
The last time most of us gave any thought to antibodies was probably in high school biology, but we’re getting a crash refresher course thanks to COVID-19. They are, after all, the key to our best defenses against SARS-CoV-2, the virus that’s caused the global pandemic. People who have been infected likely rely on antibodies to recover, and antibodies are what vaccines are designed to produce.
Or at least that’s what infectious-disease and public-health experts assume for now. Because SARS-CoV-2 is such a new virus, even the world’s best authorities aren’t yet sure what it will take to build proper and lasting immunity against it. But antibodies are a good bet, since people who get infected and recover from disease generate them both to block viruses or bacteria from infecting cells and to mark them for destruction by an army of immune cells. Lab studies also show that throwing some of those antibodies from recovered patients into lab cultures with the virus seems to neutralize it—a strong sign that these antibodies at least play a part in a good immune response.
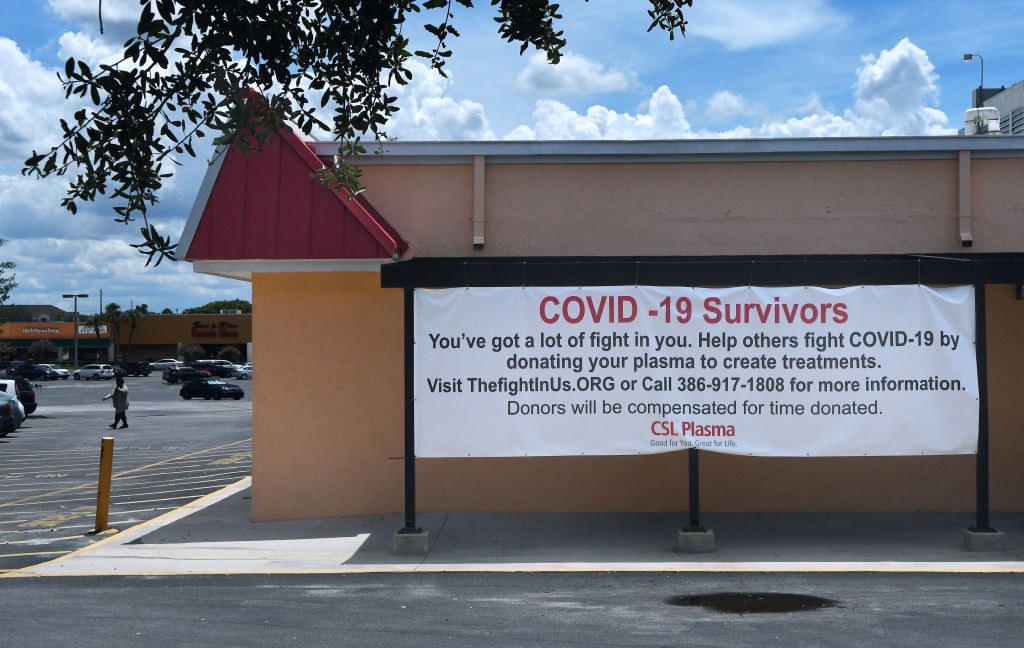
That’s the reason that on Aug. 23, the Food and Drug Administration (FDA) granted emergency use authorization (EUA) for convalescent plasma to treat COVID-19 patients, as it has for another experimental therapy, remdesivir. The decision allows doctors to transfuse plasma donated from recovered COVID-19 patients into currently sick patients in the hopes that some of the immune response against the virus can be transferred as well. The decision was a bit of an about-face, since just days before, the EUA was put on hold after leading infectious-disease and public-health experts, including National Institutes of Health (NIH) director Dr. Francis Collins and White House Coronavirus Task Force member Dr. Anthony Fauci, said that while the early data from critically ill patients who were transfused with convalescent plasma were encouraging, they were not strong enough to justify EUA—yet. They called for more data from ongoing studies to ensure the safety and efficacy of the treatment.
Other doctors, however, who are currently taking part in those trials, believe the EUA is justified. A Mayo Clinic–led trial that is collecting data for the National Convalescent Plasma Study of more than 35,000 patients from 2,800 hospitals who received convalescent plasma through the FDA’s expanded use program showed that people who were transfused with convalescent plasma within three days of their diagnosis had lower mortality rates after 30 days compared with those who received the plasma later, and that people transfused with plasma containing higher levels of antibodies also enjoyed lower mortality rates one month later compared with those receiving plasma with lower concentrations of antibodies. That program allows patients—generally the sickest ones—to receive the transfusions on an experimental basis if no other treatment options are available. “I think there is a crucial role for convalescent plasma right now,” says Dr. James Musser, chair of pathology and genomic medicine at Houston Methodist Research Institute and Houston Methodist Hospital, whose team has transfused several hundred COVID-19 patients so far.
