Until recently, polio had been a relic of history in the U.S. Once a scourge that paralyzed or killed up to tens of thousands of children every year, the U.S. declared the disease officially eradicated in 1979, thanks to widespread vaccination.
But polio is back. On July 21, the New York State Department of Health announced a case of polio in an unvaccinated man in Rockland County. Poliovirus has since been found in wastewater in both Rockland and neighboring Orange County, as well as in New York City.
The development has led to justified alarm. “Even a single case of paralytic polio represents a public health emergency in the United States,” write a group of researchers in a report published Aug. 16 in the Morbidity and Mortality Weekly Report. The bottom line is that anyone who is not fully vaccinated against the disease should get up-to-date on the shots immediately. Here’s what to know about what polio’s re-emergence in the U.S. means for your health.
A brief recent history of polio
As recently as 1988, polio was a worldwide menace: endemic in 125 countries and causing an average of 350,000 paralytic or lethal cases each year, according to the World Health Organization (WHO). It was that year that the World Health Assembly established the Global Polio Eradication Initiative with the goal of wiping out the disease, just as smallpox had been officially eradicated in 1980.
The means to the end of polio would be the same as it was for smallpox: worldwide vaccination. The strategy has worked extraordinarily well. Today, polio is endemic in just two countries—Afghanistan and Pakistan—which have seen just 18 cases between them so far this year, according to the Initiative. But there are problems with that overall success story, and they involve the vaccination campaign itself.
What is vaccine-derived polio?
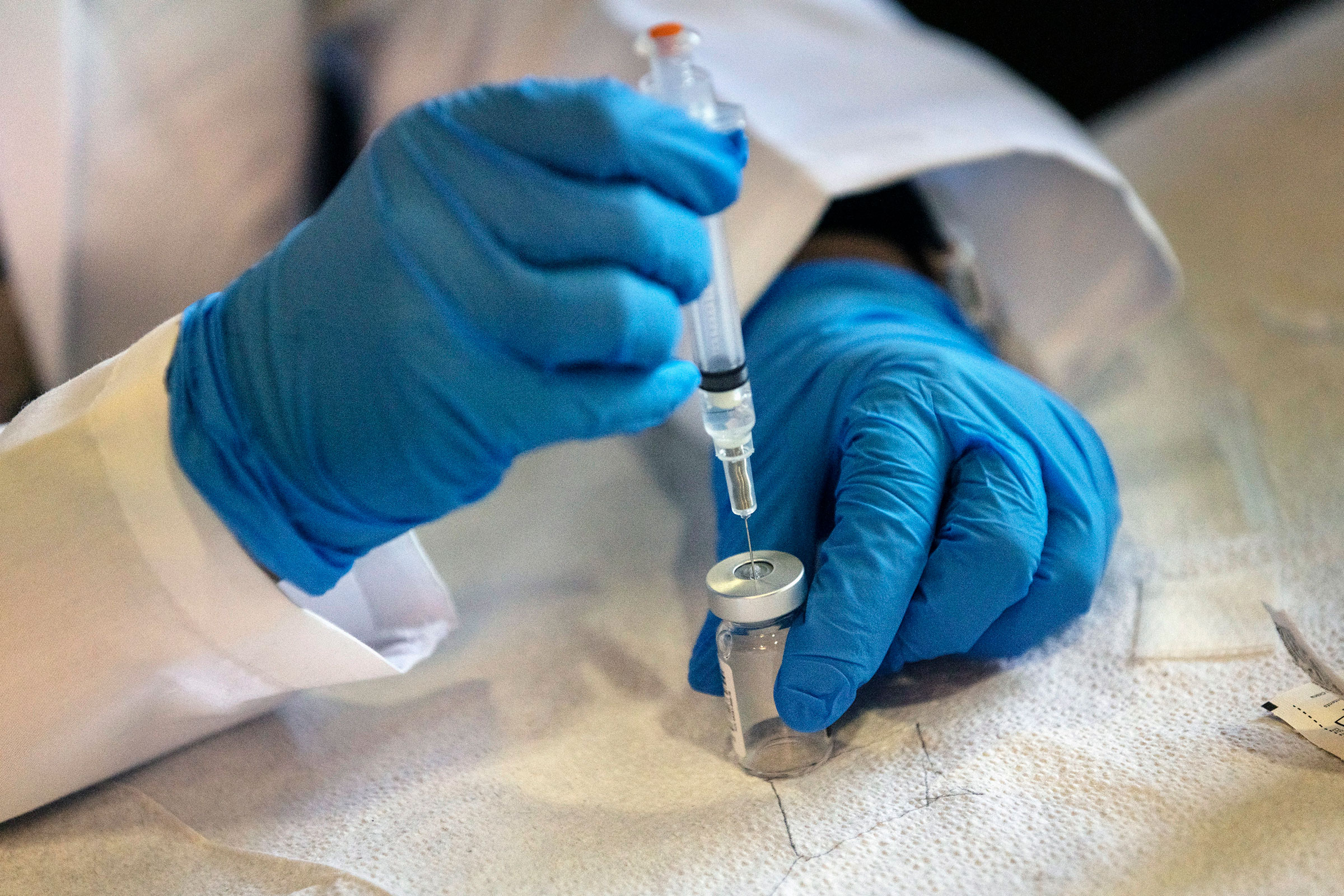
There are two types of polio vaccine: the oral polio vaccine (OPV), which, as its name suggests, is administered by drops to the mouth; and the inactivated polio vaccine (IPV), which is administered by injection. The IPV uses a killed poliovirus to familiarize the immune system with the disease and prime it to react if it ever encounters a living virus. The OPV uses an attenuated virus—weakened to the point that it can do the same work of priming the immune system without actually causing the disease.
