I tried to kill my father for years. To be fair, I was following his wishes. He’d made it clear that when he no longer recognized me, when he could no longer talk, when the nurses started treating him like a toddler, he didn’t want to live any longer.
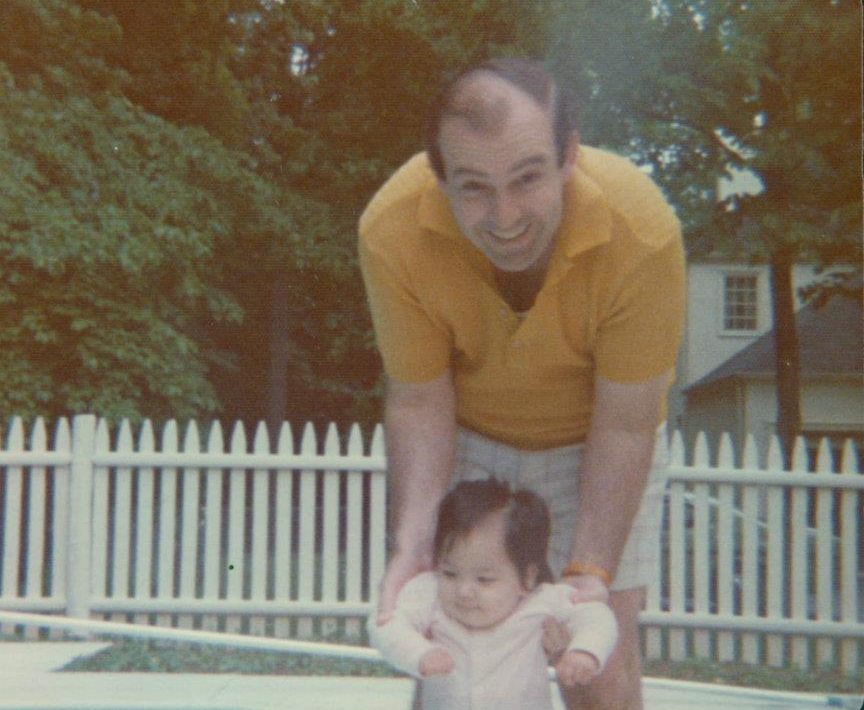
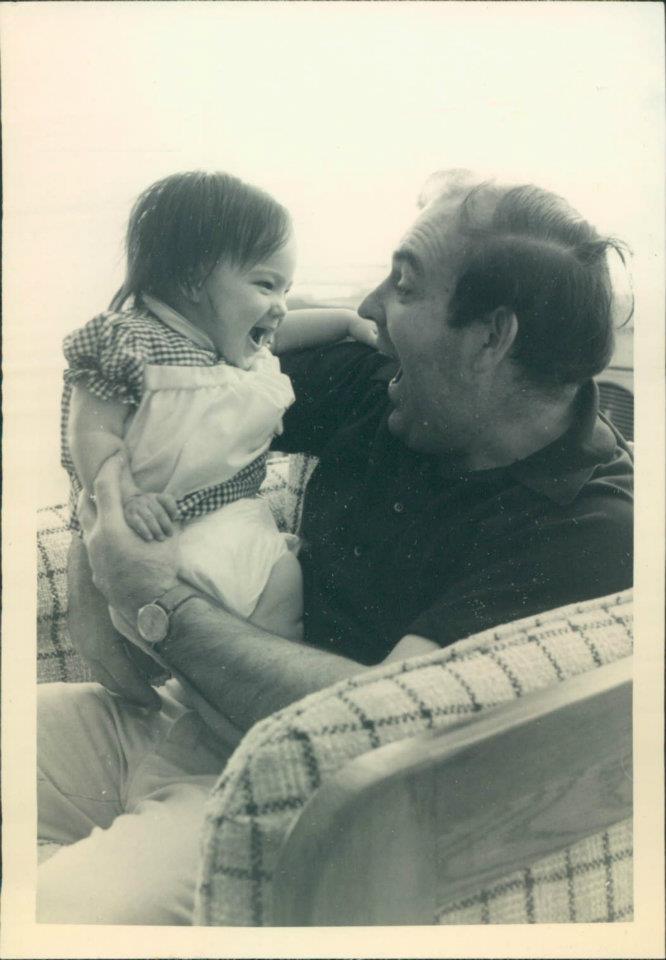
My father was 58 years old when he was diagnosed with Alzheimer’s disease. He took the diagnosis with the self-deprecating humor he’d spent a lifetime cultivating, constantly cracking jokes about how he would one day turn into a zombie, a walking corpse. We had a good 10 years with him after the diagnosis. Eventually, his jokes came true.
