Pocket-size ultrasound devices that cost 50 times less than the machines in hospitals (and connect to your phone). Virtual reality that speeds healing in rehab. Artificial intelligence that’s better than medical experts at spotting lung tumors. These are just some of the innovations now transforming medicine at a remarkable pace.
No one can predict the future, but it can at least be glimpsed in the dozen inventions and concepts below. Like the people behind them, they stand at the vanguard of health care. Neither exhaustive nor exclusive, the list is, rather, representative of the recasting of public health and medical science likely to come in the 2020s.
David Abney: Drone-delivered medical supplies
Since March, UPS has been conducting a trial program called Flight Forward, using autonomous drone deliveries of critical medical samples including blood or tissue between two branches of a hospital in Raleigh, N.C., located 150 yards apart. A fleet-footed runner could cover the distance almost as fast as the drones, but as a proof-of-concept program, it succeeded, and in October the FAA granted the company approval to expand to 20 hospitals around the U.S. over the next two years. “We expect UPS Flight Forward to one day be a very significant part of our company,” says UPS CEO David Abney of the service, which will deliver urine, blood and tissue samples, and medical essentials like drugs and transfusable blood. UPS is not alone in pioneering air deliveries. Wing, a division of Google’s parent company Alphabet, received similar, but more limited, FAA approval to make deliveries for both Walgreens and FedEx. And in Ghana and Rwanda, drones operated by Silicon Valley startup Zipline are already delivering medical supplies to rural villages. —Jeffrey Kluger
Christine Lemke: The biggest Big Data
There are 7.5 billion humans, and tens of millions of us track our health with wearables like smart watches, as well as with more traditional devices like blood-pressure monitors. If there were a way to aggregate all that data from even a few million of us and make it all anonymous but searchable, medical researchers would have a powerful tool for drug development, lifestyle studies and more. California-based Big Data firm Evidation has developed just such a tool, with information from 3 million volunteers providing trillions of data points. Evidation partners with drug manufacturers like Sanofi and Eli Lilly to parse that data; that work has led to dozens of peer-reviewed studies already, on subjects ranging from sleep and diet to cognitive-health patterns. For founder Christine Lemke, one of Evidation’s ongoing projects, to see if new technologies can effectively measure chronic pain, is personal: Lemke has a rare genetic disease that causes frequent back pain. Evidation is partnering with Brigham and Women’s Hospital on the project.—Jeffrey Kluger
Doug Melton: A stem-cell cure for diabetes
Type 1 diabetes affects 1.25 million Americans, but two in particular got Harvard biologist Doug Melton’s attention: his daughter Emma and son Sam. Treatment can involve a lifetime of careful eating, insulin injections and multiple daily blood-glucose tests. Melton has a different approach: using stem cells to create replacement beta cells that produce insulin. He started the work over 10 years ago, when stem-cell research was raising hopes and controversy. In 2014 he co-founded Semma Therapeutics—the name is derived from Sam and Emma—to develop the technology, and this summer it was acquired by Vertex Pharmaceuticals for $950 million. The company has created a small, implantable device that holds millions of replacement beta cells, letting glucose and insulin through but keeping immune cells out. “If it works in people as well as it does in animals, it’s possible that people will not be diabetic,” Melton says. “They will eat and drink and play like those of us who are not.”—Don Steinberg
Abasi Ene-Obong: A more diverse global bio bank
A major limitation threatens to hamper the era of personalized medicine: people of Caucasian descent are a minority in the global population yet make up nearly 80% of the subjects in human-genome research, creating blind spots in drug research. Dr. Abasi Ene-Obong, 34, founded 54gene to change that. Named for Africa’s 54 countries, the Nigeria-based startup is sourcing genetic material from volunteers across the continent, to make drug research and development more equitable. 54gene is conscious of the ugly history of colonial exploitation in Africa. If companies are going to profit by developing marketable drugs based on the DNA of African people, Africa should benefit: so, when partnering with companies, 54gene prioritizes those that commit to including African countries in marketing plans for any resulting drugs. “If we are part of the pathway for drug creation, then maybe we can also become part of the pathway to get these drugs into Africa,” Ene-Obong says.—Corinne Purtill

Sean Parker: A disruptive approach to cancer research
One of the original disrupters of the new economy is bringing his approach to medical research. The Parker Institute for Cancer Immunotherapy, established by Napster co-founder and former Facebook president Sean Parker, is a network of top institutions including Memorial Sloan Kettering, Stanford, the MD Anderson Cancer Center and more. Its goal is to identify and remove obstacles to innovation in traditional research. For example, all of the participating institutes have agreed to accept an approval decision by any of their respective Institutional Review Boards, which “allows us to get major clinical trials off the ground in weeks rather than years,” says Parker, and at lower costs. Perhaps most important, Parker wants to infuse the project with his market sensibility: “We follow the discoveries coming from our researchers and then put our money behind commercializing them,” he says, either by licensing a product or spinning it out into a company. Since its founding in 2016, the institute has brought 11 projects to clinical trials and supported some 2,000 research papers.