He and others also point to a more than century-long history of success in transferring some type of passive immunity from a recovered patient to a sick one, a technique dating back to the 1918 influenza pandemic, when plasma from recovered patients was used to treat those newly infected. In the years since, the practice has proved itself against other emerging infectious diseases, including other coronavirus diseases like SARS and MERS, as well as Ebola. “There is a very rich literature that is well documented over the years,” says Musser. “Importantly, there is a theoretical reason to think it may work, and pretty good justification that it is probably safe as well.”
Prior to the issuance of the EUA, doctors could use the therapy only if their patients were enrolled in a clinical trial studying the treatment, if they applied for special investigational use of the therapy, or if their hospital is one of the approximately 2,800 participating in the expanded-use program through the National Convalescent Plasma Study. The decision should provide more patients in hospitals around the country the opportunity to receive the treatment.
But one issue with the National Convalescent Plasma Study data—which Collins and Fauci note—is that all of the participants were transfused with plasma from recovered patients, and there is no control group. So, the NIH is also supporting a number of studies comparing antibodies from convalescent plasma with a placebo—including trials focused on treating severely ill patients, as well as those targeting people who are infected but aren’t hospitalized to see if the therapy can potentially prevent their infections from getting that far.
The defensive immune cells in plasma are an attractive target not only for doctors who are desperate for anything to treat their sickest patients, but also for researchers who are eager to mine them for possible drug treatments against COVID-19. Even beyond exploring how plasma from recovered patients can be transfused into sick patients to help them, researchers are also aggressively analyzing this convalescent plasma to isolate the most potent and efficient antibodies and potentially turn them into a treatment that can not only control the disease but maybe even prevent it if given to patients at the right time after their infection.
If they work in preventing some cases of COVID-19, antibody-based therapies could serve as a bridge for protecting populations until a vaccine is approved and distributed. Limited manufacturing capacity and the finite pool of recovered-patient donors make it nearly impossible to produce enough antibody therapies to protect the world’s population at the moment. And even after vaccines are available, they may not provide 100% protection, so antibodies could play an important role in filling any gaps in immunity.
Given convalescent plasma’s track record in treating other infectious diseases in the past, doctors are hoping they’ll have similar success in using it to control COVID-19. “There is not a therapy right now for anyone who is starting to get a [COVID-19] infection,” says Dr. Davey Smith, chief of infectious diseases and global public health at University of California, San Diego, who is overseeing one of the studies looking at outpatients in the U.S. “We have no way to stop it. That’s the reason for the trial.”
How Convalescent-Plasma Therapy Works
So far, early results are mixed on how helpful it is to transfuse sick patients with plasma from recovered patients. One of the first studies, in which 103 patients with severe or life-threatening disease were treated in Wuhan, China, from February 2020 to April 2020, showed little difference in mortality between those receiving the plasma and those not treated, although among severely ill patients, the plasma recipients were 23% more likely to improve over 28 days than those not receiving plasma. But the study was stopped early as cases began to wane in the country.
The early results from the Mayo-led analysis, however, are more encouraging—as are those from another recent study of 136 patients treated in Houston from March to July. In that trial, those randomly assigned to receive convalescent-plasma transfusions had lower mortality after 28 days compared with those not receiving the plasma; transfusion within 72 hours of admission to the hospital showed the most dramatic effect on mortality rate.
The seemingly contradictory data could be due to a number of factors, the most important of which is the fact that each person is capable of making hundreds of trillions of antibodies to various viruses and bacteria and other pathogens they may encounter. At any given time, our immune systems are busy churning out billions of antibodies, largely based on what bugs we’re currently encountering and which bugs we’ve battled in the past. Some people are able to make strong antibodies against SARS-CoV-2, while others may produce slightly less potent ones, and how effective the transfusions are depends on how potent the antibodies happen to be. So which ones are the best for targeting SARS-CoV-2?
The idea behind convalescent plasma is that you don’t actually have to know. Instead, you assume that if someone has recovered from the infection, then their plasma is awash with enough of the right antibodies to take care of the virus.