Seven years before he died, he forgot my name. Three years before his death, he forgot my mother’s existence. His speech devolved into word salad. “Honey, garbage bag synopsis toothbrush Bella potato beetle?” he asked. I replied as though I had understood: “Yes, Gray.” I had taken to calling him by his childhood nickname. He didn’t respond to “Dad”; he no longer realized he was a father.
He started peeing on the plastic plants in his facility, and in other inappropriate places. The nurses dressed him in diapers and a onesie. Sleep eluded him; when he slept at all, it would be on the nearest couch. He could no longer distinguish his room from others. With no pattern I could discern, he would hit me and hit his nurses. He would attack the walls.
In his final months, it took a team of nurses and aides to change him out of his onesie, shower him and put new diapers on him. He needed specialists for shaves, haircuts, dental care and toe and fingernail clipping. By his final days, his care cost $15,000 a month—none of which was covered by Medicare. I used up his pension, my mother’s death benefits, all of my parents’ savings and then my own.
I knew my father didn’t want to be this zombie, but assisted suicide was out of the question for us, for a number of reasons—not the least of which is that it’s illegal in the U.S. for dementia patients (the only country where it is legal for those living with dementia is Belgium). So, “killing” my father involved taking him off his heart, stroke and cancer medications and allowing him to eat whatever he liked, even if that meant 10 Klondike bars a day. Whatever made him happy—so little did at that point.
It seemed the only thing he remembered how to do was walk. He paced until the last week of his life. Shortly after he forgot how to get up, he forgot how to swallow. Inhaling food and spittle, he slowly choked to death—a fate unfortunately common for those living with Alzheimer’s.
A coming spike in Alzheimer’s
Stories like my father’s are about to become much more prevalent. We know of no cure for Alzheimer’s, and there is no treatment in sight (though after a review of initial findings, BioGen just resuscitated an Alzheimer’s drug trial that yielded better results than originally thought). And the number of people living with Alzheimer’s in the U.S. is about to skyrocket, thanks to general increases in life expectancy and the demographic peak of the Baby Boom.
By 2050, about 14 million Americans will have Alzheimer’s, according to Chicago’s Rush Institute for Healthy Aging. That’s compared with some 5.7 million now. Combine the total with other related forms of dementia, and the number rises to almost 30 million people, or about 8% of the country’s total estimated population in 2050.
By 2050, about 14 million Americans will have Alzheimer’s.
This epidemic is arriving in a society poorly equipped to cope with it. The U.S. health insurance system is failing those with chronic and degenerative diseases. The country’s economy is structured to make it difficult at best—and in many cases impossible—to give adequate care to adults who cannot get through the day on their own, without help.
There is no easy answer to this problem. We must devise fundamentally new ways to structure the care of Alzheimer’s patients. We must change how dementia is managed in a way that improves the quality of life of those who have the condition and also keeps it from derailing the lives of loved ones who care for them. And we have to think about how to pay for all of it. Many experts are now talking about the idea of “resilience,” giving patients tools outside of medical treatment to prevent dementia and improve the lives of those who are already living with the disease. Even neuroscientists—who are traditionally focused on biochemistry—are talking up the benefits. Neurologist Dr. Grazyna Pomorska and psychologist Judith K. Ockene argued in a 2017 article that it’s just as important to focus on the vitality, resilience and social connectivity of their patients as unraveling the science behind the disease.
A 2010 study of almost 1,000 residents of senior housing in the Chicago area found that giving the elderly a sense of purpose may reduce their risk of developing the disease. Researchers at Ohio State University in 2016 created a pilot program called “Resilient Aging” and found that when adults identified areas of adversity they’d overcome in their lives and discovered commonalities in one another’s struggles, it made them more resilient overall. And all of this may also benefit caregivers, who themselves are more likely to suffer from disease as a result of the stress of looking after loved ones. Some 40% of dementia caregivers die from the stress of caregiving before the death of those for whom they are caring, according to a 2002 Stanford study. And according to a 2017 survey of unpaid family caregivers by EMD Serono (a division of drug maker Merck), 45% skip their own medical appointments because their caregiving responsibilities don’t allow them time for themselves. This is certainly what happened to my mother. She died of a stress-induced brain aneurysm in 2011 after 10 years of caring for my dad. My father died in 2015.
