Ashley just had a baby. She’s sitting on the couch in a relative’s apartment in Clarksdale, Miss., wearing camo-print leggings and fiddling with the plastic hospital bracelets still on her wrists. It’s August and pushing 90 degrees, which means the brown patterned curtains are drawn, the air conditioner is on high, and the room feels like a hiding place. Peanut, the baby boy she delivered two days earlier, is asleep in a car seat at her feet, dressed in a little blue outfit. Ashley is surrounded by family, but nobody is smiling. One relative silently eats lunch in the kitchen, her two siblings stare glumly at their phones, and her mother, Regina, watches from across the room. Ashley was discharged from the hospital only hours ago, but there are no baby presents or toys in the room, no visible diapers or ointments or bottles. Almost nobody knows that Peanut exists, because almost nobody knew that Ashley was pregnant. She is 13 years old. Soon she’ll start seventh grade.
In the fall of 2022, Ashley was raped by a stranger in the yard outside her home, her mother says. For weeks, she didn’t tell anybody what happened, not even her mom. But Regina knew something was wrong. Ashley used to love going outside to make dances for her TikTok, but suddenly she refused to leave her bedroom. When she turned 13 that November, she wasn't in the mood to celebrate. “She just said, ‘It hurts,’” Regina remembers. “She was crying in her room. I asked her what was wrong, and she said she didn’t want to tell me.” (To protect the privacy of a juvenile rape survivor, TIME is using pseudonyms to refer to Ashley and Regina; Peanut is the baby’s nickname.)
The signs were obvious only in retrospect. Ashley started feeling sick to her stomach; Regina thought it was related to her diet. At one point, Regina even asked Ashley if she was pregnant, and Ashley said nothing. Regina hadn’t yet explained to her daughter how a baby is made, because she didn’t think Ashley was old enough to understand. “They need to be kids,” Regina says. She doesn’t think Ashley even realized that what happened to her could lead to a pregnancy.
On Jan. 11, Ashley began throwing up so much that Regina took her to the emergency room at Northwest Regional Medical Center in Clarksdale. When her bloodwork came back, the hospital called the police. One nurse came in and asked Ashley, “What have you been doing?” Regina recalls. That’s when they found out Ashley was pregnant. “I broke down,” Regina says.
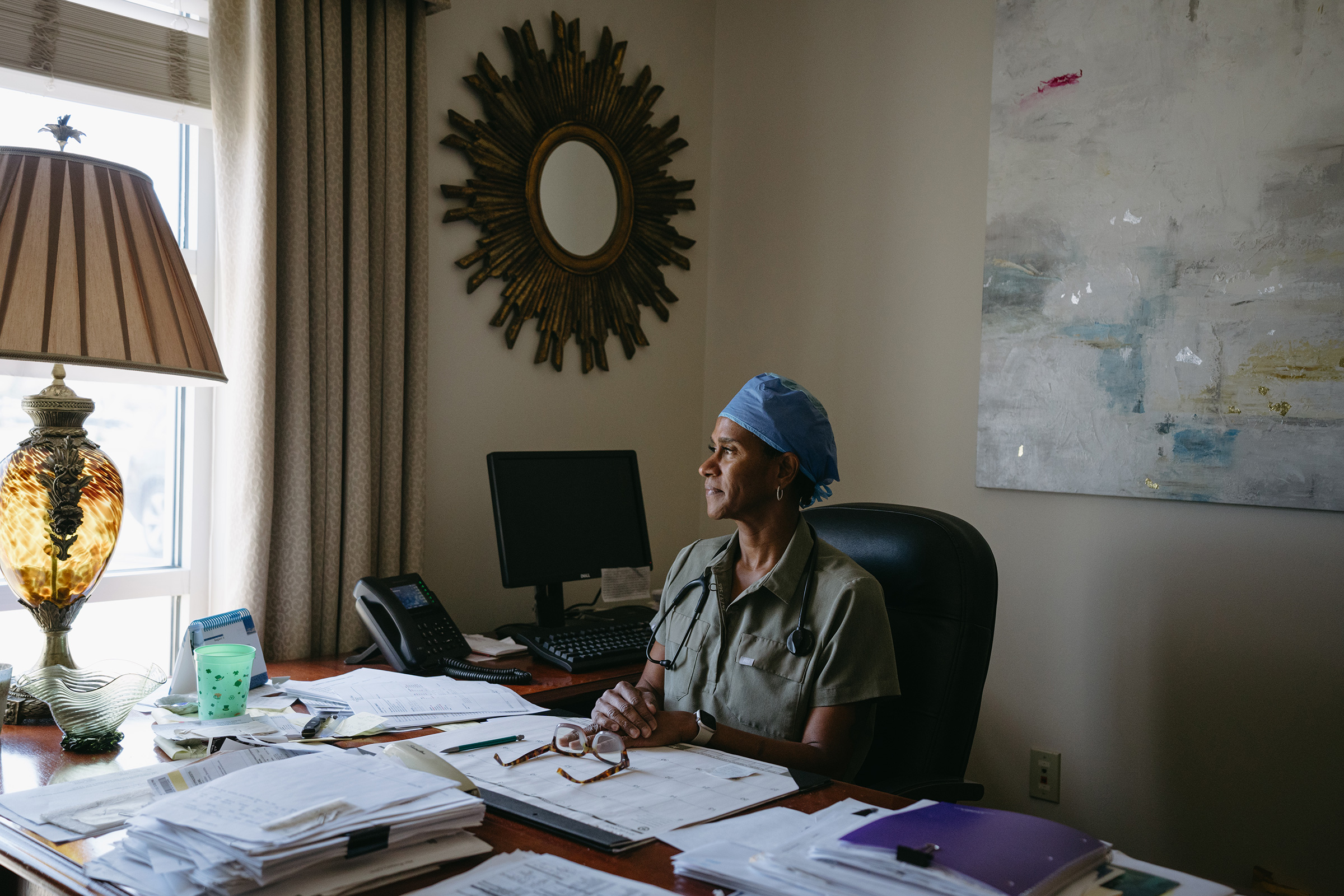
Dr. Erica Balthrop was the ob-gyn on call that day. Balthrop is an assured, muscular woman with close-cropped cornrows and a tattoo of a feather running down her arm. She ordered an ultrasound, and determined Ashley was 10 or 11 weeks along. “It was surreal for her,” Balthrop recalls. "She just had no clue.” The doctor could not get Ashley to answer any questions, or to speak at all. “She would not open her mouth.” (Balthrop spoke about her patient's medical history with Regina's permission.)
