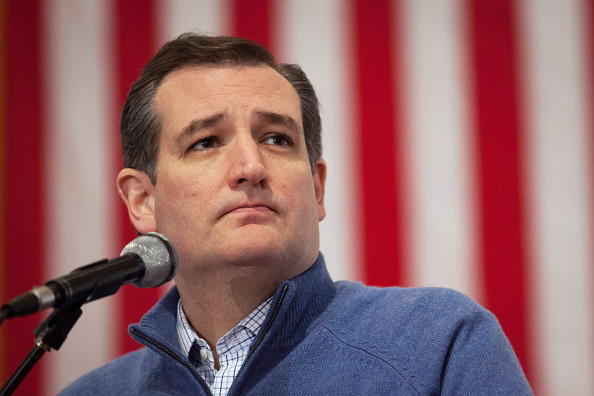
Ted Cruz won Iowa’s Republican presidential caucus promising to repeal every word of Obamacare. When pressed for details, he said he would separate insurance from employment, expand the use of health savings accounts, and allow people to purchase insurance across state lines. These are good ideas, ones we’ve heard before. There are, however, a number of other policy initiatives worthy of attention, whether the Affordable Care Act is repealed or not. There’s one simple thing Congress could do that would expand access to high-quality care, especially for patients in rural areas, without costing taxpayers a dime.
Telemedicine providers, which uses telecommunication to provide health care over distances, have made great strides in improving access to care for rural communities. Telemedicine allows quick access to specialists, as with stroke victims where time is of the essence. Video interactions are expected to replace a sizable chunk of face-to-face office visits.
But the current system of state licensing stands in the way of interstate practice. Physicians must maintain licenses in each state in which they treat patients. Congressional action to define the location of telemedicine services as the location of the physician would allow physicians to practice with a single license in multiple states. It would allow telemedicine to achieve its full potential.
Under the current system, physicians with multiple licenses are challenged to adhere to state-specific medical practice regulations, as inconsequential to patient safety as they may be. Legal scholars make the case that Congressional action to reduce barriers to interstate telemedicine would find support in the U.S. Constitutions’ Commerce Clause.
The American Medical Association and the Federation of State Medical Boards argue that allowing a physician licensed in one state to offer remote care in others would strain state board resources, putting the public at risk. The irony is that, for decades, state medical boards have been criticized by consumer groups and others for putting the public at risk.
It is not state boards, but actions by private actors that protect consumers. Physician oversight and the resulting consumer protection are the product of actions by entities liable for physician malpractice, including hospitals, provider groups, health-insurance companies setting up physician panels or networks, and medical malpractice insurers. These entities credential and evaluate physicians regularly, not just as they enter the profession or when a complaint is filed.
There is no evidence that telemedicine providers go beyond the range of services that safely can be provided remotely. Studies of telemedicine reveal improved access, high quality and, in some cases, cost savings. Telemedicine providers face incentives related to liability that are similar to those faced by other providers. As brand name becomes increasingly important in the interstate telemedicine market, I would expect telemedicine quality to rise above that of many local service providers. Telemedicine offers convenience, quality, cost savings and remote access.
Congressional action to redefine the location of the practice of medicine as that of the physician would be consistent with a 2011 Center for Medicare and Medicaid Services’ decision related to hospital credentialing. That decision allows hospitals on the receiving end of telemedicine to rely on the credentialing and privileging efforts of the hospital at which a telemedicine doctor is physically located.
Lack of license portability after nearly two decades of state board inaction led to proposals for redefining the location of the practice of medicine, as advocated here, and federal licensing of telemedicine providers. Fearful of the impact of these policy initiatives on the status quo, the Federation of State Medical Boards took steps to design model state legislation for what has come to be known as the Interstate Medical Licensure Compact. In 2015, 12 states joined the newly formed Compact.
A casual observer might miss the fact that the Compact offers no portability. Under the Compact physicians continue to be responsible for state specific license and renewal fees and held to multiple state-specific medical practice regulations. The Compact offers an “expedited” application process for multiple licenses, not a single license that would allow physicians to practice in more than one state.
Private licensing service companies already exist to help physicians secure licenses and private credential verification services facilitate the periodic credentialing of physicians. It is not clear whether the Compact Commission could expedite the process of securing multiple licenses or lower the cost.
The bottom line is that the potential of telemedicine is limited as long as state licensing obstructs interstate practice. Politicians on both sides of the aisle could take a giant step toward facilitating interstate telemedicine by supporting Congressional action to define the location of the practice of medicine as that of the physician.
More Must-Reads from TIME
- Introducing the 2024 TIME100 Next
- The Reinvention of J.D. Vance
- How to Survive Election Season Without Losing Your Mind
- Welcome to the Golden Age of Scams
- Did the Pandemic Break Our Brains?
- The Many Lives of Jack Antonoff
- 33 True Crime Documentaries That Shaped the Genre
- Why Gut Health Issues Are More Common in Women
Contact us at letters@time.com