Thomas Reardon: A wristband that can read your mind
A man wearing what looks like a chunky black wristwatch stares at a tiny digital dinosaur leaping over obstacles on a computer screen before him. The man’s hands are motionless, but he’s controlling the dinosaur—with his brain. The device on his wrist is the CTRL-kit, which detects the electrical impulses that travel from the motor neurons down the arm muscles and to the hand almost as soon as a person thinks about a particular movement. “I want machines to do what we want them to do, and I want us to not be enslaved by the machines,” says Thomas Reardon, CEO and co-founder of CTRL-Labs, the device maker. The hunched-over posture and fumbling keystrokes of the smartphone era represent “a step backward for humanity,” says Reardon, a neuroscientist who, in a past life, led the development of Microsoft’s Internet Explorer. The technology could open up new forms of rehabilitation and access for patients recovering from a stroke or amputation, as well as those with Parkinson’s disease, multiple sclerosis and other neurodegenerative conditions, Reardon says.—Corinne Purtill
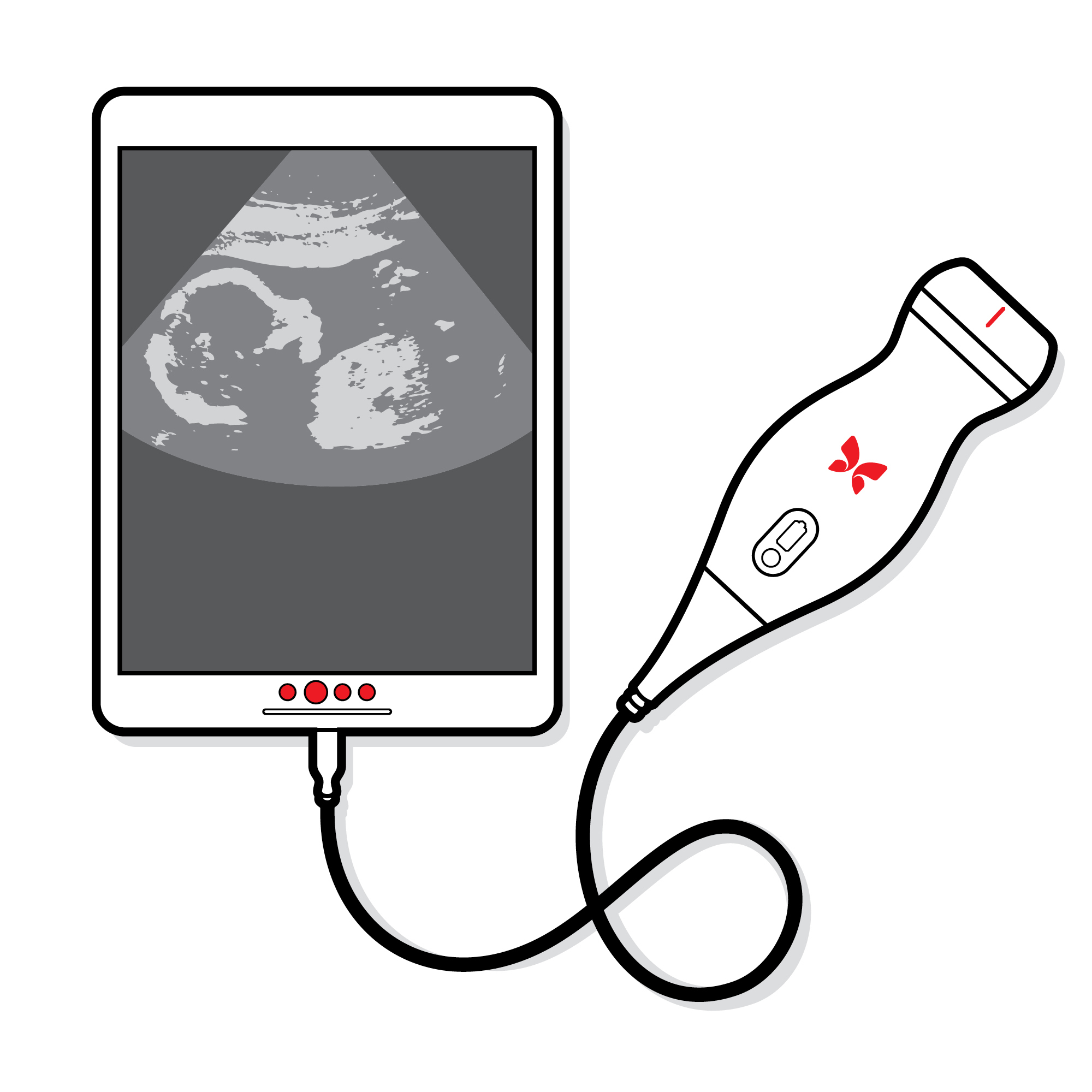
Jonathan Rothberg: An ultrasound in your pocket
There are more than 4 billion people globally who don’t have access to medical imaging—and could benefit from Butterfly iQ, a handheld ultrasound device. Jonathan Rothberg, a Yale genetics researcher and serial entrepreneur, figured out how to put ultrasound technology on a chip, so instead of a $100,000 machine in a hospital, it’s a $2,000 go-anywhere gadget that connects to an iPhone app. It went on sale last year to medical professionals. “Our goal is to sell to 150 countries that can pay for it. And [the Gates Foundation] is distributing it in 53 countries that can’t,” Rothberg says. The device isn’t as good as the big machines are and won’t replace them in prosperous parts of the world. But it could make scanning more routine. “There was a time when the thermometer was only used in a medical setting, when a blood-pressure cuff was only used in a medical center,” Rothberg says. “Democratizing [health] happens on multiple dimensions.”—Don Steinberg
Shravya Shetty: Cancer-diagnosing artificial intelligence
