There once was a boy in Alice, Texas, who saw things a little differently from everybody else. Influenced by his father, a “country” doctor, he was drawn to science instead of football and conducted biology experiments in his parents’ garage. When he was 10, someone gave him a harmonica, but he never took a lesson or learned to read music, so he wandered the woods mimicking what he’d heard on the radio. A year after that, his mother died following a long struggle with lymphoma. What he still remembers decades later are her last, bedridden days when he spent hours holding her hand, and the burns singed on her neck from the then rudimentary radiation treatments. He would lose two uncles as a teen and later his brother to different forms of cancer. There is a satisfying catharsis, then, in the fact that James Allison would earn the Nobel Prize in Physiology or Medicine for his pioneering work in developing a new way to fight cancer.
It’s still hard for Allison to admit that his family’s tragic cancer history played a role in shaping the research career that ultimately led him to succeed where others had failed: discovering how to co-opt the body’s own immune cells to attack and destroy tumors. “I guess doing something about cancer was always kind of there in my mind,” he says.
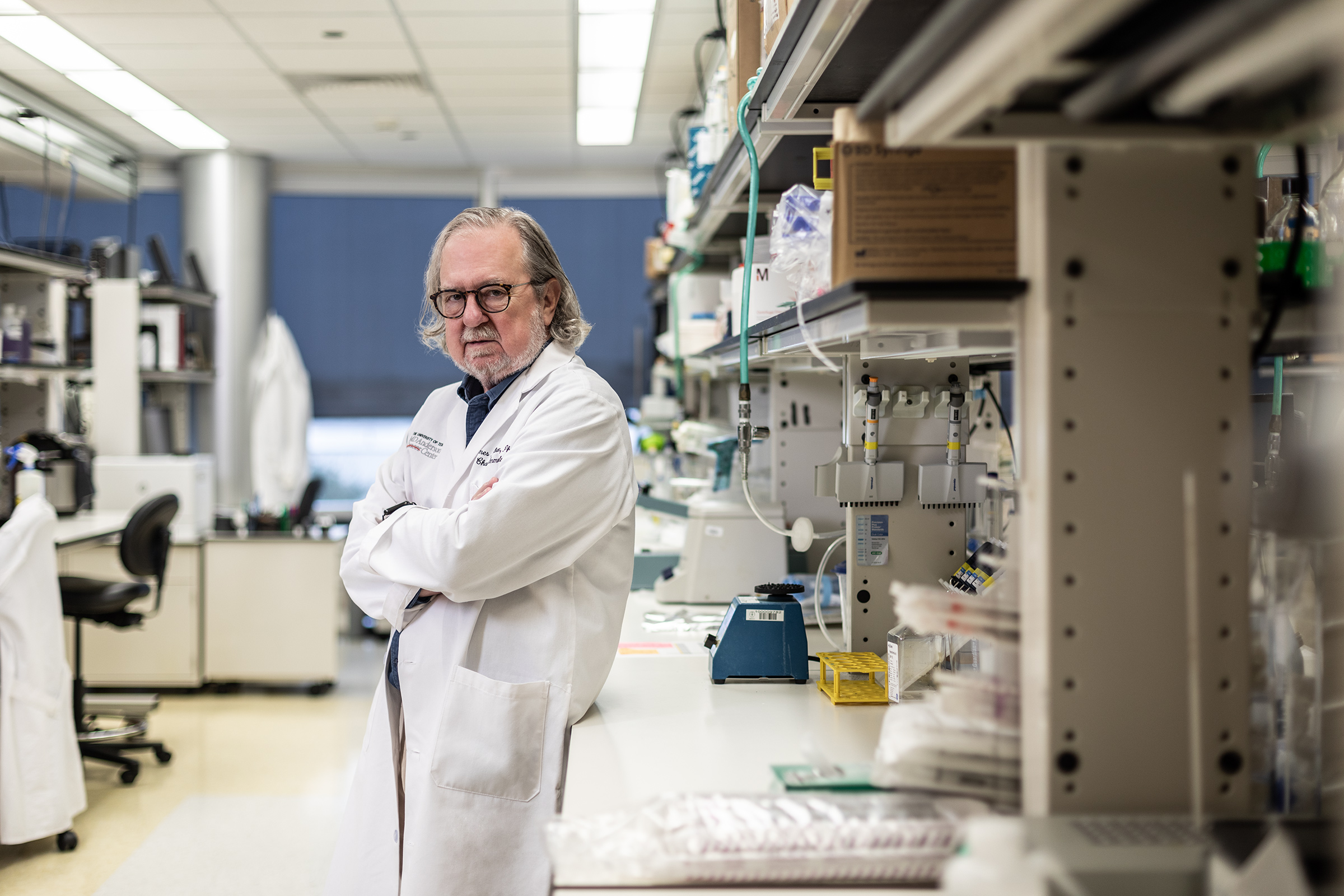
As he tells his story in his office at MD Anderson Cancer Center in Houston, Allison’s gravelly voice, edged with his Texas twang, is low and magnetic, drawing you in the way a country singer pulls people into musical arcs of love, loss, rebellion and redemption. “My mother’s death when I was young hit me hard. I didn’t realize how hard until later on,” he begins. He learned to compartmentalize his emotional family narrative from his growing curiosity about science. When his high school refused to teach evolution, he boycotted biology class, and after his father and the school counselor intervened, Allison earned that biology credit with a correspondence course taught through the University of Texas at Austin. But it wasn’t until he began pursuing undergraduate and graduate degrees there in the 1960s that he found a focus for his scientific appetite: a newly discovered set of immune cells called T cells, which at the time were essentially a biological black box. “Nobody really knew anything about them except that they cruised around the body and somehow recognized when something wasn’t right, did something about it and didn’t kill you in the process,” says Allison. “How did they know what were self and what were nonself cells, and how did they know when to react and when to do nothing?”