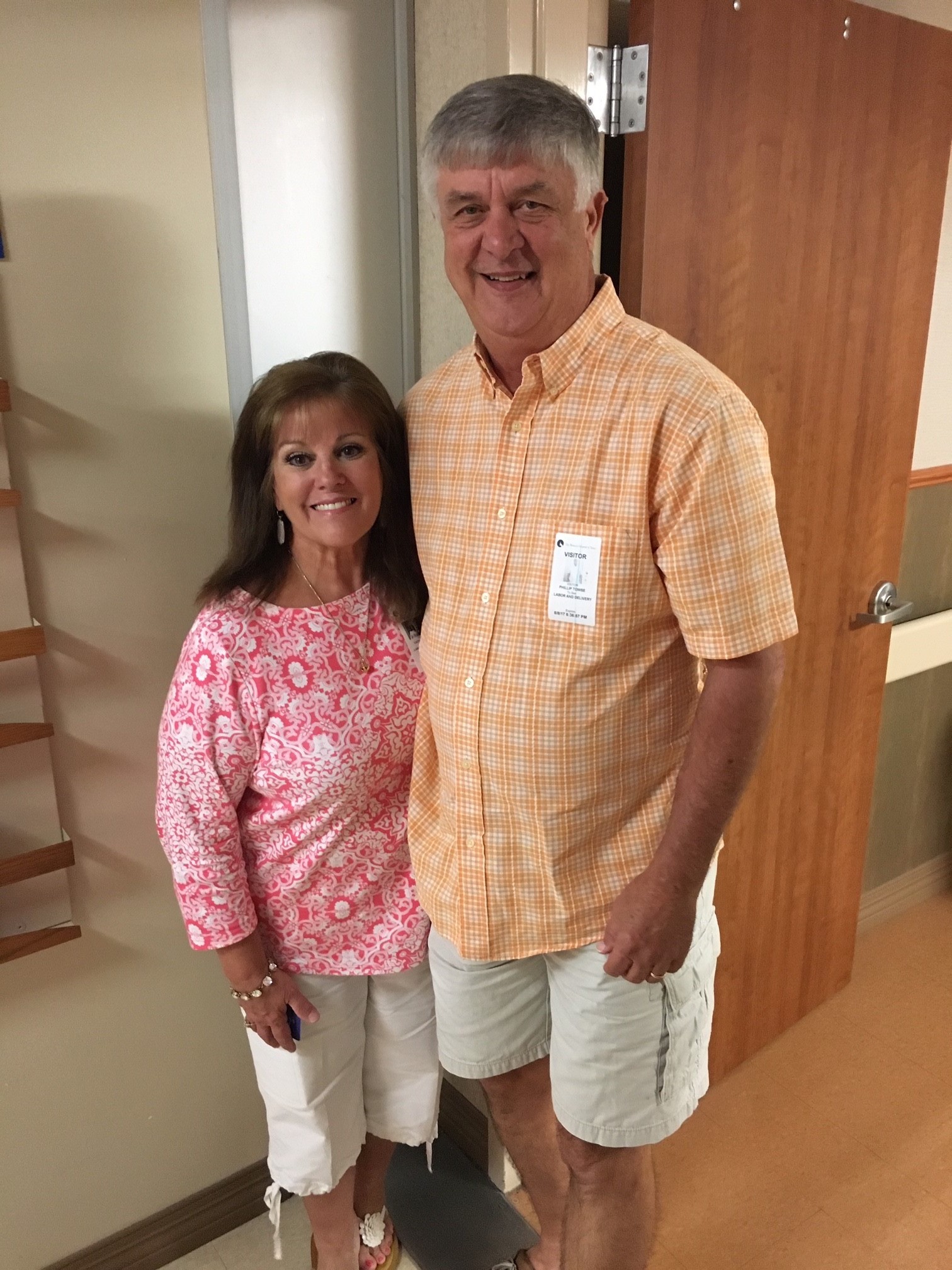
That’s presumably what helped Phil Towse. On April 24, the 68-year-old was at work as a detention officer in the Harris County Sheriff’s office near Katy, Texas, when he started feeling feverish. He got tested the following day, and three days later he learned he was positive for COVID-19. His concerned daughter bought an oximeter to measure his oxygen levels, and when they dropped enough that he could no longer think clearly, his wife took him to the emergency room. Towse wasn’t aware, but the doctors learned he already had pneumonia in both lungs. “I was really close to being put on a ventilator,” he says. “I was a sick dude.”
Towse was treated at Houston Methodist West, which is part of the Houston Methodist system, where doctors had been carefully watching the surge in cases that had recently overwhelmed health care teams in New York City, and were preparing for a similar wave. So, “we decided to move forward aggressively with the convalescent-plasma approach,” says Musser. “Like everybody else, we realized there really weren’t good alternatives available at that time.”
