
A blood test can reveal just how severe a person’s food allergy is and could possibly replace more invasive testing, a new study published Wednesday morning suggests.
Around 4 to 6% of American children have food allergies, a risk the U.S. Centers for Disease Control and Prevention (CDC) calls “a growing food safety and public health concern.” However, determining whether someone has a food allergy and then determining just how severe that food allergy is can be tricky.
To assess whether someone has a specific allergy, doctors will perform skin pricks or blood tests to look for skin reactions or high levels of allergy-specific antibodies. But doctors still don’t have a simple tool to test just how allergic a person is to a specific food. In some cases, the individual will need to eat whatever food they are allergic to in the presence of a physician so the doctor can determine the severity of their allergy in a safe space.
Of course, that experience isn’t without patient anxiety, which is one of the reasons why researchers at Mount Sinai Health System studied whether a blood test could predict allergy severity and potentially replace any tests that require ingesting allergens. Their research is published in the journal The Annals of Allergy, Asthma & Immunology.
The test is called basophil activation test (BAT). It’s a blood test that measures the levels of an immune cell called basophil which is activated by food exposure. The researchers used the blood test on 67 people with food sensitivities between the ages of 12 and 45 while they also underwent an exposure test comparing their reactions to peanut, tree nut, fish, shellfish, or sesame versus a placebo. The allergens or placebo were given at random, and the goal was for the researchers to see if the results of the blood test corresponded to how the people reacted.
The test proved accurate, showing a high correlation with the BAT’s scores and the severity of the individuals’ reactions.
The researchers say the ultimate goal is to develop a new test that can become part of clinical allergy diagnoses in order to improve the quality of life for patients. “[This study] should encourage similar studies, which could lead to wide widespread clinical use,” says study author Dr. Xiu-Min Li, a researcher at the Icahn School of Medicine at Mount Sinai.
Read next: Easter Egg Cookies Recalled For Containing … Eggs
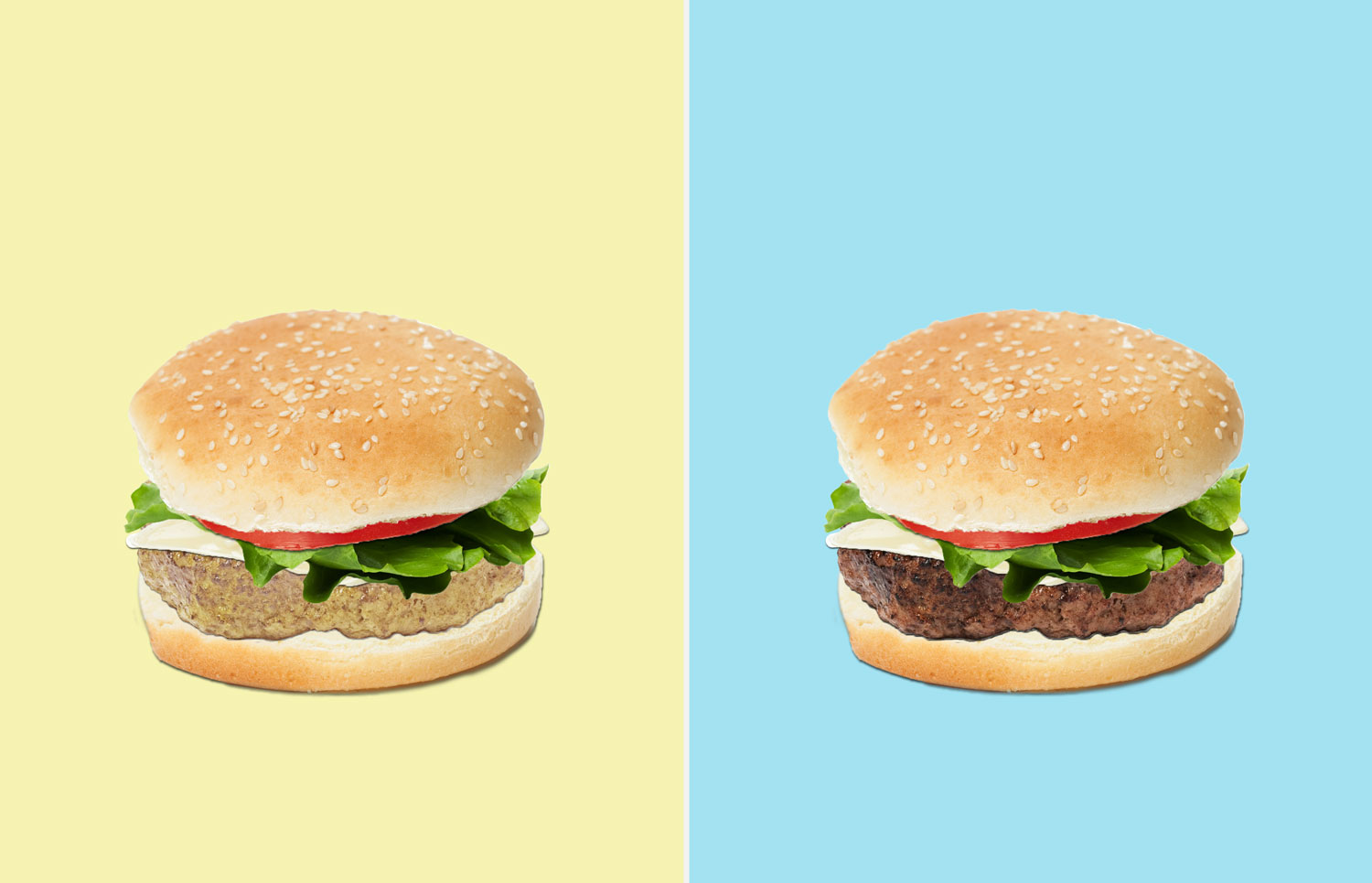
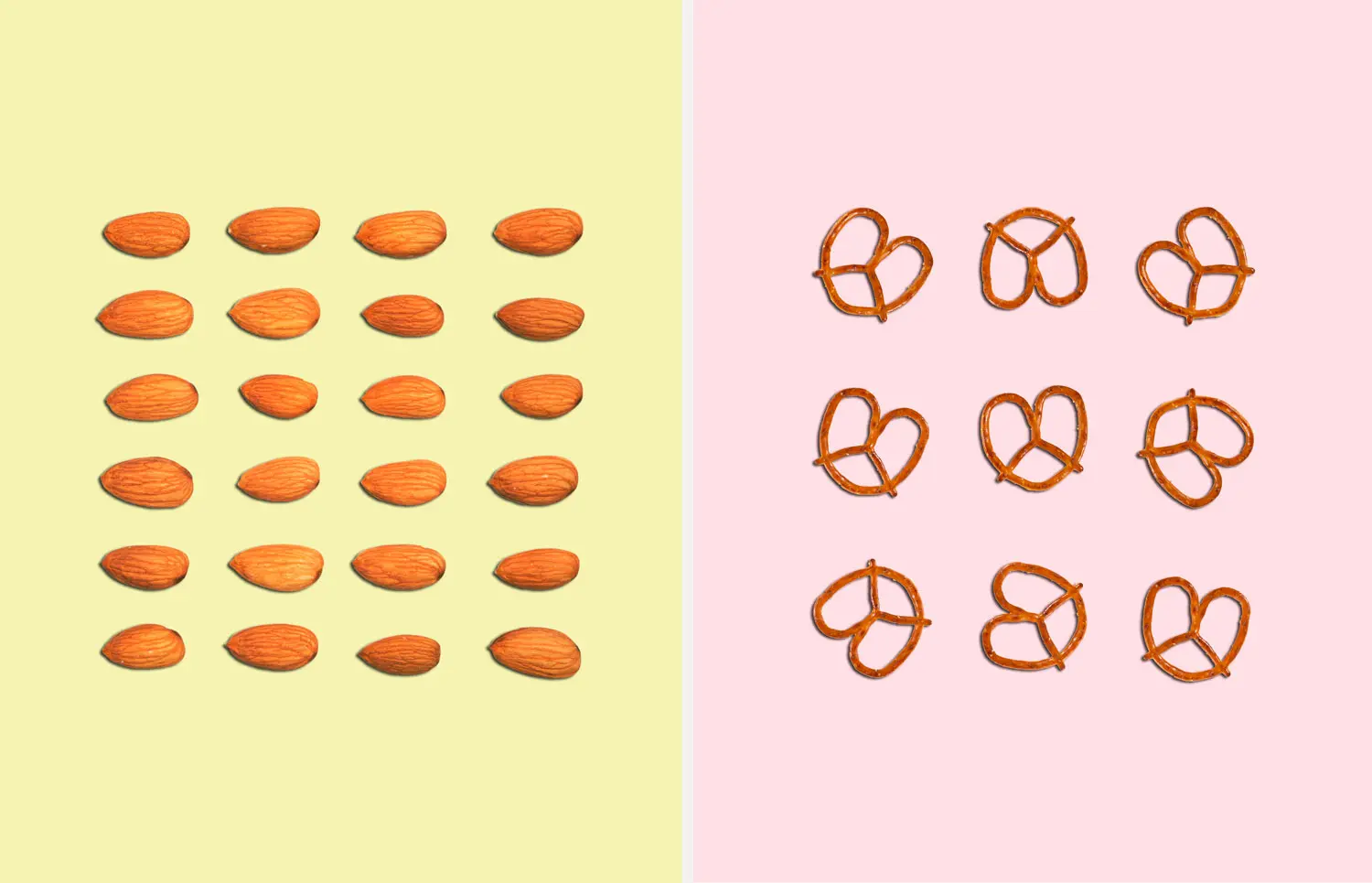
QUIZ: Should You Eat This or That?











More Must-Reads from TIME
- Why Trump’s Message Worked on Latino Men
- What Trump’s Win Could Mean for Housing
- The 100 Must-Read Books of 2024
- Sleep Doctors Share the 1 Tip That’s Changed Their Lives
- Column: Let’s Bring Back Romance
- What It’s Like to Have Long COVID As a Kid
- FX’s Say Nothing Is the Must-Watch Political Thriller of 2024
- Merle Bombardieri Is Helping People Make the Baby Decision
Contact us at letters@time.com