The U.S. Centers for Disease Control and Prevention (CDC) is tracking the rise of a deadly, treatment-resistant fungus that’s causing outbreaks in a growing number of health care facilities across the country.
New data compiled by a CDC research team, published Mar. 21 in Annals of Internal Medicine, show that Candida auris infections have increased dramatically in the U.S. in recent years. In 2021, national cases reported by health care facilities increased by 95%, and from 2019 to 2021, 17 states reported their first case. With infections recorded in a total of 28 states and the District of Columbia, these numbers suggest that current disinfection and safety measures at care facilities may not be sufficient.
Experts do not currently view C. auris as much of a threat to the wider population, since most healthy people are not at risk for severe infections, which tend to spread in hospital settings. But there are fears that it could someday evolve to become one.
The first U.S. case of C. auris infection was reported in 2016, and though travel later brought it to a number of states, “early on, we weren’t seeing such such a dramatic increase,” says Meghan Lyman, a medical officer in the CDC’s mycotic diseases branch and first author on the paper. “That gave us some hope.” Things changed in 2019, she says, when an influx of states reporting outbreaks made it clear that the threat was here to stay. “We’ve realized it’s just a really fragile situation.” A 2022 study described a concurrent increase in European outbreaks, and the CDC says that infections have occurred in more than 30 countries worldwide since the fungus first emerged in Japan in 2009.
Read More: Deadly Fungal Infection Emerged Because of Global Warming, Study Says
More from TIME
The new findings may also reflect the impact of the COVID-19 pandemic. In 2020, eight states reported their first cases of C. auris, more than in any other year. CDC scientists believe that crowded conditions in hospitals—particularly those facing shortages of staff, equipment, and PPE—contributed to the spread of the fungus. Infections are rare but serious—mortality rates are about 30%—and symptoms can include fever and chills, followed by organ failure.
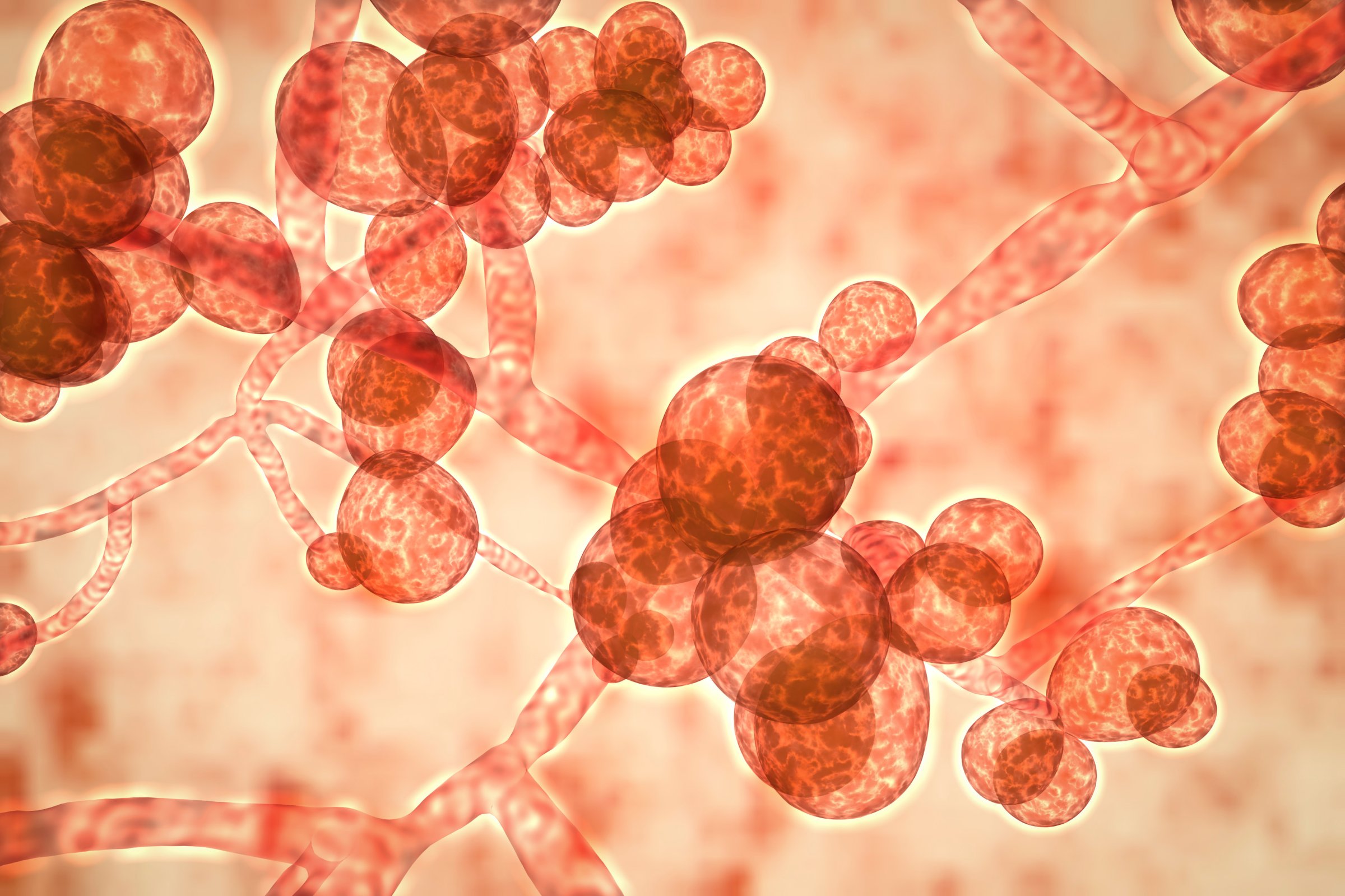
Most fungal infections, both mild and serious, are caused by one of the hundreds of types of Candida yeasts. Some types of Candida live peacefully within our bodies—a yeast infection, for instance, is simply an overgrowth of one of these helpful species. C. auris is one of the more dangerous types, but for most healthy people, the fungus will temporarily colonize the skin without causing any illness or issues; without testing, you’d likely never know it was there. This type of colonization often resolves naturally, thanks to existing fungi in the normal skin flora that eventually rebalance and take over. The danger arises when C. auris finds a way into the body through a wound or other opening, particularly if somebody is weakened or immunocompromised.