The big advantage of the OPV is that it is cheaper and much easier to administer, making it the vaccine of choice for mass inoculation campaigns. The disadvantage is that on exceedingly rare occasions, the weakened virus can revert to virulence, causing the disease in the person who received the drops or allowing the revived virus to be shed in feces of the infected person and circulate in wastewater—leading to the possibility of so-called vaccine-derived polio in others.
The reversion to virulence is rare. Since 1988, an estimated 18 million cases of polio have been prevented by vaccination, and 1.5 million lives have been spared, according to the U.S. Centers for Disease Control and Prevention (CDC). Since 2000, reports UNICEF, 10 billion doses of OPV have been administered worldwide. Measured against those numbers, vaccine-derived polio is low-risk, with a total of 540 global cases so far this year—not including the U.S. case—and a recent peak year occurring in 2020, when 1,100 cases were reported globally. Typically, there are far fewer cases in a given year.
To eliminate the problem domestically, the U.S. stopped using the OPV in 2000 and switched over to the IPV exclusively. But that doesn’t prevent vaccine-derived strains from being imported by travelers from overseas, or by a U.S. resident who traveled internationally, picked up the virus from someone who had received the OPV, and brought it back home. Typing of the virus found in the Rockland County man showed that it was indeed a vaccine-derived strain that caused the disease.
No matter how the virus got here, it is now among us—and it is by no means necessarily limited to the water supply in just three New York regions. If a traveler could bring it into one state, other travelers could carry it anywhere.
“The fact that we’re finding it in wastewater tells you it’s more common than people appreciate,” says Ian Lipkin, professor of epidemiology at Columbia University’s Mailman School of Public Health. “We’re looking at the tip of the iceberg.”
Adds virologist Vincent Racaniello of the Columbia University School of Medicine: “I suspect it’s already in many, many places in the U.S. In fact, I think that if we look in every major city in the U.S., we will find vaccine-derived polio in the sewage for sure.”
Polio vaccination rates are frighteningly low
Vaccine guidelines call for children to receive three polio shots by age two to be considered fully vaccinated. But polio vaccine uptake in the U.S. falls short. In Rockland County, just over 60% of eligible children have received their three doses. (These rates vary wildly within the county; in one zip code, only 37% of children are vaccinated according to the Aug 16 report.) In Orange County, less than 59% of children are fully vaccinated. In New York City, the rates are much higher, at about 86%, but the average varies by borough, with Manhattan reaching 91% and Brooklyn trailing the other boroughs at 81%. Statewide vaccination rates are just below 79%.
Nationwide, the figures are higher, with 92.6% of children fully vaccinated by age two, according to the CDC. But here, too, there are local differences; for example, just 79.5% of kids in Oklahoma, along with 80.3% in South Carolina, are fully vaccinated. That worries experts because every unvaccinated child is at risk of becoming a polio victim—and a reservoir for the virus. For every case of paralytic polio, up to 200 other people are likely infected who either show no signs of the virus or who have mild cold- or flu-like symptoms. Every one of them is a walking viral vector.
“The majority of people who are infected with polio have no symptoms,” says Lipkin. “They aren’t even aware that they are infected, but they can transmit the disease.”
Even people who have been vaccinated against the disease with the IPV—which is the only type of polio vaccine used in the U.S.—can potentially shed the virus. The OPV establishes what’s known as gut immunity, meaning that—assuming a person is not among the few who in whom the poliovirus reverts to its virulent state—there is no viral replication in the intestinal system, and therefore there is no infectious virus shed in feces. But the IPV, since it must be injected to be effective, does not provide gut immunity, meaning that if an IPV-vaccinated person picks up a vaccine-derived strain, that active virus can reproduce in the intestines and be shed.
That poses no health risk to an IPV-vaccinated person, but they can unintentionally contribute to the spread of the virus if they come into contact with it. “You do not develop polio” if you have the IPV vaccine, “because once the virus enters your blood, your immune system would take care of it,” says Racaniello. “But the virus can reproduce in your gut and you can shed it and it can end up in sewage that way.”
What you can do to reduce your risk
The reappearance of polio does not necessarily mean that a nationwide spread of the disease is imminent. But it is a wake-up call that unvaccinated children and adults have to get their shots now. “The solution to the problem is just making sure you’re vaccinated,” says Racaniello. “Because if you’re vaccinated, you will not develop polio.”
But the COVID-19 pandemic has laid bare that the wisdom of getting vaccinated against an infectious disease can bump up hard against politics, claims of personal freedom, and unfounded rumors about the safety and efficacy of the shots. Even before the pandemic, there was already a robust anti-vaccine community in the U.S., and that cohort has not gone away. “There are all sorts of bizarre conspiracy theories that have been put forward by one group or another,” says Lipkin. “It’s a huge problem.”
The good news is that both polio vaccines are remarkably effective and long-lasting. If people received a full course of either vaccine as children, they do not need to get a booster now. “Anyone who has had a complete polio vaccination series does not need a booster,” says Racaniello. “Immunity to polio conferred by vaccination lasts a lifetime.” This, he stresses, is true whether you received either the IPV or the OPV in childhood.
That doesn’t mean that polio boosters are never necessary. People traveling to high-risk areas, like Afghanistan, Pakistan, or any of the countries that have seen high rates of vaccine-derived polio—such as Nigeria, which is home to 238 of the 540 global cases this year—should first receive a booster, says Lipkin.
For most people though, the re-emergence of the poliovirus in the U.S. does not present a danger, thanks to the simple preventative tool of vaccines. They defeated the disease once before in the U.S., and put to work nationwide now, they can do so again.
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Write to Jeffrey Kluger at jeffrey.kluger@time.com