There is an excellent model that demonstrates how the U.S. should reform the current reactive model of public health emergency management—it is the solution found to address disasters established by the Stafford Disaster Relief and Emergency Assistance Act. Under the Stafford Act, enacted in 1974 and later updated in 1988, authorizes the President of the United States, when disaster strikes, to deploy the coordinated efforts and resources of the federal government to save lives and property, and restore communities hit hard by a calamity. The federal government provides warnings of hurricanes and floods, and in cases of wildfires dispatches resources to extinguish flames before they threaten people and property.
The knowledge of public health experts, the Centers for Disease Control and Prevention, policy makers, health-care professionals and patient advocacy organizations should be brought together with the relevant committees in the House and Senate to develop measurable criteria to create baselines for defining, responding and mitigating public health threats to effectively and immediately without the delay engendered by the need for Congress to pass an emergency supplemental appropriations.
Read more: Here’s Why Zika Funding Is Stalled in Congress
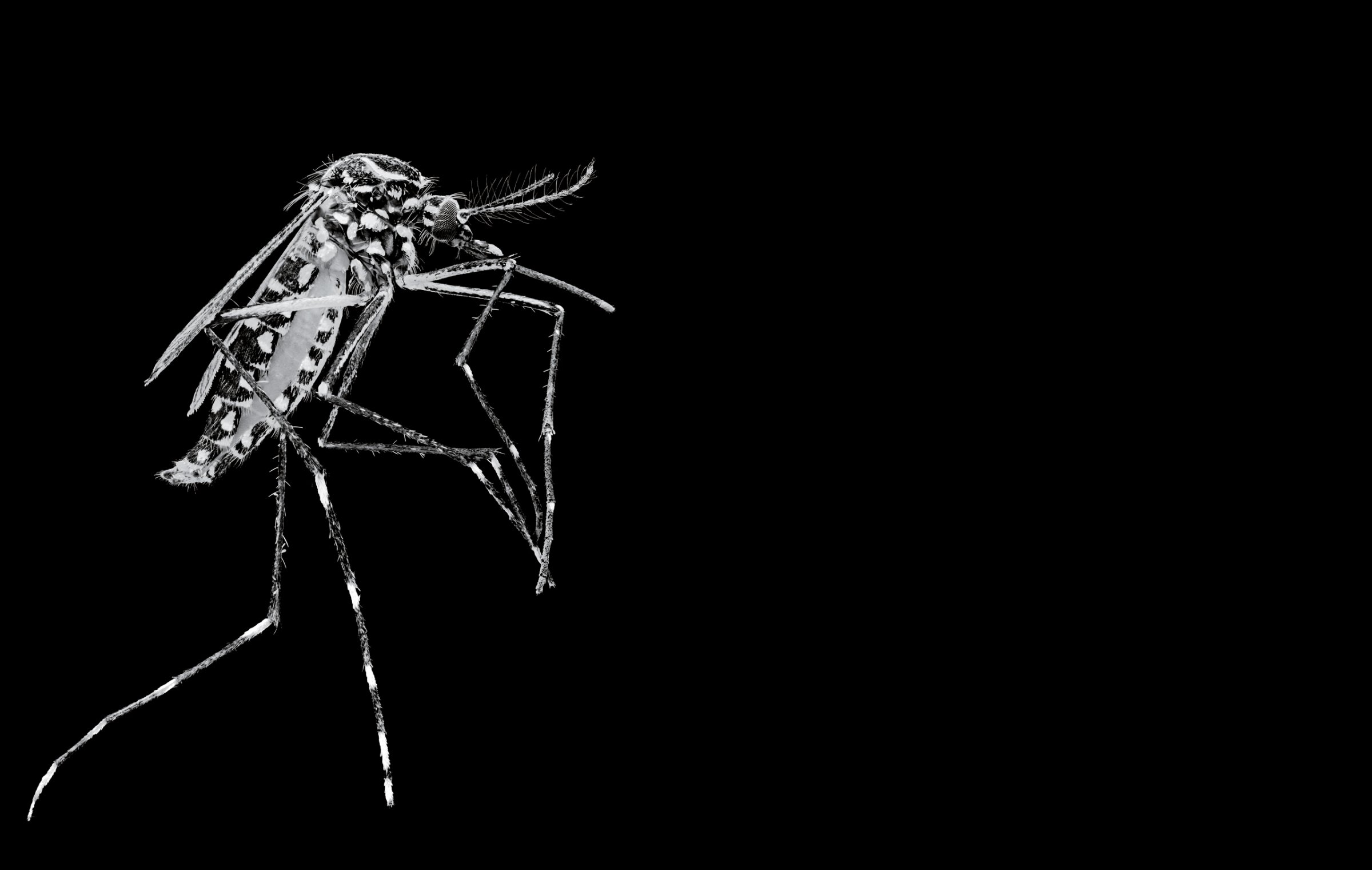
The U.S. must be capable of responding quickly to emerging threats that are identified anywhere in the world. The Ebola and Zika viruses for examples existed in other nations for many years before they became a clear and present threat to public health in the Western Hemisphere and the U.S. The cost of waiting until a public health threat is present in the U.S. increases the threat to our nation’s public health systems; it reduces the likelihood of success in winning the battle against a pathogen and it risks a new contagious disease becoming endemic—akin to the common cold. In addition, the cost of putting down a public health threat increases as time passes.