On March 28, Musser and his team performed the first two COVID-19 convalescent-plasma transfusions at an academic center in the country. He and his team worked hard to educate and recruit donors from the area who had recovered from COVID-19, including Daniel Knight, a Houston attorney. Knight’s COVID-19 experience began in the middle of March with a sore throat that he attributed to allergies. A couple of days later, he developed a fever and started coughing. At the advice of his doctor—who is on the faculty at Houston Methodist Hospital—Knight got a COVID-19 test and immediately isolated himself from his wife and two children in a room above the garage, even before getting the results back.
That caution paid off, since it took another two weeks before he received the results. “I was really sick for five or six days with all the symptoms of COVID-19,” he says, including fever, coughing, a rapid heart rate and shortness of breath. Knight was fortunate, however, in that he never got sick enough to need hospitalization, and after he recovered, he decided to donate his plasma. By that time, Houston was in the middle of a peak in cases, and “it was all hands on deck,” says Knight. “Anything I could do to help—I was going to give until I ran out of blood or they told me you can’t give any more. It was really an easy choice for me to donate because I could very easily have been one of those people who was in the ICU. I could have been one of those people who was on a ventilator.”
Towse benefited from donors like Knight; soon after his wife brought him to the emergency room, doctors informed them that he was a good candidate for the plasma treatment. “One of the things that swayed our decision to try it was that we read that in order to qualify for the plasma treatment, you had to either already be so sick that they were afraid you weren’t going to make it, or that you were trending on that path,” says Towse’s wife Cathye Jo. “There weren’t a lot of other options.”
At 3 a.m. on May 4, Towse was roused by the nursing staff and transfused with plasma that had been donated by someone who had recovered from their infection and was a blood-type match for him.
The next day, he says, “I sure did feel better.” Three days later, he was discharged. His doctors will never know exactly which antibodies from his donor contributed to his recovery but it’s enough to know that they likely did. That’s the advantage of plasma—it’s rich in a number of different antibody cells that likely find different ways to block or thwart SARS-CoV-2 from attaching to healthy cells in the body and infecting them.
So far, more than 72,000 people with COVID-19 have been transfused with convalescent plasma, and studies are ongoing to monitor how effective the antibodies were in batting the virus. Most data from the past few months of the pandemic have come from severely ill patients like Towse, including those who are on ventilators in the ICU.
Musser is overseeing the trial of convalescent plasma at Houston Methodist that first reported the reduction in mortality among plasma recipients. There are two critical hints from that study, as well as others, that could guide how convalescent-plasma therapy could be used in coming months, as schools and businesses reopen and health officials brace for more cases. In Musser’s study, people receiving plasma with higher concentrations of antibodies against SARS-CoV-2 enjoyed greater and more rapid improvement in their health. “That’s the good stuff that we have been using now for almost a month in almost all of our patients,” he says. Scientists are working on ways to identify superdonors who produce the most potent antibodies with a relatively simple lab test. “It makes sense to preselect donors based on the presence of good antibodies that can prevent the virus from docking on cells,” says Rudolf Valenta, a professor of immunopathology at Medical University of Vienna, who has developed such an assay for research use in his country. Doctors are also keeping a close eye on the amount of antibodies that donors produce. After donating 17 times, Knight was told his antibody levels were still good, but that the hospital now had enough volunteers who had recovered more recently and were willing to provide their plasma.
Also important is when the plasma is transfused. Musser learned that people receiving the transfusions within three days of being hospitalized tended to do better than those who were transfused later in their illness.
That’s why the NIH is funding studies of convalescent plasma for people who have been recently diagnosed with COVID-19. In those trials, patients are randomly assigned to receive a transfusion of convalescent plasma or a placebo solution within three or four days of their diagnosis. Experts believe that intervening early to prevent the virus from infecting healthy cells will help people to avoid some of the more serious consequences of the disease as it progresses, including respiratory problems and injury to the lungs. Those late-stage effects are due to the body’s aggressive immune response to the infection, so avoiding activation of this revved up response by controlling the infection early might protect more patients from the more serious effects of the disease.
“We think this study is situated to give the greatest opportunity to see an effect,” says Dr. Clifton Callaway, professor of emergency medicine at the University of Pittsburgh, and one of the principal investigators for the 50-site trial. “We believe that in the first week of symptoms’ appearing, patients have probably not developed their own antibodies, so that’s the time when getting a transfusion of somebody else’s antibodies has the greatest potential benefit. We also think that early in the illness is the best opportunity to change the course of illness and prevent it from becoming severe. We’d like to catch it before it gets bad.”