The mystery was irresistible for Allison, who surmised that there must be some way the T cells were able to recognize things that weren’t supposed to be there–bacteria, viruses, other pathogens and possibly even cancer cells.
It was a critical experiment with mice that ultimately led to the answer and eventually to his Nobel-winning discovery. “I had some mice sitting around that had been cured [of their tumors]. For the hell of it, I thought, What would happen if I inject them with [more] tumor cells?” It was a question born of his inquisitiveness and not part of a formal experiment, so there wasn’t a hypothesis he was testing. It turns out nothing happened–the animals didn’t get cancer–and that was a big deal. “I gave them 10 times, 100 times more tumor cells, but they wouldn’t take. They didn’t faze the mice. That made a big impression on me and made me think, Huh.” He realized that the mice had somehow “remembered” how to recognize and fight the cancer cells; their immune systems had essentially inoculated them against the disease.
By this point, Allison was working at a satellite research facility of MD Anderson Cancer Center. He says he was left “pretty unsupervised,” which meant he could pick and choose his own research projects, so he began testing his theory that T cells could actually bind with and take out cancer cells. Initially he was disappointed, and it would take a few more decades of stubborn dedication for him to understand why. Revving up an immune response isn’t simply a matter of flipping the right switches and activating the right cells. In order to protect the body’s own cells from friendly immune fire, gearing up a T cell to find and destroy its target involved a multistep process, including releasing a critical safety lock that Allison uncovered. That also applies to cancer cells, which are normal cells mutated to grow out of control.
While other scientists poured their attention into flooring the gas on the T-cell engine, Allison thought, What if you had to both apply the gas and release the parking brake in order for the T cells to get properly revved up? He eventually identified the first molecular brake that protects cancers from destruction by the immune system’s T cells. That molecular brake is now transforming cancer treatment in the form of drugs known as checkpoint inhibitors, so called because they remove the immune system’s natural blockade.
But because his data came exclusively from mice, the biotech and pharmaceutical companies he approached were reluctant to take the risk of testing checkpoint inhibitors in people. “They said anybody can cure cancer in mice, but it won’t work in humans,” says Allison. “It was insulting.”
Thanks to a friend in the biotech industry, a small company took the plunge and tested his checkpoint inhibitor against a handful of different cancers in people. Bristol-Myers Squibb eventually took notice and teamed up with the company, but even then, the idea of exploiting the immune system against cancer was so unprecedented that Allison had to persuade them to run studies long enough to see results. “I did a lot of yelling and jumping up and down and arguing with people,” he says. “I kept telling them that the tumors in mice always grew before they went away. The immune system needs time. It’s not like a drug that kills within hours.”
In 2006, while Allison was at Memorial Sloan Kettering Cancer Center in New York City, where doctors were testing the checkpoint inhibitor, he met Sharon Belvin. At 22, she had been diagnosed with late-stage melanoma, and her doctors had advised her not to start a family, since they weren’t sure she would survive long enough to raise her children. But after she was placed on the immune-based drug, Belvin’s tumors shrank away. “She was the first patient I met,” Allison says, tearing up at the memory. “After meeting her, it finally dawned on me. Until then it was abstract, and the full impact of what I was doing didn’t occur to me.” Still in remission, “she stays in touch and sends me photos of her babies,” says Allison.
Belvin is now joined by thousands of cancer patients diagnosed with melanoma, colon, liver, lung, breast, cervical and bladder cancers who are alive because of the checkpoint inhibitors that Allison helped develop. But he is not finished yet. Prostate, ovarian and other cancers are harder to treat with checkpoint inhibitors. So he is pushing to combine different immune-based drugs, many of which were inspired by his original therapy, against these more stubborn diseases. He’s also still playing the harmonica, as a member of two bands, aptly named the Checkpoints and the Checkmates. “If you find something you really love and think about all the time and that gives you joy, don’t worry about what’s going to happen,” he says.
More Must-Reads from TIME
- Why Biden Dropped Out
- Ukraine’s Plan to Survive Trump
- The Rise of a New Kind of Parenting Guru
- The Chaos and Commotion of the RNC in Photos
- Why We All Have a Stake in Twisters’ Success
- 8 Eating Habits That Actually Improve Your Sleep
- Welcome to the Noah Lyles Olympics
- Get Our Paris Olympics Newsletter in Your Inbox
Contact us at letters@time.com