One of the great misunderstandings about Alzheimer’s is that it is hereditary. My father’s family had no history of Alzheimer’s, for example, and only a tiny portion of dementias overall are thought to be caused by genetics; the vast majority are more likely caused by unknown environmental factors. Scientists are now considering everything from stress to high-sugar diets to chemical toxins as potential contributors.
Without knowing what’s causing the disease, researchers say the basics of good health apply. Exercise and a healthy diet have been shown to help with Alzheimer’s and related dementias. This has prompted a fitness and healthy-eating push for those entering middle age, when scientists now believe the disease first begins to manifest, with the aim of delaying, or maybe even preventing, the development of the disease. Increasingly, organizations like AARP, the Alzheimer’s Association and the World Health Organization, have focused on prevention.
But, of course, all of this comes too late for the majority of the Baby Boomers, the youngest of whom are already 55 years old. The Boomers—the 76.4 million people born between 1946 and 1964—represent a giant bulge in the system that will require significantly greater amounts of care than their parents or their kids.
Experiments in caregiving as a crisis looms
The U.S. is already short more than a million family caregivers. By 2030, the country will be short nearly 4 million family caregivers, and by 2040 an astonishing 11 million, according to the 2017 book Who Will Care for Us: Long-term Care and the Long-Term Workforce by Paul Osterman, an MIT professor of human resources and management. It’s likely at this rate that the cost of care will rise, and the quality of care will decline just as the nation needs it most.
In Japan, which has reached an elder demographic crisis ahead of the U.S., the government has begun developing robot caregivers. On a functional level this has helped with critical staffing shortages: robots can take blood pressure, wake people up and prompt them to take pills or remember to put on their shoes. They can even warn you when they see signs of physical imbalance. They can be fashioned into furry cats and dogs for company and play your favorite music and movies. But they can’t fully take the place of human interaction, nor are they advanced enough yet to do anything complex like changing an adult diaper or help with bathing, feeding and dressing.
In Europe, which has some of the oldest populations in the world, some governments are trying to tap into the old model of multiple generations living together under one roof. For example, the German government offers discounted housing to young students and to families in senior communities. Such interventions aim to rebuild traditional support systems, in which grandparents help babysit or cook for the kids when the breadwinning generation has to work late, and then the younger generations help when the grandparents grow too old to fully care for themselves. But this model, while successful with seniors without degenerative brain diseases, breaks down when it comes to giving care to those with worsening dementia. What can children do when their grandparents wander off, or grow paranoid and potentially violent?
Outside Weesp, a suburb of Amsterdam, the Dutch government has created a so-called “dementia village.” The residents of Hogewey have no idea that they are watched around the clock. The shop vendors and restaurant waiters are actually care staff, and residents are locked inside the village boundaries. When one comes to an exit, they’re gently redirected to another activity. Similar villages have been created in England, Canada, Australia, New Zealand and the U.S.—where there’s a 1950s-themed adult day-care chain called George G. Glenner—but they aren’t without controversy, with critics saying it’s demeaning to fool those living with the disease with fake realities.
Focusing more on the caregivers
From an Alzheimer’s diagnosis to death usually takes five to seven years. My father’s decline was more protracted; he died 14 years after he was diagnosed. For the first 10 years, he was relatively stable. My mother gave him cues—tell a joke at a certain point, flirt with a waitress at another—but it became increasingly difficult to hide. And her death provoked a steep decline. He was never the same.
My experience matches that of so many caregivers, who face increasingly untenable demands. There are innumerable duties early on, from providing transportation and managing legal affairs to helping loved ones bathe, dress and use the toilet. And then the needs spiral. At first someone with Alzheimer’s may just forgot the occasional appointment or name. Next, they lose their driver’s license and easily get lost in unfamiliar places. Travel became difficult. They stop understanding money, and so become easy prey for scammers. Then they need help doing things like cutting their toenails, dressing and speaking. At the end, they need help with everything from walking to eating.
Yet little money is earmarked for finding caregiving solutions. The vast majority of the nearly $2 billion a year spent on Alzheimer’s disease by the U.S. government and private organizations goes to medical research, which has so far proved fruitless at providing a cure. Meanwhile, Medicare, the principal system of health insurance for the elderly, doesn’t directly cover Alzheimer’s and dementia, and neither does most private health insurance. Long-term care insurance can help, but only 2% of Americans have it.
