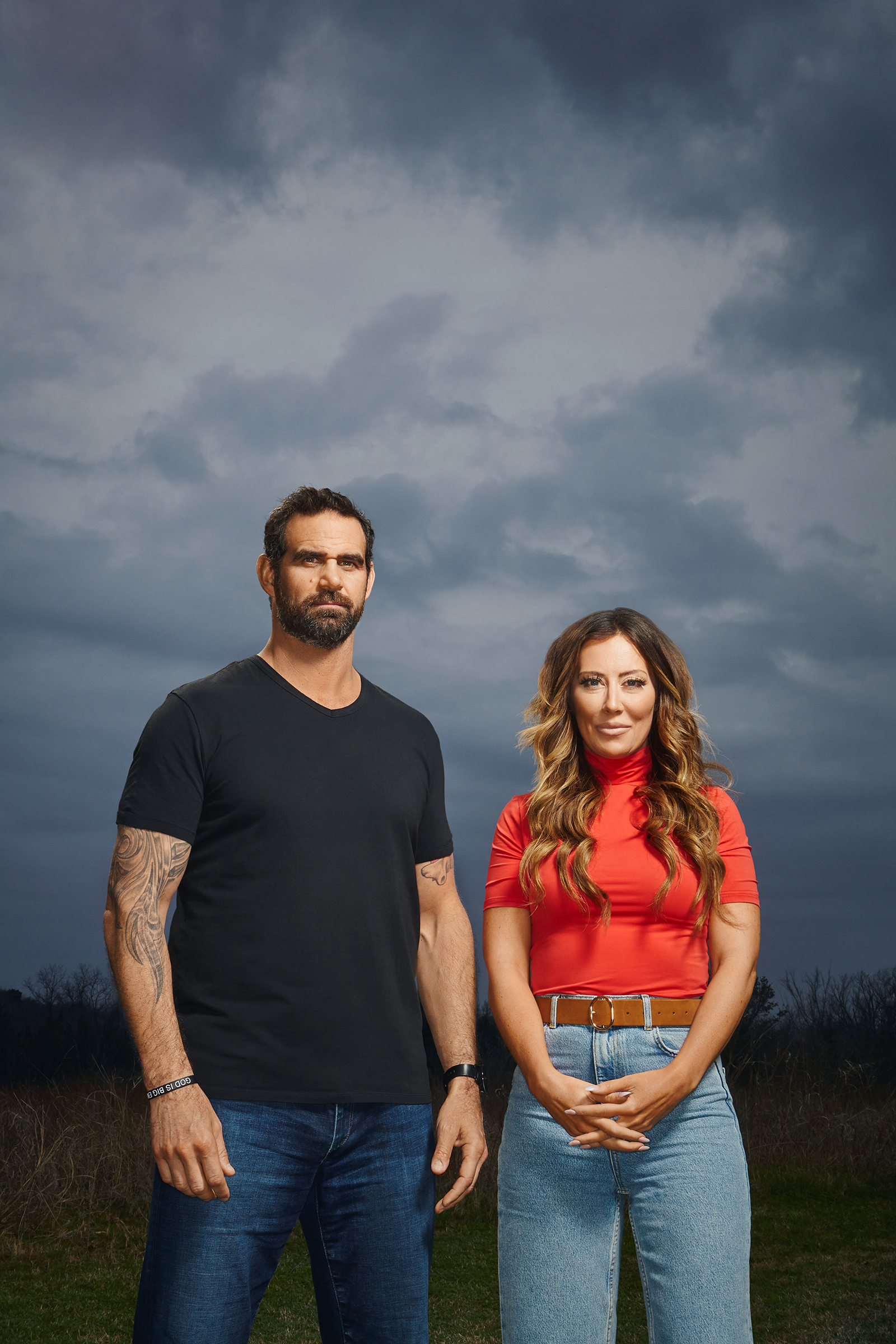
Amber Capone had become afraid of her husband. The “laid-back, bigger than life and cooler than cool” man she’d married had become isolated, disconnected and despondent during his 13 years as a U.S. Navy SEAL. Typically, he was gone 300 days of the year, but when he was home, Amber and their two children walked on eggshells around him. “Everyone was just playing nice until he left again,” Amber says.