Symptoms of lung cancer usually don’t appear until its later stages, when it’s difficult to treat. Early screening of high-risk populations with CT scans can reduce the risk of dying, but it comes with risks of its own. The U.S. National Institutes of Health found that 2.5% of patients who received CT scans later endured needlessly invasive treatments—-sometimes with fatal results—after radiologists erroneously diagnosed false positives. Shravya Shetty believes artificial intelligence may be the solution. Shetty is the research lead of a Google Health team that in the past two years built an AI system that outperforms human radiologists in diagnosing lung cancer. After being trained on more than 45,000 patient CT scans, Google’s algorithm detected 5% more cancer cases and had 11% fewer false positives than a control group of six human radiologists. The early results are promising, but “there’s a pretty big gap between where things are and where they could be,” says Shetty. “It’s that potential impact that keeps me going.”—Corinne Purtill
Joanna Shields: AI to read every science paper
Every year, more than 2 million peer-reviewed research papers are published—far too many for any individual scientist to digest. Machines, however, don’t share this human limitation. BenevolentAI has created algorithms that scour research papers, clinical trial results and other sources of biomedical information in search of previously overlooked relationships between genes, drugs and disease. BenevolentAI CEO Joanna Shields was an executive at companies such as Google and Facebook, and then the U.K.’s Minister for Internet Safety and Security, before joining BenevolentAI. A frequent critic of the tech industry’s lapses in protecting young people from exploitation and abuse online, Shields sees BenevolentAI as an opportunity to harness technology’s power for good. “All of us have family members, friends who are diagnosed with diseases that have no treatment,” she says. “Unless we apply the scaling and the principles of the technology revolution to drug discovery and development, we’re not going to see a change in that outcome anytime soon.” —Corinne Purtill

Sean Slovenski: Walmart-ification of health care
Whenever the world’s biggest retailer aims its gigantic footprint at a new market, the ground shakes. In September, Walmart opened its first Health Center, a medical mall where customers can get primary care, vision tests, dental exams and root canals; lab work, X-rays and EKGs; counseling; even fitness and diet classes. The prices are affordable without insurance ($30 for an annual physical; $45 for a counseling session), and the potential is huge. In any given week, the equivalent of half of America passes through a Walmart. “When I first started here … [I] thought, That can’t be true,” says Sean Slovenski, a former Humana exec who joined Walmart last year to lead its health care push. If the concept spreads, repercussions await in every direction. Like Walmart’s merchandise suppliers, doctors and other medical pros may need to adjust to the retailer’s everyday low prices. Still, cautions Moody’s analyst Charles O’Shea: “Health care is multiple times harder than selling food.”