy alcohol use, stress, and poor sleep also disrupt the delicate makeup of the gut, she says.
Reddy notes that use of nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen sodium, are “known to cause damage to the intestinal lining and implicated in causing a leaky gut.” Minimizing the use of NSAIDs may help heal the leaky barrier.
People who already have a health issue related to the gastrointestinal tract, such as irritable bowel symptoms, Crohn’s disease, or colitis, are more likely to develop leaky gut, Singh says. Other risk factors include autoimmune disorders, arthritis, lupus, and Hashimoto’s disease, which is an autoimmune disease that affects the thyroid gland and the metabolism-regulating hormones it produces.
Exactly why this happens isn’t completely understood, but Singh says the normal bacteria that reside in the gut and help support a healthy immune system, proper digestion, and a range of other bodily functions tend to get replaced or lost, which causes inflammation. “Inflammation leads to symptoms or signs of leaky gut syndrome, because where there’s inflammation, that will cause increased permeability,” he says.
Health implications
While an autoimmune disorder like Crohn’s disease can elevate your risk of developing leaky gut syndrome, it appears the risk goes both ways: having increased intestinal permeability has been linked with an increased risk of developing several other conditions, such as arthritis, lupus, and diabetes. More research is needed to solidify the connection.
Plus, leaky gut can also increase your chances of developing other conditions related to the overgrowth of pathogens, such as Candida (yeast infections); H. pylori (a type of bacteria that causes stomachaches, nausea, and other GI symptoms); and parasites, Dunn says.
Leaky gut can also lead to nutritional deficiencies, setting you up for other conditions. For example, if your body isn’t absorbing enough iodine, you could develop hypothyroidism. And heart palpitations can arise in people with low vitamin B12 levels.
Coping with leaky gut syndrome
If your doctor suspects leaky gut syndrome, or if you’re at risk of developing it, you’ll likely be advised to make a number of lifestyle changes to help alleviate symptoms and better manage the ailment. “There is no medication that we can use,” Singh says. “It’s basically lifestyle changes,” such as changing your diet and avoiding stress.
Some patients find that working with a functional-medicine practitioner can help guide the way. “The concept of functional medicine is to create balance within our bodily systems, and this all begins in the gut,” Beaulieu says. A functional medicine practitioner will typically “follow a 5R framework for gut restoration,” which includes five steps:
Remove the things that are negatively affecting the GI tract, such as medications that might be damaging the intestines, foods you’re allergic to, toxins, and stressors. This means no more ultra-processed foods or excess sugar.
Replace those items with higher-quality foods that can promote proper digestion. A high-fiber plant-based diet is a great place to start, Dunn says. “Diversity of plants in your diet is one of the biggest contributors to a healthy gut. Fiber is your friend.”
Reinoculate the gut by helping beneficial bacteria flourish through increased intake of prebiotic, probiotic, and postbiotic foods. Fermented foods, such as kimchi and sauerkraut, can help the gut microbiome thrive and diversify.
Read More: Can Cannabis Help Your Gut?
Repair the damaged gut lining through foods and supplements. Beaulieu recommends “eating the rainbow of foods.” Vitamin and mineral supplements such as vitamin D, omega-3 fatty acids, L-glutamine, and aloe can help support the body’s efforts to repair the gut lining.
Rebalance your overall life to support better health. “Sleep, exercise, and stress all affect the GI tract,” Beaulieu says. “Balancing all of these is crucial for gut health.” While staying physically active is a good idea for overall health, Beaulieu notes that endurance exercise, such as running, biking, or boxing, can increase the risk of leaky gut, because excessive, intense exercise is a “stress-induced state” that can alter barrier function in the gut. Stay active, but don’t overdo it.
While some providers recommend adding a probiotic supplement, Beaulieu notes that evidence suggesting probiotics improve barrier function is sparse, and often conducted only in animals. More data and research are needed.
Staying well hydrated is a good way to support gut health and overall wellness, Dunn says. “Every day, drink a minimum of half your body weight in ounces of water.” But stay away from alcoholic drinks; the sugars in alcohol can exacerbate symptoms of leaky gut.
Beaulieu notes that in some mainstream medicine circles, “the concept of leaky gut is controversial,” in part because “there’s no gold standard that everyone agrees upon that can test for this, and there’s no documented scientific evidence that these changes in intestinal mucosal function will always result in metabolic changes.”
Still, “the data are compelling, and we are learning more every day,” Beaulieu says. There’s no reason not to eat right and reduce your stress levels—and if you suspect you might have leaky gut, connect with a provider who can help you manage it.
More Must-Reads from TIME
- How Donald Trump Won
- The Best Inventions of 2024
- Why Sleep Is the Key to Living Longer
- Robert Zemeckis Just Wants to Move You
- How to Break 8 Toxic Communication Habits
- Nicola Coughlan Bet on Herself—And Won
- Why Vinegar Is So Good for You
- Meet TIME's Newest Class of Next Generation Leaders
Contact us at letters@time.com