In 2013, Marcus retired from the military. But life as a civilian only made his depression, anger, headaches, anxiety, alcoholism, impulsivity and violent dreams worse. Sometimes he’d get upset by noon and binge-drink for 12 hours. Amber watched in horror as his cognitive functioning declined; Marcus was in his late 30s, but he would get lost driving his daughter to volleyball, and sometimes he couldn’t even recognize his friends. Psychologists had diagnosed him with posttraumatic stress disorder (PTSD), depression and anxiety, but antidepressants, Ambien and Adderall didn’t help. He visited a handful of brain clinics across the country, which diagnosed him with postconcussive syndrome after a childhood of football—then a career punctuated by grenades, explosives, rifles and shoulder-fired rockets. But all they offered were more pills, none of which helped either.
Marcus wasn’t the only one suffering in his tight-knit community of Navy SEALs and special-operations veterans. A close friend killed himself, and Amber knew her husband could be next. “I truly thought that Marcus would be the one having the suicide funeral,” Amber says.
There was one last option.
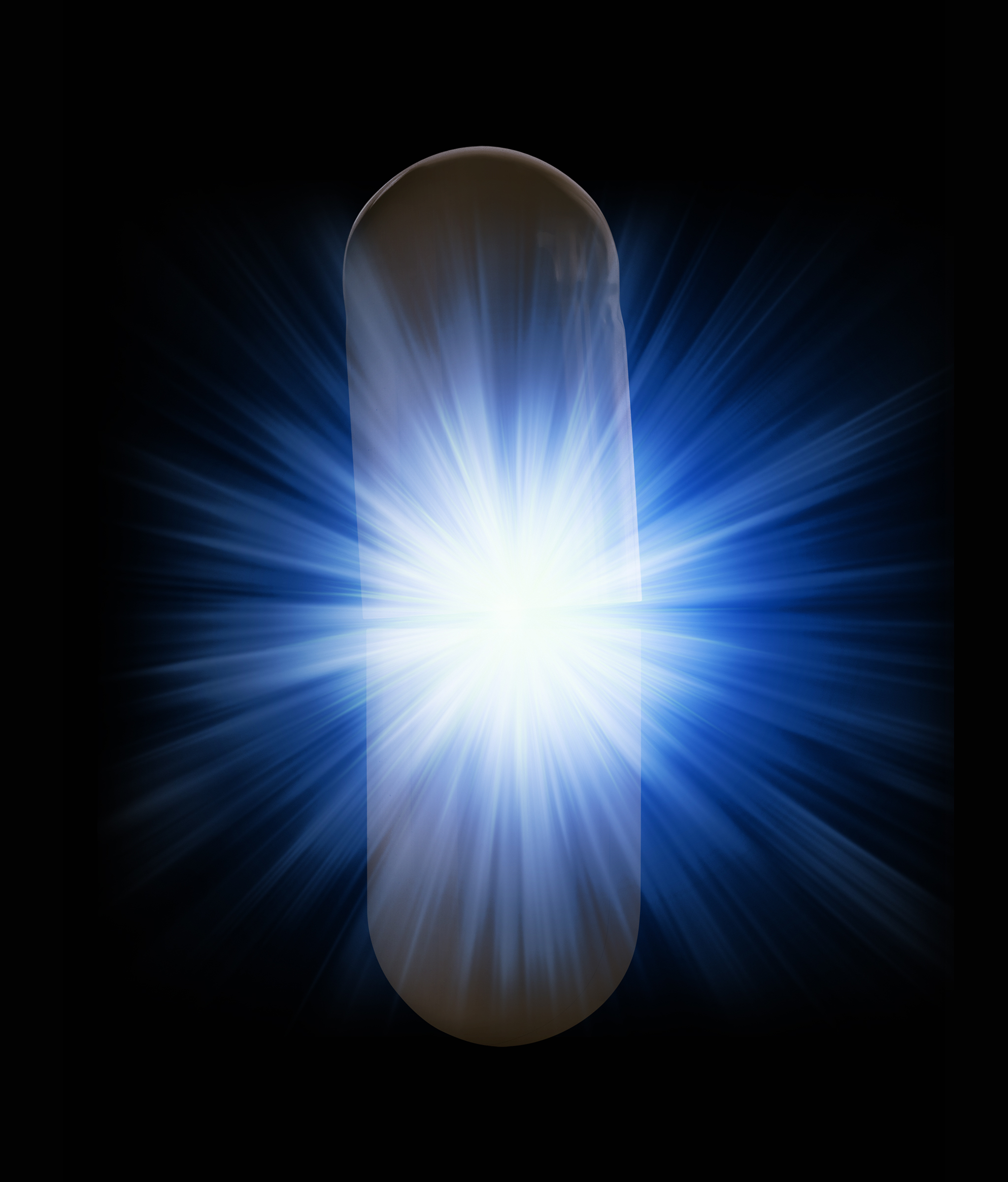
One of Marcus’ retired Navy SEAL friends, who had similarly struggled, had traveled internationally to take ibogaine, a psychedelic drug illegal in the U.S. The ibogaine experience had been transformative for him, and he thought it might be the same for Marcus. “I thought it was crazy,” Marcus says. “How can you take another pill to solve all your problems?” But Amber begged him to try it, and Marcus gave in. On Veterans Day in 2017, Marcus checked into a treatment center in Mexico, popped an ibogaine pill, slipped on eyeshades and noise-canceling headphones, and went on his first-ever psychedelic trip. After an hour or so, he entered a waking dream state and watched a movie of his life play out before his eyes. It lasted 12 hours, and it was awful at times. “Imagine some of the worst experiences of your life,” Marcus says. “You’re going to experience these again.”
