Some 31% of Americans say the pandemic is over. But a roughly equal number believe they’re at least a year away from resuming their pre-pandemic life.
In this in-between, divided moment, what’s the right level of cautious to aim for? What precautions should workplaces still be taking? What’s the outlook for another virus surge this fall?
For guidance, we reached out to epidemiologist Dr. Jennifer Nuzzo, director of the Pandemic Center at Brown School of Public Health. Here are excerpts from the conversation, edited for space and clarity:
What are the trends or patterns right now in how workplaces are approaching Covid precautions?
What’s driving it is employee preference. Different people have different levels of risk at this point. People who are fully vaccinated are well-protected against the thing we care about most, which is severe illness. But if somebody’s caring for a medically fragile relative at home, they’re going to view the risk of the workplace much differently than the healthy 20-year-old who had Covid last year.
From the epidemiologic perspective, taking local transmission trends into account is really important. The more Covid there is in the community, the more likely someone’s going to bring it to the office. Unfortunately it’s increasingly hard to get at those trends, because a lot of the health departments are pulling back on the frequency of the information that they’re sharing. National numbers don’t really tell you what’s going on. You could have national declining numbers, but your office could be in a hotspot. If I were running a business, I would want to look at not only where that business is operating, but where my employees generally live as well.
This is also a matter of philosophy. There might be some places where you’re really trying to make sure nobody gets sick, or you might just say, ‘Listen, this virus is not leaving us.’ Those conversations are really important to understand what level of control you’re aiming for. You may want to say masks are optional but not require them, knowing that that policy introduces some risk to the workplace. Whether that’s going to be tolerable is both a business decision and a consultation with employees.
Are mask mandates for the office still a best practice at this point in the pandemic? What about workplace vaccine mandates?
If you do choose to mandate masks, it’s worth explaining clearly what the goal of that mandate is. What are you trying to do? Are you trying to reduce the likelihood that people bring the virus into the office and spread it, and then people will be out sick? Are you trying to make your customers feel safer? Are you trying to say, ‘At this time of increased illness, we’re doing our part by reducing the likelihood that our business will contribute to additional cases in the community’?
Whatever it is, it needs to be clear, because some of the tension around masks has been a lack of understanding and clarity about what the goals are. And then decide, when are we not going to have to wear them? Some articulation of the endpoints is important—ideally in conversation with employees, because people tend to be more supportive of processes and policies that they’ve had input to.
The challenge is going to be that none of the medical tools we have are going to prevent people from becoming infected. It’s been very commonplace that businesses have mandated vaccines for their employees. Will that prevent infections in the workplace? Probably not. May it decrease the chances that your employees are going to be out for extended periods of time due to severe illness? Yes.
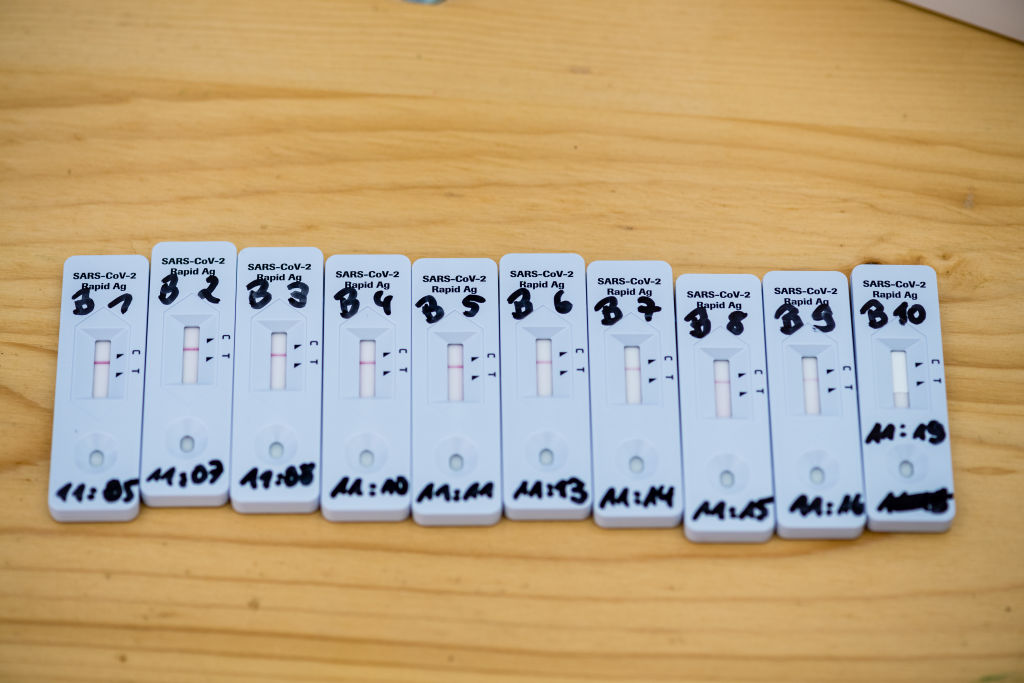
But if we want to bring down that risk of infection, we have to continue to rely on the things we’ve been using for the past two years, like masking, improved ventilation, trying to limit the amount of congregation that we do. I rapid test when I go to large meetings, because I don’t want to be the person that brought Covid to the conference. But more important is making sure that the space is well-ventilated. And if there’s any way to open windows, do it.
It feels like part of what’s changed recently is that people have moved away from the concept of contact bubbles. Is there a new framework for how we should think about public health in a workplace context?
We have to examine the physical space and whether we’re providing tools to help people as much as possible. We have not made enough progress on improving ventilation in our buildings. Businesses should absolutely demand it of the buildings that they occupy. That’s the biggest thing—these out-of-sight mechanisms that operate in the background to keep us safer, that we don’t even have to think about. And sick-leave policies have to change. It shouldn’t be that you’re rewarded for pushing through it and showing up despite being ill.
I also think masks are not going away. If I have cold symptoms and I’m going to be around people, even if I’ve tested myself and know it’s not Covid—we’re probably not going to stay home for every single cold, so employees may be encouraged to wear a mask, because nobody wants a cold either. And cleaning and disinfection are still important. Disinfecting surfaces doesn’t need to be done hourly or whatever crazy level of disinfection we were doing early in the pandemic, and it’s not necessarily important for limiting transmission of Covid. But it’s important for other viruses that can rip through an office. Norovirus can shut down a business. We have to examine the practices and policies that can just help us generally reduce the amount of infections that come to the workplace.
Are you concerned about another Covid surge in the fall or winter? What would that mean for workplaces?
I do have concerns, but they’re more like: Will we have the tools we need then to combat a surge? I’m worried about the rapid-test production pipeline possibly drying up because of funding. I’m worried about possibly not getting more up-to-date vaccines. Am I worried that we’re going to have large waves of deaths? Not as much, because we’ve seen a ratcheting down of deaths and severe illness.
I’m also a little bit worried about flu returning. While many workplaces have asked employees about Covid vaccines, they haven’t done the same with flu vaccines. While you may not mandate it, you could strongly encourage it and incentivize it. Reducing barriers to getting vaccinated tends to work. Maybe you get a half-day off to get your flu vaccine, or large employers may want to consider bringing someone in to offer vaccines to employees.
The overarching theme is the importance of being flexible and being ready to pivot if the local conditions suggest the need to pivot. And flexibility not just at the institutional level of ‘Should we do this?’ but also at the employee level, recognizing that employees have different circumstances and allowing them to make decisions that are best for themselves and their families, and trying to support them in that decision-making process as much as possible.