At their second visit, about a week later, Regina tentatively asked Balthrop if there was any way to terminate Ashley’s pregnancy. Seven months earlier, Balthrop could have directed Ashley to abortion clinics in Memphis, 90 minutes north, or in Jackson, Miss., two and a half hours south. But today, Ashley lives in the heart of abortion-ban America. In 2018, Republican lawmakers in Mississippi enacted a ban on most abortions after 15 weeks of pregnancy. The law was blocked by a federal judge, who ruled that it violated the abortion protections guaranteed by Roe v. Wade. The Supreme Court felt differently. In their June 2022 decision in Dobbs v. Jackson Women’s Health Organization, the Supreme Court overturned the constitutional right to abortion that had existed for nearly half a century. Within weeks, Mississippi and every state that borders it banned abortion in almost all circumstances.
Balthrop told Regina that the closest abortion provider for Ashley would be in Chicago. At first, Regina thought she and Ashley could drive there. But it’s a nine-hour trip, and Regina would have to take off work. She’d have to pay for gas, food, and a place to stay for a couple of nights, not to mention the cost of the abortion itself. “I don’t have the funds for all this,” she says.
So Ashley did what girls with no other options do: she did nothing.

Clarksdale is in the Mississippi Delta, a vast stretch of flat, fertile land in the northwest corner of the state, between the Mississippi and Yazoo rivers. The people who live in the Delta are overwhelmingly Black. The poverty rate is high. The region is an epicenter of America’s ongoing Black maternal-health crisis. Mississippi has the second-highest maternal-mortality rate in the country, with 43 deaths per 100,00 live births, and the Delta has among the worst maternal-healthcare outcomes in the state. Black women in Mississippi are four times as likely to die from pregnancy-related complications as white women.
Mississippi’s abortion ban is expected to result in thousands of additional births, often to low-income, high-risk mothers. Dr. Daniel Edney, Mississippi’s top health official, tells TIME his department is “actively preparing” for roughly 4,000 additional live births this year alone. Edney says improving maternal-health outcomes is the “No. 1 priority” for the Mississippi health department, which has invested $2 million into its Healthy Moms, Healthy Babies program to provide extra support for new mothers. “There is a sense of following through, and not just as a predominantly pro-life state,” says Edney. “We don’t just care about life in utero. We care about life, period, and that includes the mother’s life and the baby’s life.”