Life events flipped through his mind’s eye in rapid fire. Other times, painful memories slowed to a crawl. Marcus saw himself having conversations with his dead father, with buddies he’d lost to the wars over the years, with God. “You can’t hide from the medicine,” he says. “It’s just going to go down there and basically pull up any traumas, anything hiding in your subconscious that may be affecting you that you don’t even realize.”
When it was over, Marcus felt as if he’d finally put down a heavy load he’d been carrying for years. For the first time in a long time, he didn’t want a drink, and he didn’t touch alcohol for a year after. “I was thinking clear. I wasn’t impulsive anymore. I had no anxiety. I wasn’t depressed,” he says. Amber couldn’t believe it, but when she picked him up, she knew she had her husband back. “When he walked into the room, it was as though I was witnessing him the first time I met him,” she says. “His anger and his darkness and his whole demeanor had changed. All of that was gone. He was easy. He was light. He was present. He was happy. It just absolutely blew my mind.”
Once dismissed as a fringe, counterculture vice, psychedelics are rapidly approaching acceptance in mainstream medicine. These drugs uniquely change the brain, and a person’s awareness of experiences, in the span of just a few hours. This fast-acting shift could be useful in mental-health treatments, and research is already supporting this notion. Just one dose of psilocybin, the active ingredient in magic mushrooms, was recently shown to ease depression and anxiety in cancer patients—an outcome that lasted for years after their trip. Researchers are recognizing that psychedelics can provide a radical new approach to mental-health treatments at a time when innovation is desperately needed.
For addiction in particular, the need has never been greater. More Americans died from drug overdoses last year than ever before, aggravated by the COVID-19 pandemic. Weekly counts of drug overdoses were up to 45% higher in 2020 than in the same periods in 2019, according to research from the U.S. Centers for Disease Control and Prevention published in February. Available treatments can’t meet the need. They aren’t effective for everyone, may require long-term adherence and are sometimes addictive themselves.
