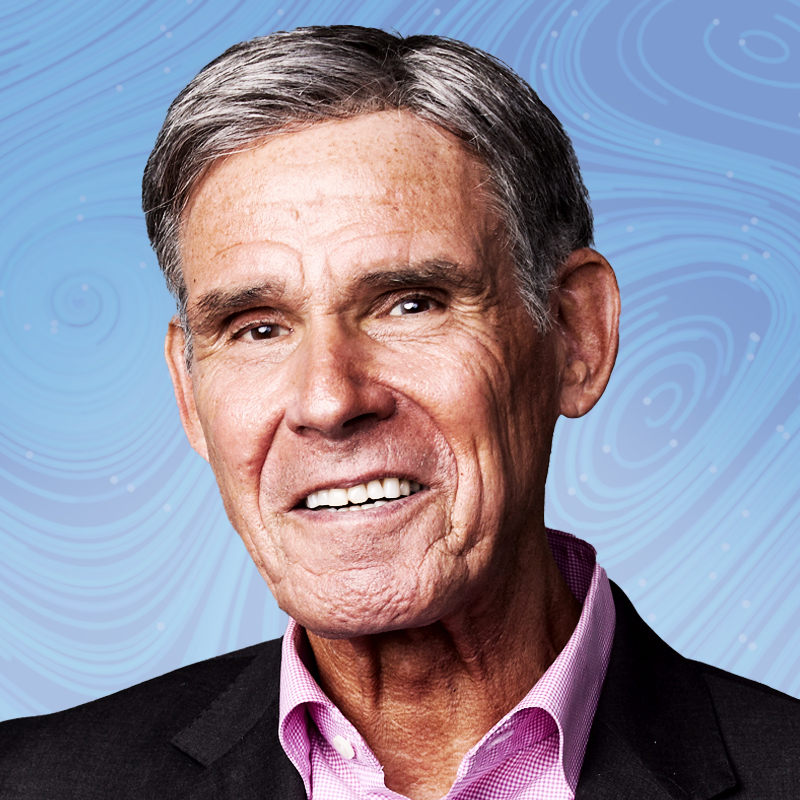
For Adrian Hill, director of the Jenner Institute at the University of Oxford, the stakes for a malaria vaccine were laid bare when, as a young researcher in 1988, he worked at a hospital in Gambia. Children were crammed two and three to a bed, “dying in front of your eyes,” he says. The world has gained ground since then, but about 600,000 people died from malaria in 2022, most younger than 5. This year may mark a turning point: while malaria has existed for at least 30 million years, and humans have chased a vaccine for a century, the first two vaccines are being rolled out—including R21/Matrix-M, which was developed by Hill and collaborators and is 78% effective. Hill’s vaccine is cheaper and easier to produce than the other shot: it is estimated to cost less than $4 a dose, and has an annual manufacturing capacity for hundreds of millions of shots. If deployed widely, it could save hundreds of thousands of lives annually.
Though he’s focused on the challenges, Hill hopes that the vaccine, in conjunction with medications and bed nets, will reawaken hopes of eradicating malaria, even within the next decade. “It would be amazing, wouldn’t it, to go back to that hospital,” he says. “And I’ll say, ‘Where’s the malaria ward?’ And they’ll say, ‘Sir, we don’t have malaria cases anymore.’”
More Must-Reads from TIME
- Donald Trump Is TIME's 2024 Person of the Year
- Why We Chose Trump as Person of the Year
- Is Intermittent Fasting Good or Bad for You?
- The 100 Must-Read Books of 2024
- The 20 Best Christmas TV Episodes
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- Merle Bombardieri Is Helping People Make the Baby Decision
Contact us at letters@time.com