In this moment of rethinking law enforcement, we must examine how both our policing and our correctional system exacerbate the crisis of mental health in America.
As an inpatient psychiatrist, I treat patients who are psychotic, plagued by voices or visions or paranoid delusions. Or they are in the throes of mania. Or they are actively trying to harm themselves or others. Their lives are replete with hardship. Many of my patients are homeless. Some are drug-addicted. Nearly all have been victims of significant trauma. They have few safe havens, and the illnesses that besiege their minds wage a relentless war on their stability, their happiness, their safety. Many of them also serve or have served time in jail and prison. Environments that exacerbate psychiatric symptoms and routinely make mentally ill people worse and in which they face a disproportionate risk of being victimized by both officers and other inmates.
In addition to my work at the hospital, I also perform forensic evaluations for the courts, and once I began working in prisons I found a system that runs counter to every principle of human flourishing that I know. Mentally ill Americans suffer from diseases of the mind, but when they come in contact with police, they also suffer from our law enforcement policies.
At the 2016 annual meeting of the American Academy of Psychiatry and the Law, former Portland, Oregon police commander Sara Westbrook illustrated this truth to a roomful of doctors. She recounted a call her department had recently received about a mentally ill man at the city’s downtown Waterfront Park. The man was large and muscular and had a gallon jug filled with fluid attached to a long chain. He was grunting loudly, swinging the chain in a large circle above his head, and charging at people.
The police arrived, and the man began charging at the officers. Over the course of the next two and a half or three hours, the police officers worked diligently to get the man into custody with what Commander Westbrook described as “very little force.” When they succeeded, they took him to the hospital for psychiatric care. But due to a chronic shortage of psychiatric hospital beds, he was discharged from the ER before the police paperwork had even been finished. Police would soon be called again, and this time they would take the man to jail.
Encounters with police require obedience, and people with manic or psychotic symptoms—who are in the grip of delusions, or who are distracted by visions or voices, for example—are not always able to comply. The misalignment between the expectation that people follow commands and their medical inability to do so has the potential for disaster. Of the roughly 1,000 fatal shootings by police in 2018, approximately 25% of the victims were mentally ill. People with mental illness are sixteen times more likely to be killed in a police encounter than people who are psychiatrically well. This statistic is even more sobering given that it is often desperate friends or family members seeking help for their mentally ill loved one who have called police in the first place.
Even when, as in this case, police are able to safely de-escalate a psychiatric emergency, their presence at the front lines of mental health crises means that they—not clinicians—decide whether a person should be taken to jail or to the hospital. In the moment of the police encounter, law enforcement becomes the arbiter of psychiatric care. Once police are involved, even if they attempt to opt for treatment over punishment, a therapeutic and just outcome is by no means guaranteed. If psychiatric units are full, police are often forced to turn to jails to house the acutely mentally ill—facilities that have what a prison psychologist once described to me as “an iron-clad, no-refusal, admission policy.”
When mentally ill people in crisis are not admitted to hospitals, Westbrook said, she and her officers view taking them to jail as a last resort act of compassion. Given the lack of community services available for the mentally ill, she said, jail is at least “three hots and a cot, and I know somebody will check to make sure they’re still breathing.”
Across the country, jail is now seen as a treatment option—and sometimes the lone treatment option—for disadvantaged citizens with mental illness. There is even a term for this response: compassionate arrest. We use “compassionate arrests” only for people who suffer from lack of access to care for their psychiatric illnesses. We would never incarcerate people in order to obtain treatment for their cancer, or their asthma, or their diabetes. But we have come to treat psychiatric crises as legal problems rather than the health care emergencies that they are. The consequences of such an approach are stark, and have resulted in the fact that today our country’s largest mental health institution, holding more than 2,000 mentally ill people, is Chicago’s Cook County Jail.
We have ended up as a society like this because of a very specific series of choices by the government over the last 50 years. The closing of state psychiatric hospitals in the 1960s, ’70s, and ’80s led directly to the influx of mentally ill people into correctional facilities. The prospect of liberating tens of thousands of people from long-term psychiatric institutions was initially thrilling, especially given the egregious treatment and even abuse that many of the facilities’ residents had endured in the name of psychiatric “care.” In 1963 the Community Mental Health Centers Act was passed with the intention of shifting care for the mentally ill out of the asylums and into the communities. State mental hospitals across the country were defunded and closed, but the accompanying promises of community resources—from psychiatric treatment to vocational training to social supports—never materialized.
Without funds, without treatment, and suddenly also without housing, our nation’s most vulnerable citizens fell out of health care and into the realm of the legal system. The criminalization of mental illness had begun.
Since that time, the field of psychiatry has seen more than fifty years of institutional reform alongside tremendous advances in neuroscience and pharmacology. The care that hospitals like mine are now able to provide is both humane and therapeutic. However, the woefully insufficient funding of mental healthcare in America has only worsened, and therefore such care is not widely accessible. Following the 2008 recession, five billion dollars were cut from state mental health services and 4,500 psychiatric hospital beds were eliminated across the country. The lack of resources for psychiatric care in our communities means that people who suffer from severe mental illness all too often receive inadequate treatment, if they receive treatment at all. With a chronic lack of availability of both inpatient and outpatient mental health services, our mentally ill citizens are relegated to emergency rooms, to homeless shelters, and to correctional facilities.