Mississippi’s abortion ban contains narrow exceptions, including for rape victims and to save the life of the mother. As Ashley's case shows, these exceptions are largely theoretical. Even if a victim files a police report, there appears to be no clear process for granting an exception. (The state Attorney General’s office did not return TIME’s repeated requests to clarify the process for granting exceptions; the Mississippi Board of Medical Licensure and the Mississippi State Medical Association did not reply to TIME’s requests for explanation.) And, of course, there are no abortion providers left in the state. In January, the New York Times reported that since Mississippi's abortion law went into effect, only two exceptions had been made. Even if the process for obtaining one were clear, it wouldn’t have helped Ashley. Regina didn’t know that Mississippi’s abortion ban had an exception for rape.
Even before Dobbs, it was perilous to become a mother in rural Mississippi. More than half the counties in the state can be classified as maternity-care deserts, according to a 2023 report from the March of Dimes, meaning there are no birthing facilities or obstetric providers. More than 24% of women in Mississippi have no birthing hospital within a 30-minute drive, compared to the national average of roughly 10%. According to Edney, there are just nine ob-gyns serving a region larger than the state of Delaware. Every time another ob-gyn retires, Balthrop gets an influx of new patients. “These patients are having to drive further to get the same care, then they're having to wait longer,” Balthrop says.
Read More: The Future of Abortion Access After Roe v. Wade.
Those backups can have cascading effects. Balthrop recalls one woman who had to wait four weeks to get an appointment. "That’s unacceptable, because you don't know if she’s high risk or not until she sees you," the doctor says says. Her patient "didn’t know she was pregnant. Now the time has lapsed so much that she can’t drive anyplace to terminate even if she chose to."
Early data suggests the Dobbs decision will make this problem worse. Younger doctors and medical students say they don't want to move to states with abortion restrictions. When Emory University researcher Ariana Traub surveyed almost 500 third- and fourth-year medical students in 2022, close to 80% said that abortion laws influenced where they planned to apply to residency. Nearly 60% said they were unlikely to apply to any residency programs in states with abortion restrictions. Traub had assumed that abortion would be most important to students studying obstetrics, but was surprised to find that three-quarters of students across all medical specialties said that Dobbs was affecting their residency decisions.
“People often forget that doctors are people and patients too,” Traub says. “And residency is often the time when people are in their mid-30s and thinking of starting a family.” Traub found that medical students weren’t just reluctant to practice in states with abortion bans. They didn’t want to become pregnant there, either.
And so Dobbs has compounded America's maternal-health crisis: more women are delivering more babies, in areas where there are already not enough doctors to care for them, while abortion bans are making it more difficult to recruit qualified providers to the regions that need them most. “People always ask me: ‘Why do you choose to stay there?’” says Balthrop, who has worked in the Delta for more than 20 years. “I feel like I have no choice at this point."

The weeks went on, and Ashley entered her second trimester. She wore bigger clothes to hide her bump, until she was so big that Regina took her out of school. They told everyone Ashley needed surgery for a bad ulcer. “We’ve been keeping it quiet, because people judge wrong when they don’t know what’s going on,” Regina says. She’s been trying to keep Ashley away from “nosy people.” For months, Ashley spent most of the day alone, finishing up sixth grade on her laptop. The family still has no plans to tell anybody about the pregnancy. “It’s going to be a little private matter here,” Regina says.
Ashley has ADHD and trouble focusing, and has an Individualized Education Program at school. She had never talked much, but after the rape she went from shy to almost mute. Regina thinks she may have been too traumatized to speak. At first, Regina couldn’t even get Ashley to tell her about the rape at all.
In an interview in a side bedroom, while Ashley watched TV with Peanut in another room, Regina recounted the details of her daughter’s sexual assault, as she understands them. It was a weekend in the fall, shortly after lunchtime, and Ashley, then 12, had been outside their home making TikToks while her uncle and sibling were inside. A man came down the street and into the front yard, grabbed Ashley, and covered her mouth, Regina says. He pulled her around to the side of the house and raped her. Ashley told Regina that her assailant was an adult, and that she didn’t know him. Nobody else witnessed the assault.
Shortly after finding out Ashley was pregnant, Regina filed a complaint with the Clarksdale Police Department. The department's assistant chief of police, Vincent Ramirez, confirmed to TIME that a police report had been filed in the matter, but refused to share the document because it involved a minor.

