About three-quarters of people in the U.S. have had COVID-19 at least once, according to the latest federal estimates—but, if they were asymptomatic, some of them might not realize it.
Since the beginning of the pandemic, researchers have tried to understand why some people who are infected by the SARS-CoV-2 virus never experience telltale symptoms like a cough, sore throat, or fever. A new study, published July 19 in Nature, offers one possible explanation: it’s thanks to a quirk of their genes.
Genes that are part of what’s known as the HLA complex help the body identify proteins made by pathogens, such as viruses, and leap into action when a foreign invader is present. Some people with a common HLA mutation seem to respond to the SARS-CoV-2 virus as if their immune systems already know how to fight it off, even if they’ve never been exposed before, explains study co-author Jill Hollenbach, a professor of neurology, epidemiology, and biostatistics at the University of California, San Francisco. That recognition appears to facilitate an immune response fast and effective enough that people don’t even develop symptoms.
“Conceptually,” Hollenbach says, “it’s the same as what we’re trying to accomplish with vaccination.”
More from TIME
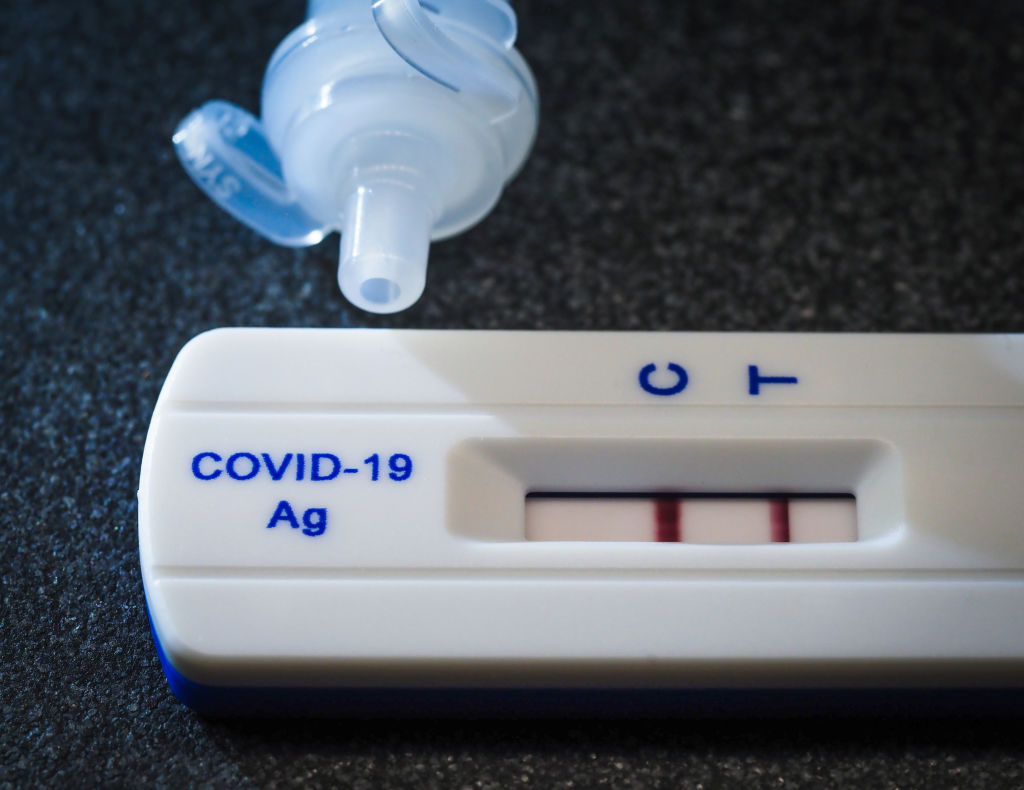
To reach that finding, Hollenbach and her colleagues analyzed the genetic information of more than 1,400 unvaccinated people who tested positive for COVID-19 in April 2021 or earlier. Out of those people, 136 did not develop symptoms. (Many got tested because they had to for work or came into contact with someone who had COVID-19.)
About 20% of the asymptomatic individuals had a gene mutation called HLA-B*15:01, compared to only 9% of the people who felt sick when they were infected, the researchers found. And the small group of people who had two copies of the gene variant were about eight times more likely to be asymptomatic than those without any copies of it.
The researchers ran similar analyses in two other groups of patients. Both times, they found that the HLA-B*15:01 mutation was disproportionately common among people who had asymptomatic COVID-19, suggesting it played a role in keeping symptoms at bay.
How? In some people who have the HLA-B*15:01 mutation, the immune system’s T cells seem to use their past experiences with similar coronaviruses, including those that cause the common cold, as training to target SARS-CoV-2, taming it before it causes symptoms.
“We know that SARS-CoV-2 has a lot of similarities with some seasonal coronaviruses,” Hollenbach says. “From very early on, [researchers] thought, ‘Maybe there’s some cross-protection there.’” Her research suggests there is—at least, among people with the right genes.
Still, there are plenty of outstanding questions about asymptomatic COVID-19. For example, only 20% of the asymptomatic people in the study had the HLA-B*15:01 mutation, and it’s not clear why the remaining 80% didn’t develop symptoms—or why the 9% of symptomatic people with the mutation did. One theory: Those who had the mutation but still felt sick might not have been exposed to the right seasonal coronaviruses or mounted a strong-enough response to them to achieve lasting immunity, Hollenbach says.
Hollenbach and her colleagues also focused their analysis on white adults, since there weren’t enough people of color enrolled in the study to draw solid conclusions about how their genes affected their COVID-19 symptoms. She says future research should focus on people of other ancestries to see if the same trends apply.
In the meantime, she says, the findings have important implications even for people born without the HLA-B*15:01’s mutation. If researchers could develop a drug or vaccine that mimics its lightning-fast response, they could theoretically stop COVID-19 symptoms before they start. “Should we be thinking about a vaccine that’s aimed not at preventing infection, necessarily, but preventing symptoms?” Hollenbach says.
The research could also hold clues that help answer another long-standing question: Why have some people never been infected by the virus at all, even after years of widespread transmission? Behavioral choices like wearing masks or limiting contact with others may explain it for some people, but others could have their genes to thank. “I would be shocked if there was not a genetic component,” Hollenbach says, and “I would bet money that HLA is involved.”
More Must-Reads from TIME
- How Donald Trump Won
- The Best Inventions of 2024
- Why Sleep Is the Key to Living Longer
- Robert Zemeckis Just Wants to Move You
- How to Break 8 Toxic Communication Habits
- Nicola Coughlan Bet on Herself—And Won
- Why Vinegar Is So Good for You
- Meet TIME's Newest Class of Next Generation Leaders
Write to Jamie Ducharme at jamie.ducharme@time.com