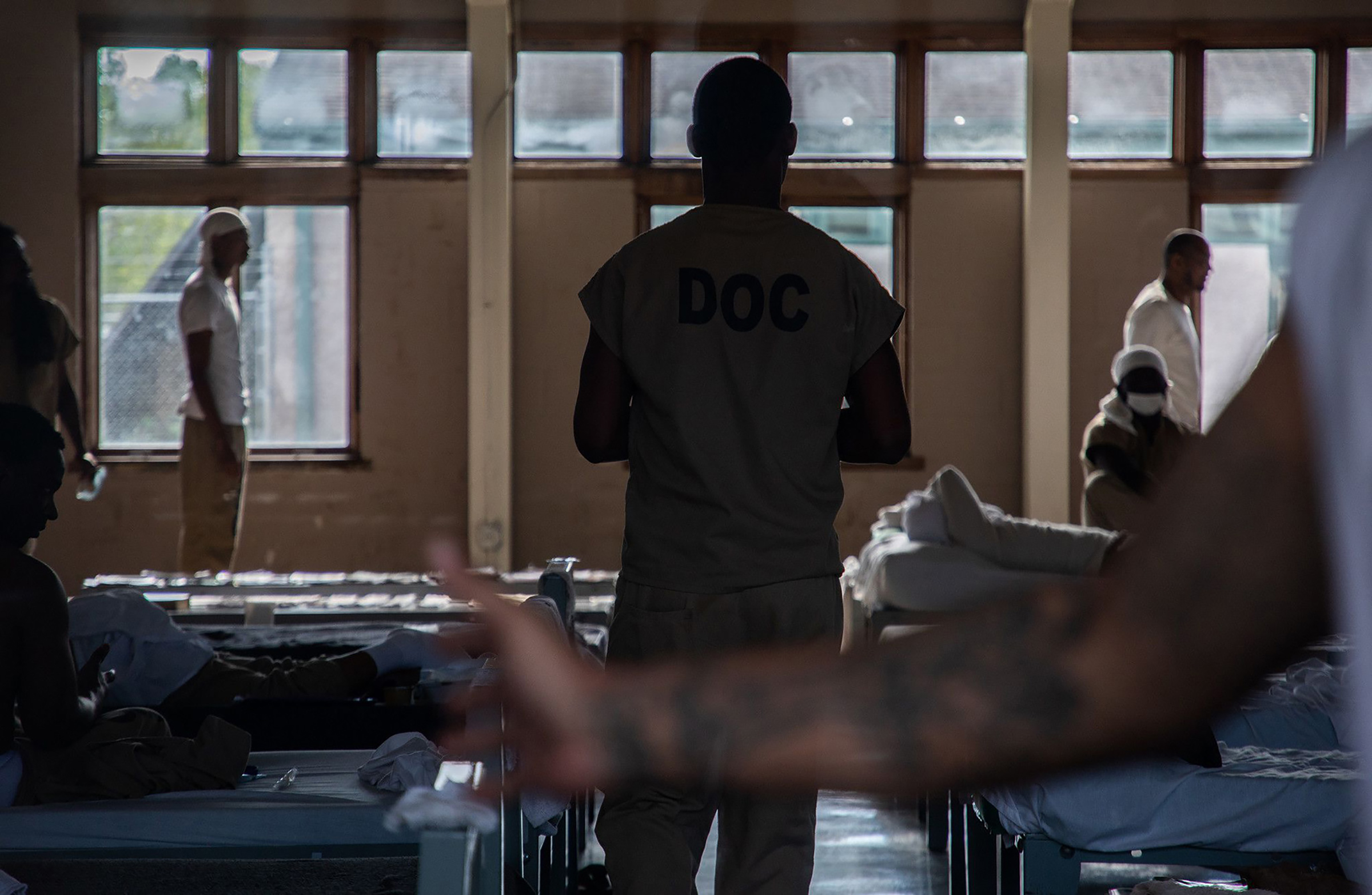
As a result, our system continues to indiscriminately shift large numbers of people who belong in therapeutic environments into punitive ones. Today, ten times more people with serious mental illness are in our nation’s correctional facilities than in our state psychiatric hospitals.

Once in jail—no matter the rationale behind the incarceration, no matter the state of their minds—all people behind bars are subjected to the same strict rules and harsh punishments. When we underfund psychiatric care in our country and then ask police to serve on the front lines of mental health emergencies, everyone loses. People who belong on treatment wards end up on cellblocks, and the results can be catastrophic.
If my patients become assaultive in the hospital, their symptoms are more aggressively targeted with medications and therapy. We aim to quickly and safely reduce their delusions or ease their hallucinations. In correctional facilities the responses to the same actions are drastically different, as was true for a man I evaluated who, in the grip of paranoia, punched a correctional officer. He incurred a felony assault charge that comes with a possible penalty of 15 years in prison. In just this way, when we punish people for the symptoms of their illnesses, our overcrowded correctional facilities become inundated with the psychiatrically ill. The practice strains our prison system and drains money from state coffers. It is also unjust and cruel.
Widespread demands for change offer us an opportunity. Calls to shift money from policing to mental health can move people who suffer from mental illness from beneath the auspices of police and corrections and back into healthcare where they belong.
But if we continue to use police as the frontline workers for mental healthcare, we perpetuate the criminalization of mental illness that began sixty years ago at great cost to the legal system, to the mentally ill, and to us all.
More Must-Reads from TIME
- Donald Trump Is TIME's 2024 Person of the Year
- Why We Chose Trump as Person of the Year
- Is Intermittent Fasting Good or Bad for You?
- The 100 Must-Read Books of 2024
- The 20 Best Christmas TV Episodes
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- Merle Bombardieri Is Helping People Make the Baby Decision
Contact us at letters@time.com