Medicaid, a public health insurance system for the poor, will pay for a bed in a nursing facility. But it’s also not much of a solution. Only 10% of Americans currently over 65 qualify. And the facilities covered by Medicaid focus on traditional nursing, designed to cure diseases. Faced with the incurable, they can panic. Wandering Alzheimer’s residents often end up in psychiatric wards.
Dementia isn’t something that can be treated and ameliorated. It requires specialized care. Engagement is key to maintaining quality of life for as long as possible. But nursing homes have few activities, and those living with dementia often can’t keep up with the non-cognitively challenged. The sense of being left behind compounds isolation and depression, leading to quicker declines.
Meanwhile, costs for paid care are growing much faster than inflation. The average stay at an assisted living facility is 28 months at a cost of $3,500 a month. For those who need full-time care, that’s close to $100,000—almost all out of pocket for Alzheimer’s and dementia.
Currently, Alzheimer’s and related dementia costs Americans $259 billion annually. This estimate includes the amount families pay for home or assisted-living care; spending on accommodations for the disease like senior-proofing homes or buying Velcro shoes and pants when laces and buttons become too complex to master; as well as lost wages by caregivers who quit work to care for loved ones. By 2050, that number will more than quadruple to $1.1 trillion, according to Alzheimer’s Association estimates.
Alzheimer’s and related dementia costs Americans $259 billion annually. By 2050, that number will more than quadruple to $1.1 trillion
There’s little help available from the government. The 2010 Affordable Care Act had a long-term care provision in it—the Community Living Assistance Services and Supports Act that created a voluntary and public long-term care insurance option for employees—but the Obama administration deemed the program unsustainably expensive, and it was repealed by Congress in 2013. Though Hawaii and Washington recently passed some versions of long-term care funds to help their citizens pay for senior care, the other 48 states have no plans in place.
The Zombie Apocalypse
Of all the 2020 candidates, only two have comprehensive long-term care plans: Vermont Senator Bernie Sanders and Massachusetts Senator Elizabeth Warren, though they cost $30 trillion and $20.5 trillion respectively. If those numbers are eye-popping, the Urban Institute, an economic policy think tank, estimates that if nothing is done, the government will end up paying $50 trillion as millions of middle-class families spend down their loved one’s assets and dump them into Medicaid.
Currently, Medicare won’t pay for the long-term care of Alzheimer’s and dementia. But it will cover most diseases a patient gets as a result of dementia. So, if you suffer heart failure, have pneumonia or break a hip due to losing your balance—all common side effects—Medicare will pay for your initial treatment and up to 120 days of long-term care per diagnosis. If Medicare covered dementia directly, rather than only the secondary symptoms, overall care would be much better, and likely also cheaper. People with dementia would be less isolated, less depressed, and have a better quality of life.

In many ways, I was lucky. My dad needed little extra nursing until the last two years. He could put on his Velcro shoes. He could still walk. For years, he couldn’t tell you who was U.S. president, what decade it was, my name, or his own. But he could feed himself and go to the bathroom unaided. He was, as he called it, a zombie.
In his final days, he had skin lesions, and constant urinary tract and ear infections. I only treated the things that made him uncomfortable. By the end, a lot of things made him uncomfortable. He also developed lymphoma and heart failure—conditions that Medicare would finally have covered but which I chose not to treat.
After all, I was trying to kill him, not prolong his suffering, which was by this point all too clear to me. One day I saw a woman on his hall throwing up in a trash bin. I asked the staff if she had food poisoning. “No,” they told me, her nausea was just a side effect of her chemotherapy. To me, giving cancer treatments to someone with advanced Alzheimer’s seemed like cruel and unusual torture. She had no idea why she was so sick. And the chemo was prolonging her poor quality of life.
For my father, I stuck with the bare minimum. Even that was a huge stress on my finances. I was considering a home-equity loan before his death absolved that need.
But even Medicaid may not be a solution for much longer. As the costs of care skyrocket and states struggle to meet Medicaid budgets, Alzheimer’s and dementia patients like my dad may be released—like other “psychiatric” patients—on to the streets if their families can’t support them. And unless they get arrested and put into jail, they may be doomed to homelessness in their senescence. This spectacle, I imagine, is what my father would have wryly dubbed the “zombie apocalypse”: the living dead wandering America’s streets as their brains are slowly eaten. If nothing is done to overhaul the system, I fear that my father’s fate will be shared by millions, without the care and protection I was able to provide.
A version of this story appeared first in New America Resilience.
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com



