A new medical research center in San Diego is embracing an innovative way to treat antibiotic resistant infections called bacteriophage therapy—phage therapy for short—which uses viruses as weapons against hard-to-treat infections.
Antibiotic-resistant infections are part of a growing global health problem. Each year in the United States, at least two million people contract drug-resistant infections, and 23,000 die from those illnesses. Bacteria naturally grow resistant to the drugs used to treat them, and for people with especially tough infections that aren’t responding to the usual medications, the options are limited.
On Thursday, the University of California San Diego School of Medicine announced that it is collaborating with national research groups and private companies to create the Center for Innovative Phage Applications and Therapeutics (IPATH). The first of its kind in North America, the center will conduct clinical trials of phage therapy for people living with severe drug-resistant infections.
MORE: Superbugs Are Nearly Impossible to Fight. This Last-Resort Medical Treatment Offers Hope
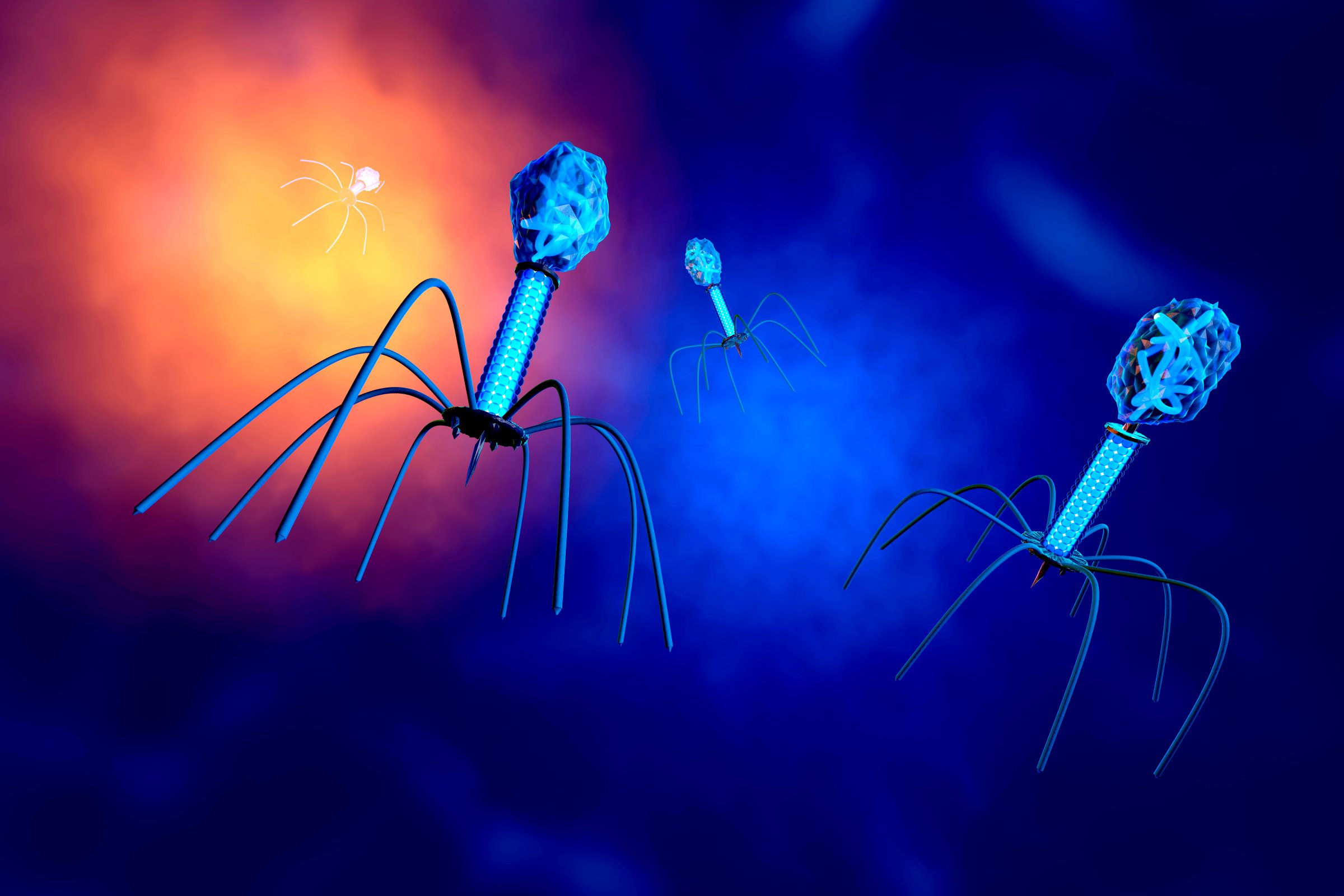
Phages are ubiquitous viruses—there are more of them than any other organism in the world—that fight bacteria. They do this by injecting their DNA into bacteria cells, where they rapidly replicate and cause bacteria to burst and die. For the most part, each phage strain attacks a specific kind of bacteria, so if scientists harness phages in the right way, they could offer a more personalized approach to treating resistant infections than broad-spectrum antibiotics, which decimate a wide variety of bacteria (including the good strains).
More than 100 years ago, researchers were studying phages as therapy. But as antibiotics rose to prominence in the 1930s, phage therapy was largely abandoned by Western researchers—until recently.
UC San Diego is among the first institutions to rediscover the promise of phage therapy. It started when Steffanie Strathdee, the associate dean of global health science at UC San Diego, and her husband Tom Patterson vacationed in Egypt in 2015, and Patterson contracted a deadly superbug infection that almost took his life. While researching last-resort options, Strathdee came across research on using phages. Phage therapy is not a currently approved treatment in the United States, and people who want access to it will need to get approval from the Food and Drug Administration (FDA) for emergency use. Patterson was given the therapy in March 2016, and it was a success. Today he’s healthy and working again.
Since then, doctors at UC San Diego Health have treated five other people with phage therapy for resistant infections, and Strathdee says she regularly hears from people asking for her help securing treatment. “Up until now, we’ve had to re-invent the wheel each time,” says Strathdee. “By having the center, we have a brain trust and can leverage more resources.”
The main goal of IPATH is to conduct clinical trials of phage therapy to better understand the therapy and ideally make it more widely available, if the FDA determines it to be safe and effective for most people. The center will initially focus its research on people with complicated multi-drug resistant infections, including people with cystic fibrosis and men and women with organ, joint or pacemaker transplants (which put them at a higher risk for such infections).
IPATH will be partnering with other groups also working to tackle the crisis of antibiotic resistance with phage therapy, including the Center for Phage Technology (CPT) at Texas A&M University, San Diego State University and two biotechnology companies called Ampliphi Biosciences and Adaptive Phage Therapeutics, Inc. “It’s not a competition,” says Strathdee. “Antibiotic resistance is a global health crisis.”
For now, phage therapy remains an experimental treatment. But the team at UC San Diego Health and their partners are hoping that with further study, phage will prove effective and gain government approval. “We think this is something that warrants further exploration with rigorous clinical trials,” says Strathdee.
More Must-Reads from TIME
- Donald Trump Is TIME's 2024 Person of the Year
- Why We Chose Trump as Person of the Year
- Is Intermittent Fasting Good or Bad for You?
- The 100 Must-Read Books of 2024
- The 20 Best Christmas TV Episodes
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- Merle Bombardieri Is Helping People Make the Baby Decision
Contact us at letters@time.com