Ibogaine is one of the most promising psychedelics for addiction. Few people have heard of it, it’s illicit in the U.S., and nobody does it for fun. It’s not pleasant. It could kill you. But for extinguishing addiction—and a range of other issues—many people swear there’s nothing like it. The drug hails from a shrub called Tabernanthe iboga, which is native to Central Africa. Since at least the 1800s, members of the Bwiti religion in Gabon have eaten iboga bark shavings during initiations and coming- of-age ceremonies; those who consume it report visions of and contact with their ancestors and even God. The wider world encountered the hallucinogenic plant in the form of ibogaine, a compound extracted from iboga bark and packed into a pill.
In France, ibogaine was sold and prescribed as an antidepressant and stimulant called Lambarene for more than 30 years until the 1960s, when the government outlawed the sale of ibogaine. But its antiaddictive effects weren’t well known in the U.S. until 1962, when Howard Lotsof—then a 19-year-old completely outside the medical establishment—experimented with it and noticed it wiped out his heroin addiction. It did the same for several of Lotsof’s peers when he organized 20 lay drug experimenters, all in their late teens and early 20s, to try many hallucinogens including ibogaine. Seven people in the group were hooked on heroin at the time. After they took ibogaine, all seven said they were no longer in heroin withdrawal, and five of them lost their desire to use heroin for six months or longer. Ibogaine was the only drug to have this effect. “Suddenly, I realized that I was not in heroin withdrawal,” Lotsof later said of his own ibogaine experience. Nor did he crave it. “Where previously I had viewed heroin as a drug which gave me comfort, I now viewed heroin as a drug which emulated death. The very next thought into my mind was, I prefer life to death.”
Lotsof found ibogaine so helpful that he launched a campaign to get researchers to dig into it more deeply. But pharmaceutical companies didn’t bite. Ibogaine is a naturally occurring plant compound and therefore difficult to patent; plus, nobody knew exactly how it worked, and drug companies historically did not see addiction medications as profitable. In 1970, the federal government classified ibogaine (along with other psychedelics) as a Schedule I drug, declaring it had no medical use and a high potential for abuse. But case studies in which ibogaine had helped heroin users successfully detox—including Lotsof’s New York City group and another from the Netherlands in the early ’90s—were promising enough that one U.S. government agency took notice.
In 1991, the National Institute on Drug Abuse (NIDA) decided to fund animal research into ibogaine; the resulting studies (and later ones) in rodents found that ibogaine reduced how much heroin, morphine, cocaine and alcohol the animals consumed. This work primed the U.S. Food and Drug Administration (FDA) to greenlight a clinical trial of ibogaine in humans for cocaine dependence, but it fell apart in early stages because of a lack of funding and contractual disputes. NIDA abandoned its interest in ibogaine, citing safety as one concern. There still has been no completed clinical trial in the U.S. to test ibogaine in people.
Now, for the first time, some upstart pharmaceutical companies, including ATAI Life Sciences and MindMed, are realizing there’s money to be made here, and they’re racing to develop ibogaine or drugs that act like it. But as they start the long slog of chasing FDA approval through clinical trials—with outcomes far from clear—many people are desperate enough to skip the U.S. and try ibogaine in parts of the world where it’s unregulated.
Plenty of these people have shared their experiences with researchers through case reports and survey data. The success stories sound eerily alike: a single dose of ibogaine can take you on a visual journey of your most significant life events. You’re able to forgive yourself and others for past traumas, and the drug seems to rewire your brain, zapping withdrawal symptoms and extinguishing opioid cravings within hours—with results that can last for weeks, months and sometimes even longer. Unlike buprenorphine and methadone, two common approved medications to overcome opioid addictions, ibogaine is not an opioid substitute. “Ibogaine seems to resolve these signs of opioid withdrawal by a mechanism that is different from an opioid effect, and I think that is what is so interesting about it,” says Dr. Kenneth Alper, a longtime ibogaine researcher and an associate professor of psychiatry and neurology at New York University School of Medicine.