—Don Steinberg
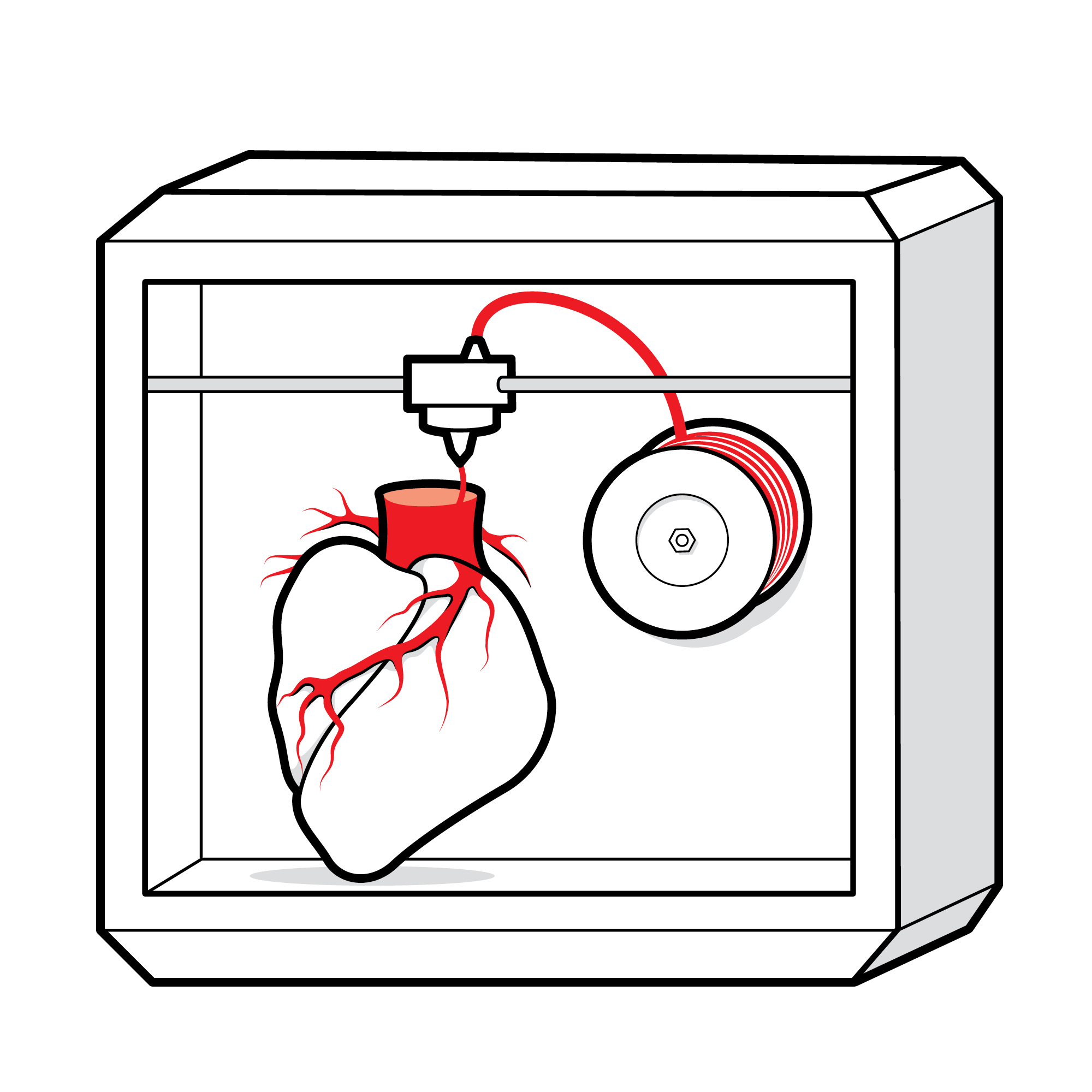
Charles Taylor: 3-D digital hearts
For too many people with suspected heart problems, invasive catheterization is necessary to diagnose blocked or narrowed arteries. Doctors must then choose the best method for improving blood flow from a handful of options, including balloon angioplasty and stenting. Charles Taylor, a former Stanford professor, started HeartFlow to help patients avoid invasive diagnostic procedures and improve treatment outcomes. The company’s system creates personalized 3-D models that can be rotated and zoomed into, so doctors can simulate various approaches on screens. In some cases, it can help avoid invasive procedures entirely. “By adding the HeartFlow … to our available resources for diagnosing stable coronary disease, we are able to provide patients with better care as we evaluate risk,” said Duke University cardiologist Manesh Patel, at the American College of Cardiology’s annual meeting in March. —Jeffrey Kluger
Isabel Van de Keere: Rehab in virtual reality
Isabel Van de Keere was at work one day in 2010 when a steel light fixture pulled loose from the ceiling and fell on her. The accident left Van de Keere, a Belgian-born Ph.D. in biomedical engineering, with a cervical spine injury and severe vertigo that required three years of intense neurological rehabilitation. She practiced the same tedious exercises dozens of times in a row, with progress so slow it seemed undetectable. Now 38, she’s the founder and CEO of Immersive Rehab, a London-based startup whose goal is to change the neurological-rehab experience using virtual reality. By expanding the range and type of exercises patients can try, VR creates more opportunities to harness the brain’s plasticity and repair neural pathways; increases the amount of data caregivers can use to measure progress and adapt programs; and improves the monotonous, frustrating experience of rehab. Feedback from volunteer patients and therapists has been promising; the company is now preparing to run clinical trials in the U.S. and Europe.—Corinne Purtill
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com