Regina says that another family member believed they had identified the rapist through social-media sleuthing. The family says they flagged the man they suspected to the police, but the investigation seemed to go nowhere. Ramirez declined to comment on an ongoing investigation, but an investigator in the department confirmed to TIME that an arrest has not yet been made. With their investigation still incomplete, police have not yet publicly confirmed that they believe Ashley’s pregnancy resulted from sexual assault.
Regina felt the police weren’t taking the case seriously. She says she was told that in order to move the investigation forward, the police needed DNA from the baby after its birth. Experts say this is not unusual. Although it is technically possible to obtain DNA from a fetus, police are often reluctant to initiate an invasive procedure on a pregnant victim, says Phillip Danielson, a professor of forensic genetics at the University of Denver. They typically test DNA only on fetal remains after an abortion, or after a baby is born, he says.
But almost three days after Peanut was born, the police still hadn’t picked up the DNA sample; it was only after inquiries from TIME that officers finally arrived to collect it. Asked at the Clarksdale police station why it had taken so long after Peanut's birth for crucial evidence to be collected, Ramirez shrugged. “It’s a pretty high priority, as a juvenile,” he says. “Sometimes they slip a little bit because we’ve got a lot going on, but then they come back to it.”

Ashley doesn’t say much when asked how it felt to learn she was pregnant. Her mouth twists into a shy grimace, and she looks away. “Not good,” she says after a long pause. “Not happy.”
Regina’s own feelings about abortion became more complicated as the pregnancy progressed. She got pregnant with her first daughter at 17, and was a mother at 18. “I was a teen,” says Regina, now 33. “But I wasn’t as young as her.”
Regina had considered abortion during one of her own pregnancies. But her grandmother admonished her, “Your mama didn’t abort you.” Now Regina felt caught between her family’s general disapproval of abortion and the realization that her 13-year-old daughter was pregnant as the result of a rape. “I wish she had just told me when it happened. We could have gotten Plan B or something,” Regina says, referring to the emergency contraceptive often known as the “morning-after pill.” “That would have been that.”
Balthrop often sees this kind of ambivalence. Clarksdale is in the heart of the Bible Belt, and many of her patients are Black women from religious families. Even if they want to terminate their pregnancies, Balthrop says, many of them ultimately decide not to go through with it. Since the Dobbs decision, however, Balthrop has seen an increase in “incomplete abortions,” which is when the pregnancy has been terminated but the uterus hasn’t been fully emptied. Medication abortions— abortions managed with pills, which are increasingly available online—are overwhelmingly safe, but occasionally can have minor complications when the pills are not taken exactly as directed. “They're having complications after—not serious, but they'll come in with significant bleeding, and then we still have to finish the process,” Balthrop says, explaining that they sometimes have to evacuate dead fetal tissue.
According to Balthrop, Ashley didn’t have complications during her pregnancy. But she didn’t start speaking more until she felt the baby move, around her sixth month. “That’s when it hit home,” Balthrop says. “She’d complain about little aches and pains that she had never had before. That’s when her mom would come in and say, ‘She asked me this question,’ and the three of us would sit and talk about it.”
How did Ashley feel in anticipation of becoming a mother? “Nervous,” is all she will say. Toward the end of the pregnancy, she was terrified of going into labor, Balthrop recalls. Most of her questions were about pushing, and delivery, and how painful it would be. She was focused on “the delivery process itself,” Balthrop says. “Not, ‘What am I going to do when I take this baby home?’”
The Clarksdale Woman’s Clinic, where Balthrop practices, is across the street from the emergency room at Northwest Regional Medical Center, where Ashley first learned she was pregnant. The clinic is large and welcoming, with comfortable chairs and paintings of flowers on the walls. The staff is kind and efficient, the space is clean, and it helps that the three ob-gyns on staff are Black, since most of the patients are Black women. The clinic’s strong reputation attracts patients from an hour away in all directions. It is a lifeline in a vast region with few other maternity health options.
Even for healthy patients, it can be dangerous to be pregnant in such a rural area. “We have patients who walk to our clinic. They don't have transportation,” says Casey Shoun, an administrative assistant at Clarksdale Woman’s. Some can get Medicaid transportation, but it’s notoriously unreliable. The trip can be hard even for local residents: the roads leading to the clinic don’t have good sidewalks, and temperatures in the Delta regularly reach 100 degrees in the summer.

