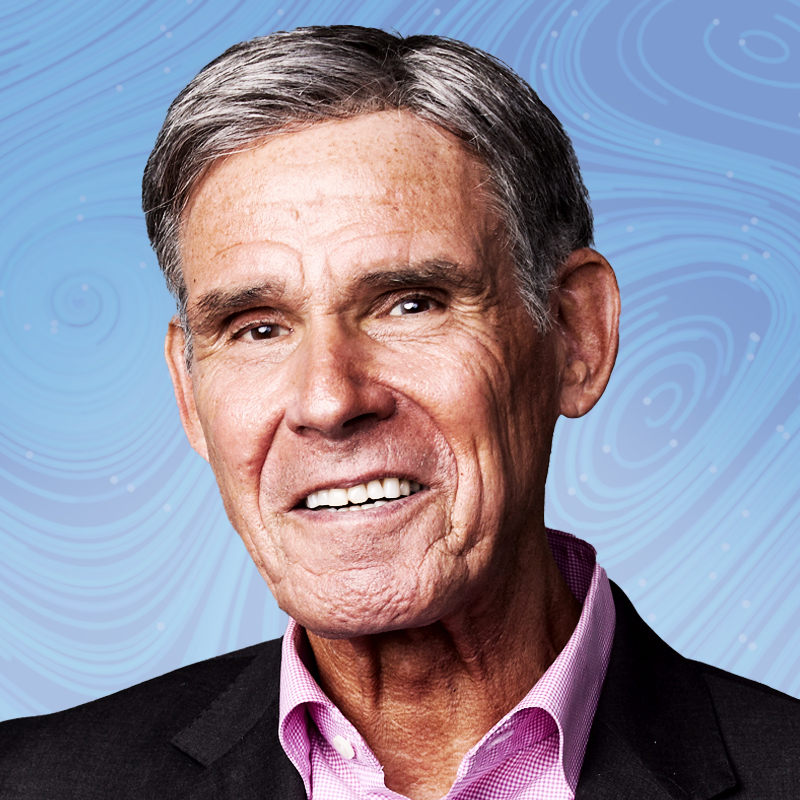
As head of the agency that insures 160 million people through Medicare and Medicaid, Chiquita Brooks-LaSure is well aware of the ripple effect that each decision she makes has on the U.S. health care system. The Centers for Medicare and Medicaid Services (CMS) has been both criticized—for its requirements for covering a new Alzheimer’s drug—and lauded—for lowering drug prices—in the past year. Brooks-LaSure defends the decision to require Alzheimer’s patients to join a registry in order to get reimbursed, saying that the process does not limit access to the drug and the information will be critical for determining long-term health outcomes.
CMS’s role in reducing drug prices is a relatively new one for the agency, since prescription drugs were not a large part of costs when it was created in the 1960s. But Medicare and Medicaid coverage has always shaped the delivery of health care in America; the agency catalyzed the desegregation of hospitals across the country when it decided to withhold federal funding from any hospital that discriminated based on race. Today that legacy continues, most notably in drug pricing. Not only do private insurers often follow CMS’s lead in how much to reimburse for treatments, but beginning in 2023, the Inflation Reduction Act gave CMS the ability to negotiate directly with drug makers to set prices that it reimburses. First up was insulin, which CMS capped at $35 a month for its members beginning in July 2023; that prompted manufacturers including Eli Lilly, Novo Nordisk, and Sanofi to drop their prices as well. Last summer, the agency announced the first 10 drugs to be negotiated in the program, which included medications for diabetes, stroke, and blood clots. And for the first time, Medicare also capped overall out-of-pocket spending on prescription drugs for members at $3,300 to $3,800 a year, dropping to $2,000 in 2025. “When Medicare starts paying attention to something or setting rules, it changes the entire health system,” says Brooks-LaSure. “I think we are at an inflection point on prescription drugs. There is a feeling that enough is enough, and that current pricing is not sustainable.”
Correction, May 2
The original version of this story mischaracterized the state of CMS's drug negotiations program. Last summer, CMS announced the first 10 drugs to be negotiated in the program, but has not yet completed these discussions.
More Must-Reads from TIME
- Why Biden Dropped Out
- Ukraine’s Plan to Survive Trump
- The Rise of a New Kind of Parenting Guru
- The Chaos and Commotion of the RNC in Photos
- Why We All Have a Stake in Twisters’ Success
- 8 Eating Habits That Actually Improve Your Sleep
- Welcome to the Noah Lyles Olympics
- Get Our Paris Olympics Newsletter in Your Inbox
Contact us at letters@time.com