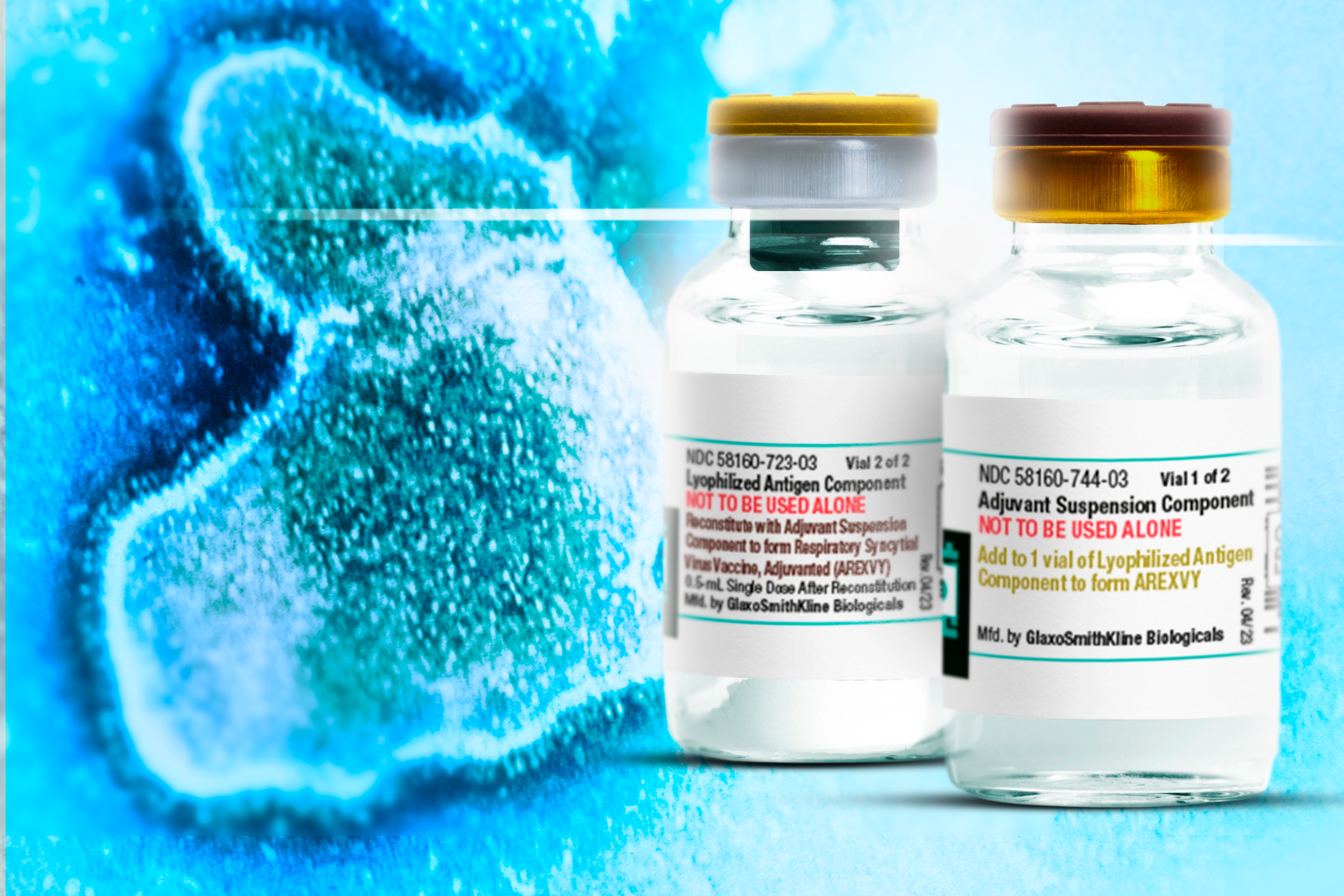
Respiratory syncytial virus (RSV) can dangerously compromise breathing, especially for infants and the elderly. But there has been no vaccine to prevent it—until today. On May 3, the U.S. Food and Drug Administration (FDA) approved the first vaccine against RSV, from GlaxoSmithKline (GSK), to prevent respiratory disease in people ages 60 and older. The Centers for Disease Control’s vaccine committee will make formal recommendations in June about who should receive the vaccine, but GSK says it currently has enough doses to vaccinate eligible people beginning this fall.