This helps explain why the CDC’s data come almost entirely from health care settings. Another factor is that people who are already in these settings are more likely to be tested for it, following a bad infection or death. “When the first case pops up, often it’s a clinical case, because people might not be looking for it,” explains Lyman. If you’re headed to the hospital and fearful of infection, “you can always ask, as soon as you enter, if they’re screening for C. auris,” says Johanna Rhodes, a researcher at Imperial College London (who was not involved with the study). In an ideal world, she says, hospitals would be screening all patients upon entry. While no state yet requires hospitals to test this thoroughly, several have either recommended it or undertaken county-level projects to make widespread screening more feasible.
Most fungi capable of infecting humans pose threats to certain body systems. Some can infect the lungs, others the skin, and some even seem to affect mental health. This particular species of Candida affects the bloodstream, and infections like those caused by C. auris, “are similar to sepsis,” explains Rhodes. “But it’s harder to treat.”
C. auris is resistant to antifungal medications, which makes it unique among fungi. “If you look across all species of Candida, only about 7% of all isolates [individual cell samples trapped and regrown in a lab] are resistant to antifungals,” says Shawn Lockhart, director of the CDC’s fungal reference laboratory and an author on the paper. “Now, all of a sudden, we’ve got this bug where 85-90% of all isolates are resistant.”
Read More: Why Fungi Can Be Good
Generally, a drug-resistant fungus can evade one of the the three major types of antifungal medications. But C. auris is pan-resistant, which means that all three treatments are weakened or ineffective against it. Scientists have also tracked the drug resistance of C. auris over time, and the fungus has evolved dramatically in a short period of time—which worries experts. “I can only think of one other report of a pan-resistant Candida,” he says. “The difference is that it was never resistant to all three antifungals at the same time.”
C. auris also has an unusual ability to stick around. The fungus is able to form biofilms, explains Rhodes, “which is essentially like having a suit of armor or Iron Man suit. It allows it to persist in the environment—it makes it super sticky to surfaces, and it can resist disinfectant.” In a 2015 study, Rhodes found that C. auris was resistant to most of the disinfectants used by the U.K.’s National Health System at the time, and pushed for recommendations to be adjusted. This “stickiness” allows C. auris to cling to medical equipment like ventilators and catheters in a way that other infectious agents can’t.
To help reverse the rise of the fungus, the first step should be to find a way to reduce the amount of C. auris that patients harbor, Lockhart says.“The key is getting the colonization low enough so that it’s not transmitting to other patients, to protect the people who are most at risk.” Doing this requires minimizing spread in the first place, which she says can be done by adequately maintaining sterile hospital environments and cleaning procedures.
Lyman is confident that measures can be taken to slow the spread and reduce case numbers in the U.S. “We’ve actually seen a lot of facilities in areas that have prevented and even stopped transmission,” she says. The key, she says, will be “really rigorous infection control and good communication.”
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com