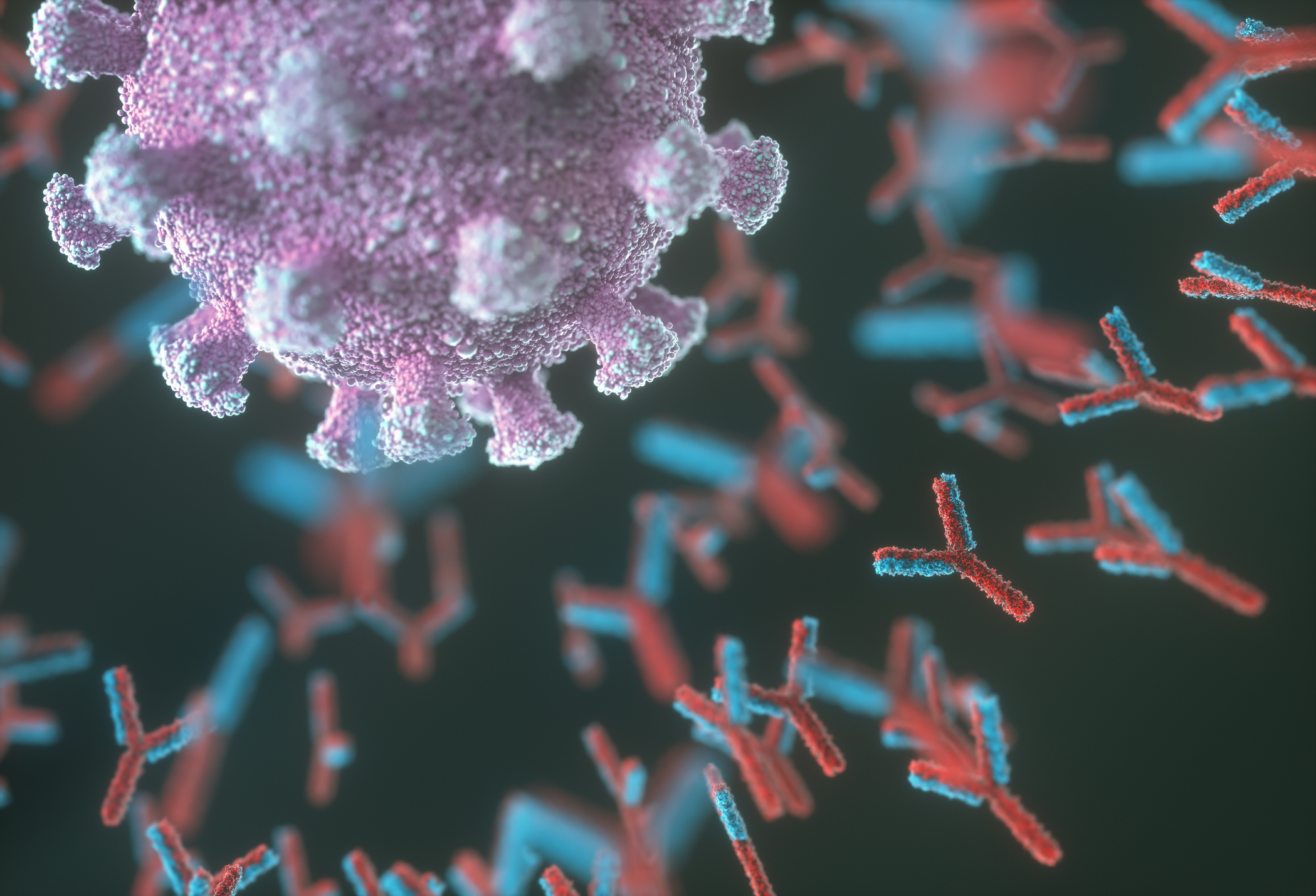
As SARS-CoV-2 continues to evolve, knowing your immunity status—both from vaccines and from infections—will become increasingly important.
COVID-19 antibodies are the best proxy for disease immunity. But they currently require a health care provider to order the test, which has to be performed at a pharmacy or doctor’s office. The sample is then sent to a lab to analyze—all of which takes time, making the process inconvenient and too burdensome for most people.
Researchers at Johns Hopkins have found a way to potentially make antibody testing much more accessible. They developed a method to use widely available and relatively inexpensive glucometers—small devices that read blood sugar levels from a finger prick—to detect SARS-CoV-2 antibodies.
In a paper published in June in the Journal of the American Chemical Society, the research team described how they developed a way to attach SARS-CoV-2 antibodies to sugar and then have the glucose reader measure those sugar levels, which reflect the antibody levels.
“We can manipulate the contents of the test strip to see if we can better understand where that immunity is coming from, and how long it is lasting,” says Dr. Netz Arroyo, the paper’s senior author and assistant professor of pharmacology and molecular sciences at Johns Hopkins.
While antibodies don’t make up the entire human immune response to a virus, they are an important window into the protection people build. Antibodies are generally the first line of defense against a microbe, and once antibodies are generated, then other immune cells, including T cells, jump in to broaden and strengthen the response.
Arroyo was inspired to develop the system after remembering a 2011 paper he read as a graduate student in 2014 describing a similar system. As the pandemic unfolded in 2020, testing was slow and cumbersome, leaving public-health officials blind to how much virus was circulating and how much immunity people were developing. “The idea of using a glucometer immediately came to mind,” he says.
Arroyo and other Johns Hopkins researchers got to work developing a protein that would stick to COVID-19 antibodies and could be placed on a test strip, then creating a way for a glucometer to read the test strip. In the first version, the group used blood samples, but ultimately, a finger prick of blood was sufficient for the test, Arroyo says. The researchers are exploring ways to make the test even more accessible by using other samples such as saliva or swabs of the mouth, which also contain antibodies.
Another big advantage of the system is that it’s generalizable to any infectious agent; the scientists just need to change the target to which the sugar binds. “We wanted to innovate a way that would not only impact this pandemic but future epidemics or pandemics as well,” says Arroyo.
That means the test can also be used to measure monkeypox antibodies and provide doctors with valuable information about how well the vaccine, Jynneos, is working, Arroyo says. The vaccine was approved based on limited information on monkeypox in people—and it’s now given in a different way in order to stretch supply—so being able to easily track antibodies in vaccinated people will give scientists a better understanding of efficacy and how quickly people become protected.
Information about SARS-CoV-2 immunity could become more important in coming months and years, as the world learns to live with COVID-19. Understanding how long protection lasts after each infection or booster dose will help health authorities provide better advice about how frequently shots should be given. Because the test can also be tweaked to detect different variants, health experts can also get a better handle on whether people’s protection from vaccines is effective against the most recently circulating variants.
To detect the antibodies, the researchers’ system now requires three steps, each of which involves treating the blood to different reactions. But the researchers are working on ways to streamline the process to make it similar to the one-step process that the at-home COVID-19 tests use. The university’s office of technology ventures will license the test for companies interested in developing it further.
“The goal is to better understand immunity to COVID-19 and other diseases,” says Arroyo. This type of test is a “powerful tool to monitor what is happening in our population, and can inform policy decisions.”
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com