Beyond Convalescent Plasma
Convalescent plasma, while useful, is still far from a panacea. For one thing, not all recovered patients make the same number of antibodies, or even the same types of antibodies, and those that pump out higher levels of antibodies are more sought-after as donors than those with lower levels. Some antibodies are also known to actually help viruses infect cells rather than block them, as a way to ensure viruses are destroyed by pathogen-devouring immune cells. One recent study showed that as many as 20% of patients who recovered from COVID-19 harbored these types of antibodies. While most experts believe that’s unlikely that these would negate the benefit of antibody-based therapies, they are watching for this effect in ongoing studies.
In addition, says Callaway, “Plasma is precious. It requires donors, it requires people to have the disease and to recover. More desirable would be to have something we can make in the lab and put into a vial.”
For decades now, scientists in the pharmaceutical industry have perfected developing and manufacturing monoclonal antibodies, which are antibodies specifically made to target a single part of an offending pathogen or even a tumor in cancer patients. Monoclonal antibodies have transformed cancer care, leading to remarkable improvements in survival rates in patients with breast, lung and skin cancers, among others, and have also proved to be formidable foes against infectious diseases such as rabies and Ebola. So once COVID-19 began its invasion of the human population last winter, researchers began investigating ways to target SARS-CoV-2 with monoclonal antibodies as well. “The hope is that we can nail down which type of monoclonal antibodies or cocktails of antibodies could do the same job as what we hope plasma will do,” says Callaway.
Plasma from recovered patients is the logical starting point for this search, and that’s where Carl Hansen and his team at AbCellera, a biotech company in Vancouver, began last spring. And they hit the antibody lottery.
AbCellera’s scientists specialize in developing monoclonal antibodies. In late February they received samples of plasma from the first recovered COVID-19 patients in North America, most of whom were from the West Coast. The team screened 6 million cells from one of these early patients and found about 500 unique antibodies against SARS-CoV-2. The researchers then mapped out where and how these antibodies attach to the virus, and isolated a single antibody that, in the lab, powerfully blocked SARS-CoV-2’s ability to bind to human cells.
That early luck may pay big dividends in a highly anticipated human trial. AbCellera partnered with pharmaceutical giant Eli Lilly to test its monoclonal antibody, dubbed Ly-CoV-555, in a multicenter study sponsored by the NIH that began recruiting around 200 participants in June and is expected to conclude in November.
Ly-CoV-555 is just one of a handful of specific antibodies that are currently being put to the test to treat COVID-19. And some scientists see potential for antibodies to prevent the disease as well. Because antibodies block the SARS-CoV-2 virus from infecting cells, it’s reasonable to test whether the right antibodies could be useful in preventing people from getting sick in the first place. The NIH agrees, and is sponsoring biotech company Regeneron’s study of a pair of antibodies to see if they can both prevent and treat disease; about 2,000 asymptomatic people who are part of households where a member tested positive will be randomly assigned to receive the two-antibody combination or a placebo. And the NIH is also sponsoring a study of Eli Lilly’s Ly-CoV-555 antibody as a preventive treatment in nursing homes. Once a resident or staff member in a nursing home tests positive, scientists will randomly assign the remaining residents and staff at the facility to receive either the antibody treatment or placebo to see if there is any difference in infection rates between the groups. “We and others have found that we can create a very potent antibody [in Ly-CoV-555] that completely blocks the virus’s ability to enter cells via the spike protein,” says Dr. Dan Skovronsky, chief scientific officer at Eil Lilly. In tests with monkeys, the antibody prevented the animals from getting massive infections. “That’s great news for the monkeys and possibly good news for humans,” he says. Researchers expect to have the first preliminary results from the study in September.
If it turns out that antibodies are an effective preventative, they could significantly reduce the number of new infections and help to stop the spread of COVID-19. And if the studies of antibody use early in people’s disease also proves successful, that could help to thwart transmission as well; if more people have their infections under control, then they are less likely to spread it to others. That’s an idea borrowed from the HIV field, in which doctors increasingly rely on “treatment as prevention” to bring viral load down to levels where it can’t spread as easily by contact.
Even if and when there is a vaccine to protect people against SARS-CoV-2 infection, antibody-based treatments may still be needed as part of a robust disease-fighting plan, says Callaway. “I believe there is a good chance that people will still pop up with illness, even with a vaccine,” he says. “Therapies like monoclonal antibodies or convalescent plasma are important for patients who develop illness despite a vaccination campaign and who are at risk of getting severe disease.”
For Towse, it doesn’t matter how antibodies actually do their job, just that, in his case, he believes they did. Grateful for his recovery, he is planning to donate his own plasma to potentially help others. “It’s a no brainer for me to give,” he says. “I could have been on a ventilator, and that just scares the hell out of me. We’ve got to get [the pandemic] under control and find some way to take care of this. And I think this plasma is the way to go.”
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com