In a partnership with Apple, health insurance company Aetna announced Tuesday a new app and wellness program that will track and offer personalized health recommendations to its customers, and grant them the option to redeem points for gift cards or toward payments for an Apple Watch by meeting activity goals and other health-related challenges. In short, you can expect a free Apple Watch as long as you’re taking care of yourself.
To participate in Aetna’s program, which kicks off later this spring, users will need either an iPhone 5S or newer, or an Apple Watch Series 1 or newer. The announced Attain app — which resembles Apple’s in-house apps — will provide personalized activity goals based on your age, sex, and weight, and challenge you to engage in activities like getting more sleep. It turns your activity and challenges into points, which can be redeemed for items like gift cards should you not want to put them toward the payment of your Apple Watch.
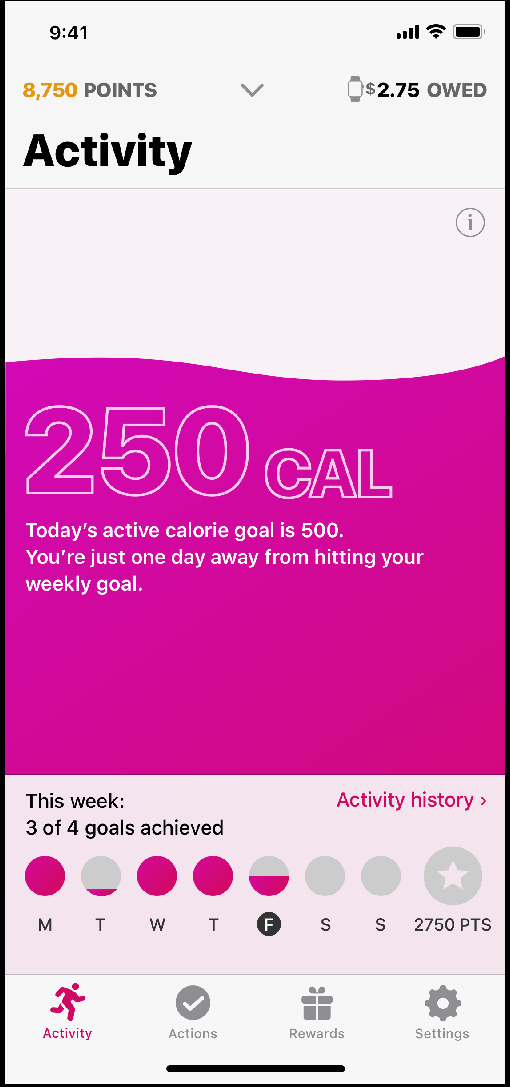
The app will also make recommendations based on both your health records and the activity measured by your Apple Watch. “As we learn over time, the goal is to make more customized recommendations that will help members accomplish their goals and live healthier lives,” Apple COO Jeff Williams said in a statement. You’ll receive alerts when it’s time to schedule a visit with your physician, or for prescription refill reminders and flu shots.
Aetna isn’t the first insurance company to offer wearable devices to its customers, just the first to partner with Apple in such a prominent fashion. Aetna and Apple teamed up in 2016 with a similar program, noting that “90 percent of participants” reported at least one health benefit while using their Apple Watch. Aetna also cited a study from RAND Corporation claiming an average activity increase of 34 percent when a “loss-framed incentive” like being forced to pay out of pocket for your ostensibly free Apple Watch was introduced.
Companies like UnitedHealthcare offer wellness programs that use devices like a Fitbit to track steps and reward users with a discounted device. Recently, John Hancock Insurance announced its own wellness incentive program, complete with Apple Watch payment program, though customers will have to cough up $25 up front. Both Aetna’s and John Hancock’s wellness incentive programs are based on a rewards program developed by wellness and insurance company Vitality Group.
Health insurance providers certainly have an incentive to improve their customers’ overall health, as that could reduce the number of claims they have to pay out over long term. And a free Apple Watch will no doubt appeal to many people looking to try out the wearable or improve their health, though skeptical customers might be scared off by the prospect of providing even more health data to insurance companies. In 2018, the West Virginia’s Public Employment Insurance Agency voted to scrap a wellness incentive program with Humana Go365 that would increase customer deductibles and insurance rates if certain health and activity goals were not met. But Aetna says the information gathered by Attain “will not be used for underwriting, premium or coverage decisions,” and will be used only to improve the app’s custom recommendations. Furthermore, Aetna says the data gathered will be encrypted and fully HIPAA compliant, stored securely by both Aetna and Apple.
More Must-Reads from TIME
- Caitlin Clark Is TIME's 2024 Athlete of the Year
- Where Trump 2.0 Will Differ From 1.0
- Is Intermittent Fasting Good or Bad for You?
- The 100 Must-Read Books of 2024
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- FX’s Say Nothing Is the Must-Watch Political Thriller of 2024
- Merle Bombardieri Is Helping People Make the Baby Decision
Write to Patrick Lucas Austin at patrick.austin@time.com