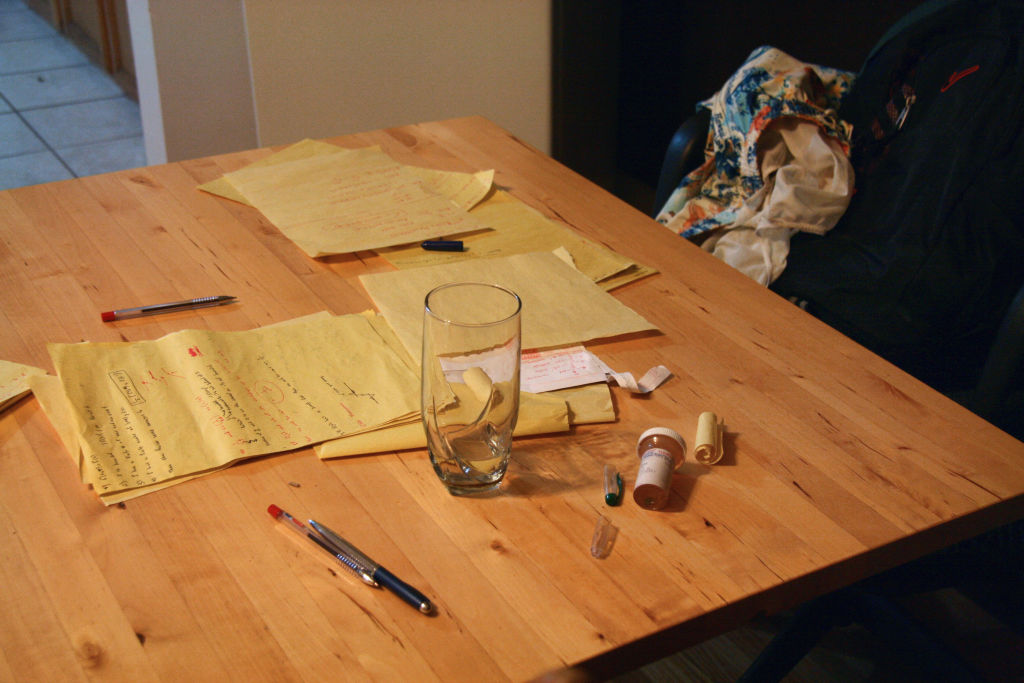
For at least the last six months, Adderall—the stimulant medication commonly used to treat attention-deficit/hyperactivity disorder (ADHD)—has been in short supply in the U.S. That seems to be in part because demand is growing as more people are diagnosed with ADHD, a condition that can make it difficult to focus, remember details, control impulses, or sit still. About 8% more people in the U.S. filled a stimulant prescription in 2021 versus 2020, according to federal data. Other studies suggest ADHD diagnoses are increasing across age groups.
Why? And is that apparent spike in diagnoses cause for concern?
Some experts fear the uptick reflects lax diagnostic standards during the COVID-19 pandemic and a growing trend of people becoming convinced they have ADHD because of content they see on social media. But at the same time, some experts say the rise may be a long overdue sign that people from groups historically under-treated for ADHD are getting the care they need.
“There’s a risk of under-diagnosis, and there’s a risk of over-diagnosis,” says Dr. Lidia Zylowska, an associate professor of psychiatry and behavioral sciences at the University of Minnesota Medical School and an adult ADHD specialist. It’s not yet clear which—if either—is happening with ADHD.
A perfect storm
By federal estimates, about 10% of U.S. children and 8% of U.S. adults ages 18 to 44 have been diagnosed with ADHD during their lives.
ADHD diagnoses have been rising for decades, and some data suggest there’s been an additional increase since the pandemic began. A recent analysis from the health records company Epic found that 0.6% of the millions of U.S. patients in its database were diagnosed with ADHD in 2022, compared to about 0.4% in 2019. An analysis from health care research firm Trilliant Health also found that more adults ages 22 to 44 sought care for ADHD in 2021 versus 2020, and that 15% more adults in this age group had an Adderall prescription in the middle of 2021 compared to a year earlier.
For some people, the pandemic may have been a tipping point from manageable concentration issues to those that required professional help, says Margaret Sibley, an associate professor at the University of Washington School of Medicine and an ADHD specialist. Many people were forced out of their normal work and school routines, stressed, sleeping less, and scrolling social media more—a perfect storm of distraction that may have exacerbated symptoms in some people.