There is a long history of threats to public health posed by pathogens. In March 1918, in Kansas, the U.S. had its first case of the Spanish Flu, which is recorded as the first H1N1 flu epidemic. This pandemic killed 50 million persons worldwide it ended abruptly in 1919. The mortality rate of the Spanish Flu was as high as 1 death for every 5 infections and 50% of the deaths, or about 25 million, occurred in the first 25 weeks of the outbreak. We are now in the 31st week of the Zika Virus global health emergency, which was declared by the World Health Organization on Feb. 1, 2016.
The world is still battling the HIV/AID global pandemic, which became known to public health experts well before the disease made it into the United States. Still, it took President Clinton’s efforts to put the full force of the federal government behind finding an effective treatment for HIV that slowed the progression of the disease from becoming full blown AIDs. By 2011, more than 60 million people globally had been infected by AIDS and 25 million had died.
The legislative process has proven itself not to respond in a timely manner to public health threats. The U.S. to be more robust enough needs to have in place mechanisms designed to respond systemically to federally declared public health emergencies and deliver assistance to support state and local governments in carrying out their responsibility to protect the public health. This is the second time in three years that a global health emergency has been declared that required Congress to act by passing a new law to fund the national response. This is the second time that the legislative process failed to act quickly when the public health threat was known and its consequences were clearly understood by domestic infectious disease experts.
On Aug. 24, 2014, the Democratic Republic of the Congo Ministry of Health notified the World Health Organization of an outbreak of Ebola virus. On Oct. 8, 2014, Ebola claimed the life of Thomas Eric Duncan after he presented symptoms at the time of admission to an emergency room. He had recently traveled to a country where the disease was actively being transmitted; he had a fever over 100 degrees accompanied by abdominal pain, dizziness, nausea and headache. Communications had gone to public health officials, hospitals, and health-care providers from the Centers for Disease Control stating that all patients should be asked whether they had traveled to West Africa recently; and checked for symptoms of Ebola, which include a dangerously high fever, abdominal pain, nausea and headache. Unfortunately, Mr. Duncan having all of the symptoms to be considered a possible Ebola patient was not admitted for observation, tests, and treatment, but instead sent home.
As of April 13, 2016, globally there were 28,652 suspected Ebola cases; 15,261 laboratory confirmed Ebola cases and 11,325 deaths from Ebola. Today, the CDC continue to monitor for Ebola disease outbreaks. We can no longer act as if a disease outbreak in a nation on the other side of the world has no relevance or importance to the public health status of communities within the U.S. In fact, we know that this is not the case. H1N1, Ebola, and Zika viruses are hard lessons to the global health community teaching that the world has changed and that it is time the U.S. adjusts by becoming proactive and cease being reactive in preparing for and defending against public health threats and emergencies.
Establishing a model that is quantitative and based upon measurable changes in public health conditions around the world as well as within the U.S. and having the capacity to react quickly can save lives and assures public health system stability. Our nation has some local health-care systems that are second to none, such as the Houston Medical Center, but our national public health system has glaring weaknesses when handling pathogens that may be as dangerous as Ebola and as contagious as the Spanish Flu. There are only four hospitals in the U.S., and a total of 15-16 beds, for persons infected with a human viral hemorrhagic fever: Emory University Hospital in Atlanta has two Ebola beds; St. Patrick Hospital in Missoula, Montana, has one or two; National Institutes of Health in Bethesda, Maryland, has the capacity to treat two patients in its Special Clinical Studies Unit, according to the National Institute of Allergy and Infectious Diseases at the NIH; and Nebraska Medical Center in Omaha, reportedly has a biocontainment facility with 10 beds total.
The public health challenge for our nation is to effectively address the sudden emergence of a highly contagious pathogen with a mortality rate of 1 in 5 so that the public health threat may be identified within hours of patient zero, a team of public health experts deployed with the requisite equipment and resources within 24 hours to any point on the globe, establish field labs, hospitals, coordinate with local public health officials, communicate with public health and disease experts globally; type and identify the threat; its method of transmission; and determine what is needed to contain the threat; while beginning work on treatments and potential cures. Their work would also be to calculate mortality rates and the point when the disease may become endemic over a 25 week time period to stop its spread, which should include communicating to local, state and tribal public health officials’ the information they will need to prepare to face the threat that may be just a flight away.
A Public Health Relief and Emergency Assistance Law is overdue—I urge the leadership of the House and the Senate to work in a bipartisan fashion to put on the desk of the President of the United States a law that will be the cure for the weaknesses in our nation’s public health system when it is faced with public health emergencies.
More Must-Reads from TIME
- How Donald Trump Won
- The Best Inventions of 2024
- Why Sleep Is the Key to Living Longer
- Robert Zemeckis Just Wants to Move You
- How to Break 8 Toxic Communication Habits
- Nicola Coughlan Bet on Herself—And Won
- Why Vinegar Is So Good for You
- Meet TIME's Newest Class of Next Generation Leaders
Contact us at letters@time.com