Scientists don’t know exactly what ibogaine does to the brain. There’s some recent evidence—in rats—that ibogaine may increase neurotrophic factors in the brain, which are proteins that encourage neuron growth and plasticity (the ability of the brain to change even in adulthood). These appear to be key in helping the brain remodel to overcome an assault like a substance-use disorder. But since other psychedelics also increase neural plasticity, something more is likely going on.
Human clinical trials for ibogaine and addiction are under way. In October, researchers in Spain began testing ibogaine in 20 people trying to wean themselves off methadone. And in an upcoming clinical trial set to begin in Brazil once the pandemic is under control, researchers at the University of São Paulo will give different doses of ibogaine to 12 alcoholic patients to see if it’s safe and effective at reducing the amount they drink.
But many are not waiting for studies. If there’s even a chance that taking ibogaine will help a person overcome addiction, many are willing to try it. Ibogaine is unregulated in many countries, neither illegal nor approved, and that gray zone has allowed dozens of ibogaine treatment centers to pop up worldwide. Americans desperate to shake their addictions spend thousands of dollars at these clinics, which vary wildly in their practices and treatment standards. Some facilities use licensed physicians and monitor heart activity and other vital signs throughout the trip, while other clinics don’t.
Success rates also vary. Some people stop using drugs completely and stay sober for years. Others die. Because of a lack of controlled ibogaine trials, it’s difficult to quantify the risks, but the threats to cardiovascular health are particularly concerning. The drug may block certain channels in the heart and slow down heart rate, which can cause fatal arrhythmias. In one observational study published in 2018, researchers followed 15 people as they received ibogaine treatment for opioid dependence in New Zealand, where ibogaine is legal by prescription, and interviewed them for a year after. Eight of the 11 patients who completed the study cut back on or stopped using opioids, and depression improved in all of them. One person died during the treatment, likely because of an ibogaine-induced heart arrhythmia.
But how much risk is too much when nothing else works?
Four rounds of rehab hadn’t touched Bobby Laughlin’s heroin addiction. He didn’t believe the hype about ibogaine but figured it was his last shot, so he traveled to a clinic in Rosarito Beach, Mexico. Before the flight, he used heroin—and it was the last opiate he ever took. The most valuable outcome of Laughlin’s 30-hour ibogaine experience was that it let him bypass withdrawals, he says, opening a window of opportunity. “One thing that was made very clear to me was that I had to change my life dramatically after the experience if I wanted to capitalize on it and have long-term sobriety,” he says. Laughlin started a private-equity firm in L.A., then a family. “I’ve been able to establish myself,” he says, eight years later. “All roads lead back to ibogaine as the start.”
Alan Davis, a Johns Hopkins University adjunct assistant professor researching psychedelics, has been hired by several clinics outside the U.S.—including the one Laughlin visited—to follow up with clients to see what, if anything, changed in their lives after the treatment. In 2017, Davis published a study in the Journal of Psychedelic Studies in which he surveyed 88 people—most of whom had been using opioids daily for at least four years—who had visited an ibogaine clinic in Mexico from 2012 to 2015. About 80% said ibogaine eliminated or drastically reduced their withdrawal symptoms; half said their opioid cravings diminished, and 30% said that after ibogaine, they never used opioids again. Ibogaine “is not a magic bullet,” Davis says, but even a short-term disruption of the sort the psychedelic provides can give addicted people the space and time to make needed changes to their environment, behavioral patterns and relationships.
Addiction may be only the beginning. In a 2020 research paper published in the journal Chronic Stress, Davis and his team found that among 51 U.S. veterans who had taken ibogaine in Mexico from 2017 to 2019, there were “very large reductions” in symptoms related to every domain they measured, including suicidal thoughts, PTSD, depression, anxiety and cognitive impairment. “Their improvement [was] way above what we would see with typical currently approved treatments,” Davis says. “Even if you cut these effect sizes in half”—assuming that the data aren’t as accurate as they’d be in a rigorous, controlled trial—”that’s still two to three times more powerful than our currently approved treatments.” More than 80% of the vets surveyed said the psychedelic experience was one of the top five most meaningful experiences of their lives.