In studies involving 25,000 people that GSK submitted to the FDA, the company’s vaccine, called Arexvy, reduced the risk of respiratory disease by 82.6% among those who received a single shot, compared to those receiving placebo. The FDA asked the company to continue studying how long the protection against RSV disease might last to determine if people would need annual vaccinations. The company will also monitor for potential side effects of the shot; two people who received Arexvy and the flu shot on the same day developed a rare inflammatory condition, and one died, while another who received just an Arexvy vaccination developed Guillain-Barre syndrome, a rare immune system condition that can cause muscle weakness and even paralysis.
It won’t be the only shot targeting the virus for long. Pfizer has also submitted its RSV vaccine in older adults for approval, and the FDA has until May 31 to make a decision. Not far behind, Moderna plans to request approval for its RSV vaccine, based on the same mRNA technology behind its COVID-19 vaccine, this year. (Johnson & Johnson-Janssen, which was also testing an RSV vaccine, decided to stop its late-stage trials in March.) In coming months, the companies and FDA will also consider approving a vaccine for young babies from Pfizer, and Moderna is launching studies of its vaccine in pediatric populations.
Getting to this point has been a long journey, but one that has benefited from game-changing discoveries. Here’s how we got here.
More from TIME
The long road to a vaccine
In the 1980s, Paul Glezen, a microbiologist and immunologist at Baylor College of Medicine, made the first important discovery toward creating an RSV vaccine. Doctors knew that while nearly every baby became infected with RSV by the time they were two, only a small percentage became sick enough from their infection to be hospitalized. He guessed that most babies were benefiting from antibodies that they passively received from their mothers, which helped their still undeveloped immune systems fight off the virus. To prove his theory, Glezen collected cord blood from thousands of babies born at Baylor’s maternity hospital, and compared those who ended up being hospitalized for RSV to those who were not. The babies who did not get admitted tended to have high levels of antibodies against the virus, while those who did not had lower levels.
“That was a fundamental breakthrough,” says Bill Gruber, senior vice president of vaccine clinical research and development at Pfizer. “It indicated that if you could get the right antibodies to the babies, they would likely provide protection against RSV.”
That insight turned into an antibody treatment: an injectable shot known as palivizumab, or Synagis. This is currently the only antibody-based therapy for RSV, but it’s reserved for babies at highest risk of developing infections and requires five shots over the course of one viral season.
A vaccine that trains the immune system to fight the virus would have broader impact and could be more widely distributed to every newborn as part of their routine immunizations. But after an early vaccine candidate failed to protect babies and instead led to worse illness—particularly among those who had never been exposed to the virus before getting immunized—development stalled for decades. “That vaccine, which was given to infants, made things worse and set back research years and years,” says Dr. Phil Dormitzer, global head of vaccines R&D at GSK.
Scientists working on another virus, parainfluenza virus, that also causes respiratory disease in babies, first introduced the idea that an effective vaccine against that pathogen should target a specific form that the virus takes, just before it infects a cell. Previous attempts to develop vaccines had targeted the wrong form of the RSV protein—one that the virus made after it had infected cells. By then, the virus had already co-opted the cell’s machinery to make more copies of itself, and had launched a full scale infection—too late for any vaccine to come in and have much effect. Once the idea had been planted with the parainfluenza virus, “we assumed that we could do the same thing with RSV, and that it would be pretty easy to engineer,” says Dormitzer. “But it turned out to be way more difficult, and many frustrating years went by when we tried to do the same thing with RSV, with minor variations, and they weren’t working.”
Then, Barney Graham made a breakthrough discovery in 2013. An immunologist and virologist at the National Institute of Allergy and Infectious Diseases at the National Institutes of Health, Graham had devoted years to unpacking how RSV worked. He focused on understanding how the main RSV protein that sets up a red flag for the immune system was constructed. Graham successfully isolated a version of the protein that the virus made before infecting a cell, and in tests in animals and with human cells, this protein was far more potent in stimulating the immune system than previously isolated RSV proteins.
At Pfizer, Gruber, who was Graham’s undergraduate roommate at Rice University, learned of his friend’s discovery after reading Graham’s description in a scientific journal. The two connected, and Gruber convinced Pfizer to license the technology. The pharmaceutical giant put its scientists to work creating a stabilized form of the RSV protein that targeted not just one strain of the virus, but two—similar to the way different versions of the influenza virus are included in each flu shot—in order to prompt the most wide ranging immune response possible.
GSK relied on its own strategies using recombinant technology to ensure that the target RSV protein did not “flip to a form we didn’t want,” says Dormitzer. The engineering in GSK’s vaccine, he says, has advantages in that scientists can perform quality control to ensure that the RSV protein in the shot is pure and in the proper form, and gives them more control over how the vaccine can activate the immune system.