The pandemic also opened up new avenues for getting an ADHD diagnosis. Thanks to relaxed regulations on both telehealth and remote prescription of controlled substances, it became easier than ever to get diagnosed with and treated for ADHD online. Plenty of people benefitted from that increased access to care, but it also raised concerns about over-treatment and over-diagnosis—particularly when teletherapy startups began writing so many stimulant prescriptions that federal investigators raised alarm bells. (Many teletherapy services have stopped prescribing stimulants like Adderall.)
ADHD content on social media only added to concerns about over-diagnosis. Some startups offering remote ADHD care advertised their services on platforms like TikTok, adding to a chorus of social media posts (many misleading, according to one 2022 study) about common signs of ADHD, such as forgetfulness and difficulty focusing.
For some people, those videos led to appropriate diagnoses. But since almost everyone has experienced focus, memory, or attention issues at some point, it’s easy to jump to a self-diagnosis that may not be correct, says Dr. Jessica Gold, an assistant professor of psychiatry at the Washington University School of Medicine in St. Louis who has studied ADHD diagnosis trends. “That’s okay if you take that information to a doctor who feels comfortable sussing it out,” she says, but not all clinicians are well-versed in ADHD detection.
To diagnose ADHD, clinicians usually rely on the patient’s description of their symptoms at various phases of their life, reports from people they know, or, more rarely, neuropsychiatric testing. Not all clinicians are properly trained to do that assessment—which goes back to a long misunderstanding of what ADHD is and who it affects.
A misunderstood condition
“If you ask a person to close their eyes and imagine someone with ADHD, I’d wager nine out of 10 times they’re going to think of a little boy running around a classroom, making lots of noise, and getting into trouble,” says Julia Schechter, co-director of the Duke Center for Girls and Women with ADHD.
But the reality, Schechter says, is that people of all ages and genders experience ADHD. It’s just that girls and adults have historically been missed.
While boys typically experience hyperactive symptoms of ADHD, including impulse control and excess energy, girls are more likely to experience internal symptoms, like trouble focusing or listening, that are harder to notice. Adults with ADHD may slip through the cracks for similar reasons, Zylowska says: hyperactivity tends to improve as someone gets older, but inattention and other symptoms can persist.
Many mental-health professionals aren’t comfortable diagnosing those issues, in some cases because they’re nervous about prescribing stimulant medications, Zylowska says. Stimulants can be abused and come with potential side effects, including insomnia, loss of appetite, nausea, and headaches. They can also worsen anxiety—which is important, since anxiety can either accompany or be mistaken for ADHD, Gold notes.
Sibley says that’s one of her primary concerns about potential misdiagnosis of ADHD: the possibility that people have other conditions that are being missed. Plenty of mental and physical conditions can lead to concentration or behavioral issues that look similar to ADHD, and many clinicians aren’t prepared to sort through the differences.
That’s in part because ADHD has received less research funding than other mental-health conditions over the years, Sibley says, so clinicians simply know less about it. In 2022, the National Institutes of Health granted $78 million for the study of ADHD, compared to $655 million for depression.
“Adult psychiatrists, historically, have had no training in ADHD because for decades it was seen as just a childhood disorder,” Sibley says. “They aren’t even asking the right questions.”
That is starting to change: Epic’s analysis found that almost twice as many women ages 23 to 49 got new ADHD diagnoses from 2020 to 2022, and diagnostic rates have also risen among girls in recent years. People of color are also being diagnosed more frequently. Those trends suggest clinicians are getting better at detecting ADHD among more diverse patient groups, Schechter says.
For someone whose symptoms have been downplayed or ignored for years, finally getting an accurate diagnosis can be a “life-changing experience,” Schechter says. “To find out that the difficulties they’ve experienced their entire lives are due to a biologically based condition is such a relief.”
In that respect, Sibley agrees, the uptick in diagnoses may be a good thing, a signal that people are at last getting the care they need—but it’s hard to say for sure, since it’s not clear how many people have been appropriately versus inappropriately diagnosed.
“It’s a weighing of pros and cons,” she says. “Which is the lesser of two evils: giving an incorrect ADHD diagnosis, or having somebody who should be diagnosed with ADHD missed?”
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Write to Jamie Ducharme at jamie.ducharme@time.com