“We’re not actually healing problems with medications that we currently have; we’re just trying to treat the symptoms,” Davis says. Psychedelics like ibogaine, on the other hand, seem “to be showing that we might actually be getting below just symptom reduction into a place where true healing can happen.”
Despite intriguing initial data like these, modern pharmaceutical companies until recently had not touched ibogaine. Now they’re interested. ATAI Life Sciences, a three-year-old German biotech company focused on psychedelics for mental health, is trying to develop ibogaine as an FDA-approved drug to treat opioid-use disorder. If clinical trials, which are slated to begin in the U.K. in May, support ibogaine’s efficacy, the company’s hope is that an ibogaine capsule would be used at detox centers in the U.S. “I’m a hardcore neuropharmacologist and physician by training,” says Dr. Srinivas Rao, co-founder and chief scientific officer at ATAI. “I’ve viewed it a little skeptically … but the stories with ibogaine keep surfacing and [keep] being very similar. People seem to get a lot out of this experience.” ATAI is also pursuing noribogaine—the substance ibogaine breaks down to in the body—as a possible addiction treatment.
Fears about how ibogaine affects the heart have scared away most establishment pharmaceutical companies, but Rao calls those worries overblown. “It does hit some of these channels in the heart, and in very uncontrolled settings, it’s certainly been associated with issues of arrhythmia,” he says. “In the context of more controlled settings with medical support, it has not really been associated with any kind of arrhythmia or significant adverse outcome.” Careful dosing and monitoring can lessen risk, Rao says, and trials will eventually uncover ibogaine’s true cardiovascular impact. However, some risk might be worth it in the context of the drug’s potential benefits. “If this were treating acne, of course—this is not a great choice,” he says. But for opioid addiction, which kills about 128 Americans per day, “some degree of cardiovascular risk is probably acceptable.”
MindMed, a U.S.-based company aiming to develop medicines based on psychedelics, is pursuing a synthetic derivative of ibogaine called 18-MC for opioid addiction. “We do see merit in hallucinogenic drugs,” says J.R. Rahn, CEO and co-founder of MindMed. “We just don’t see the merit of ibogaine, because I don’t think anyone wants to take medicine and have the risk of having a heart attack.” The company’s hope is that 18-MC will have the same impact on withdrawal as ibogaine but won’t come with the psychedelic or heart effects. MindMed’s Phase 1 trial in Australia has so far found no adverse cardiovascular effects with 18-MC. Phase 2 trials, to test if 18-MC lessens opioid withdrawal, are expected to begin this year.
Other synthetic compounds that act like ibogaine are on the horizon. In a study published in December in the journal Nature, researchers at the University of California, Davis, engineered a compound that’s structurally similar to ibogaine but less damaging to the heart. It also appears to be nonhallucinogenic, at least in mice. Called tabernanthalog, or TBG, it increased neural plasticity, reduced heroin- and alcohol-seeking behavior, and even had antidepressant effects in rodents; researchers are considering pursuing a study of TBG’s effects on humans.
These innovations are still years off. But in the meantime, Marcus Capone knows that his community of special-operations veterans can’t afford to wait. In 2019, he and his wife Amber started a nonprofit called Veterans Exploring Treatment Solutions (VETS) to fund those who want to receive psychedelic therapies like ibogaine abroad. They’ve funded about 300 veterans so far, with more than 100 currently on the waitlist. VETS is also financing research exploring what ibogaine does to the brains of veterans with symptoms of head trauma.
Marcus hopes that someday, Americans who need it will be able to receive the treatment that, in a single dose, saved his life and gave him a new mission. “This word has to get out,” he says.
More Must-Reads from TIME
- Donald Trump Is TIME's 2024 Person of the Year
- Why We Chose Trump as Person of the Year
- Is Intermittent Fasting Good or Bad for You?
- The 100 Must-Read Books of 2024
- The 20 Best Christmas TV Episodes
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- Merle Bombardieri Is Helping People Make the Baby Decision
Write to Mandy Oaklander at mandy.oaklander@time.com