How RSV vaccines got sidelined by COVID-19
Graham was preparing to launch a trial of his RSV protein in a vaccine toward the end of 2019. But it turned out the first virus his theory would be tested against wouldn’t be RSV, but SARS-CoV-2. Based on his work with RSV to that point, Graham was among the first to realize that the same approach he was testing for a new RSV vaccine could work for the novel coronavirus as well. He asked his boss, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, to allow him to test that idea and develop a prototype COVID-19 vaccine with a form of SARS-CoV-2.
NIAID had partnered with a small biotech in Cambridge, Mass., called Moderna, to test this strategy. Not only did the company place its bets on the genetic code for the same form of the viral protein as Graham, but it also banked on a new way of delivering that information into the body using a genetic material known as mRNA. Scientists at Moderna were convinced that mRNA would serve as a better foundation for a vaccine, since the platform did not require growing any viral proteins but only relied on zeroing in on the right RNA sequence from the virus that would stimulate the immune system.
Graham’s advance allowed the immune system to generate a strong immune response to SARS-CoV-2 that surprised even the most jaded scientists. In the first studies in people, the COVID-19 vaccine was able to neutralize lab versions of SARS-CoV-2 with more than 90% efficacy. Graham’s discovery, coupled with the mRNA platform’s flexibility and speed, set records for vaccine development that will be tough to beat. In under a year, scientists had gone from not knowing what SARS-CoV-2 was to having a very effective vaccine directed against it.
Next steps for RSV vaccines
The success of those shots redirected scientists to bring their other vaccine candidates full circle, hopefully with equally robust results.
Building on the right form of the RSV protein that Graham’s group had identified, GSK scientists super-charged its vaccine for older people, many of whom have waning immune systems and other conditions that that can weaken their body’s defenses, with an accelerant known as an adjuvant, which makes foreign targets in vaccines more attractive to the immune system.
Gruber says Pfizer also focused on developing a vaccine for adults at highest risk of RSV—the elderly—and used the same vaccine to also immunize pregnant women as a way to protect newborns. “Some pregnant women could make antibodies to pass on to their infants, so we needed to figure out how to make every pregnant woman have that opportunity,” he says. In March, the company presented to an FDA panel of outside experts its encouraging late-stage results from human testing among older people. That data showed the vaccine was around 67% effective in reducing RSV illness associated with at least two symptoms of infection, and had 85.7% efficacy in lowering more severe illness associated with at least three symptoms.
Pfizer’s next target will be immunizing pregnant women against RSV in order to protect their newborns. In November 2022, the company announced encouraging results from its late-phase testing of the same vaccine used in older adults that was given to expectant moms. In that study, the vaccine was almost 82% efficacious in reducing the need for medical treatment of respiratory illness in the first 90 days after birth, and 69% efficacious in the first six months. That study is ongoing, and Gruber says Pfizer’s scientists are hoping that vaccine could be given once during pregnancy to protect the newborn. “We knew pregnant women who got infected with RSV made antibodies that they passed on to their infants, and we figured out how to give every woman that opportunity with a vaccine,” he says.
Dormitzer says that GSK’s RSV vaccine for older people likely will not be applicable to pregnant women; early trials found a possible safety issue in this population, so the company stopped the study. “If we go with a vaccine directly in children, we would probably not use [the current formulation], because of what we saw in the 1960s,” says Dormitzer. “Right now, focusing on the older populations, we are immunizing people who have all had RSV before, so there is no risk of seeing what happened in the 1960s.”
So far, GSK found that protection from a single vaccination protects older people through an entire respiratory disease season, and potentially up to a year. In coming months, its scientists will know if that protection lasts longer, into a second season. Also coming could be combination vaccines that target pairings of three of the major respiratory diseases that plague older people — flu, COVID-19 and RSV.
Because vaccines are among the most effective ways to prevent infectious with viruses and protect people’s health, these shots could be critical in controlling RSV, not just in the U.S., but around the world as well. “These are transformational products in my view,” says Ruth Karron, professor of international health at the Johns Hopkins Bloomberg School of Public Health. “They will certainly transform what happens in high income countries, and we hope they will be able to transform things globally as well.”
More Must-Reads from TIME
- Why Biden Dropped Out
- Ukraine’s Plan to Survive Trump
- The Rise of a New Kind of Parenting Guru
- The Chaos and Commotion of the RNC in Photos
- Why We All Have a Stake in Twisters’ Success
- 8 Eating Habits That Actually Improve Your Sleep
- Welcome to the Noah Lyles Olympics
- Get Our Paris Olympics Newsletter in Your Inbox
Contact us at letters@time.com