Shoun says the clinic gets patients who are six months pregnant by the time they have their first prenatal appointment. “We've had patients who go to the hospital, and they've already delivered,” Shoun says. Balthrop recalls one woman who went into labor about seven weeks early, and had to drive 45 minutes to get to the hospital. She was too late. “By the time she got here, the baby had passed already,” Balthrop says.
Clarksdale Woman's is equipped to handle routine appointments for a healthy pregnancy like Ashley’s. But a pregnant woman with any complication at all—from deep-vein thrombosis to diabetes, preeclampsia to advanced maternal age—will have to make a three-hour round trip drive to Memphis to see the closest maternal-fetal-medicine specialist. The most vulnerable patients are often the ones who have to travel the farthest for pregnancy care.
Read More: Inside Mississippi's Last Abortion Clinic.
One morning in August, as the clinic filled, Balthrop allowed TIME to interview consenting patients in the waiting room and parking lot. One of them was Mikashia Hardiman, who is 18 years old and pregnant with her first child. Hardiman had just had her 20-week anatomy scan, and learned that she has a shortened cervix, which means her mother now has to drive her to Memphis to see a specialist.
Jessica Ray, 36, was 13 weeks pregnant with her third child. Three years ago, when she suddenly went into labor with her second child at 33 weeks, she drove herself 45 minutes to the hospital and delivered less than half an hour after she arrived. Ray knows the travel ordeals ahead of her: because she had preeclampsia with her first two pregnancies, she’ll have to go see the specialist in Memphis each month. “You have to take off work and make sure somebody's getting your kids,” Ray says.
Balthrop, who has three kids of her own, has long considered moving to a different region with a better education system. "I feel like I can’t," she says. "I would be letting so many people down."
But the clinic is under serious financial strain. Between overhead, malpractice insurance, the increasing costs of goods and services, and decreasing insurance reimbursements, Balthrop and her colleagues can barely afford to keep Clarksdale Woman's open. They’re considering selling the practice to a hospital 30 miles away. If that happened, Balthrop says, babies would no longer be delivered in Clarksdale, a city of less than 15,000. Some of her patients would have to leave the Delta—possibly driving an hour or more—to get even the most basic maternity care.
For the patients who already struggle to make it to Clarksdale, that would spell disaster. "They just wouldn't get care until they show up for delivery at the hospital,” says Shoun, the administrative assistant. “Imagine if we weren't here. Where would they go?"

Ashley started feeling contractions on a Saturday afternoon when she was 39 weeks pregnant. She called Regina, who came home from work, and together they started timing them. They arrived at the hospital around 8 p.m. that night. An exam revealed Ashley was already six centimeters dilated. Her water broke soon after, and she got an epidural. She delivered Peanut within five hours. Ashley describes the birth in one word: “Painful.”
For Regina, the arrival of her first grandchild has not eased the pain of watching what her daughter has endured. “This situation hurts the most because it was an innocent child doing what children do, playing outside, and it was my child,” Regina says. “It still hurts, and is going to always hurt.”
Ashley doesn’t know anybody else who has a baby. She doesn’t want her three friends at school to find out that she has one now. Regina is working on an arrangement with the school so Ashley can start seventh grade from home until she’s ready to go back in person. Relatives will watch Peanut while Regina is at work. Is there anything about motherhood that Ashley is excited about? She twists her mouth, shrugs, and says nothing. Is there anything Ashley wants to say to other girls? “Be careful when you go outside,” she says. “And stay safe.”
There is only one moment when Ashley smiles a little, and it’s when she describes the nurses she met in the doctors’ office and delivery room. One of them, she remembers, was “nice” and “cool.” She has decided that when she grows up, she wants to be a nurse too. “To help people,” she says. For a second, she looks like any other soon-to-be seventh grader sharing her childhood dream. Then Peanut stirs in his car seat. Regina says he needs to be fed. Ashley’s face goes blank again. She is a mother now.
With reporting by Leslie Dickstein
More From TIME
More Must-Reads from TIME
- Donald Trump Is TIME's 2024 Person of the Year
- Why We Chose Trump as Person of the Year
- Is Intermittent Fasting Good or Bad for You?
- The 100 Must-Read Books of 2024
- The 20 Best Christmas TV Episodes
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- Merle Bombardieri Is Helping People Make the Baby Decision
Write to Charlotte Alter/Clarksdale, Miss. at charlotte.alter@time.com
