“Health consists of having the same diseases as one’s neighbors,” the English writer Quentin Crisp once quipped. He was right: when a disparity occurs, the sense of threat to our health inevitably increases. And what is true of the individual seems to be true of societies as a whole. “Parasite stress,” as scientists term it, has long been a factor in human relations, intensifying the fear and loathing of other peoples, as well as marginal groups within our own societies.
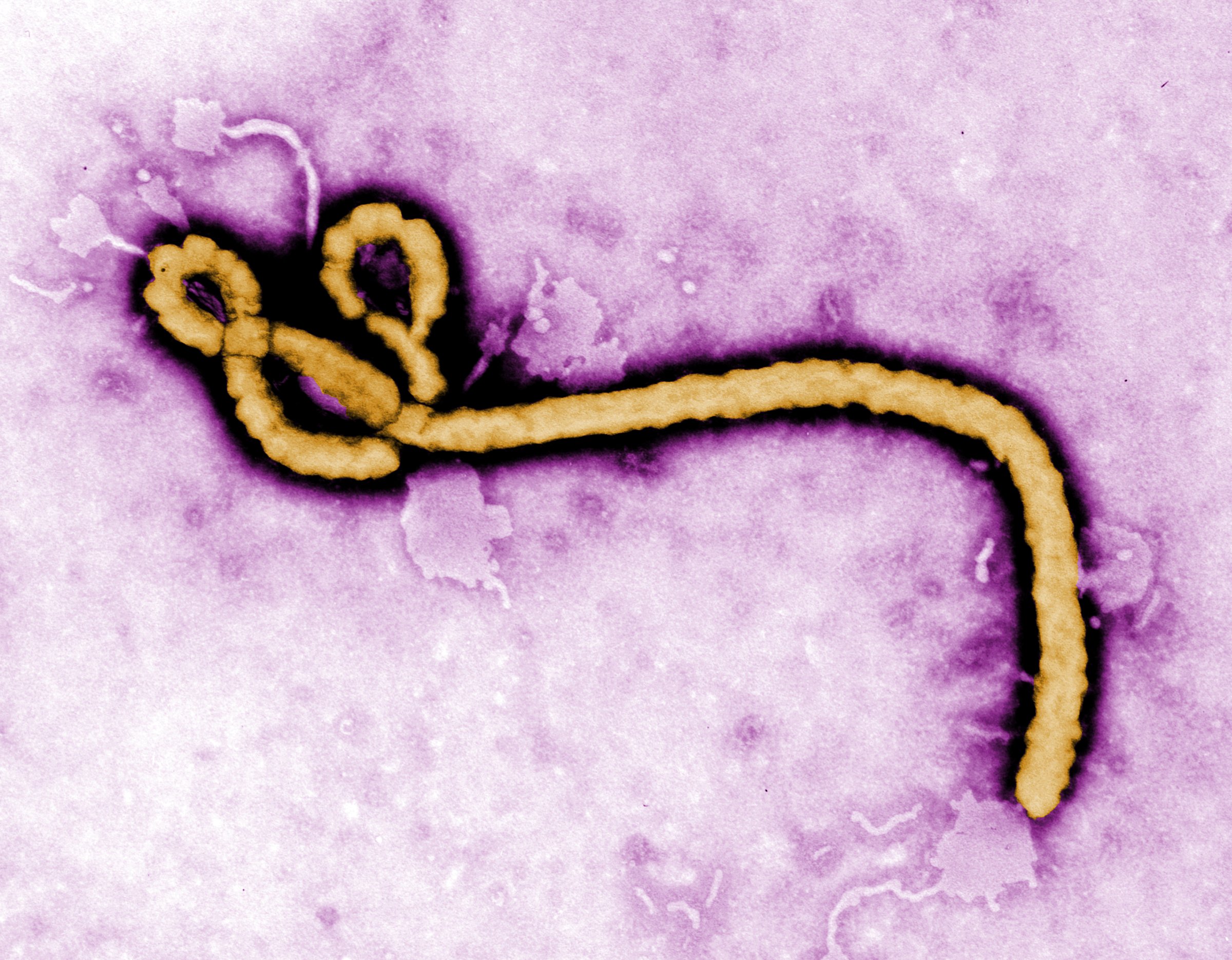
For a while, it seemed that we had transcended all that. In the wake of AIDS, a real effort was made to raise awareness of the link between health and civil rights. A more cosmopolitan sensibility emerged, encapsulated in the noble ideal of global health. Money poured into Africa in an effort to reduce the crippling burden of malaria and HIV. But, as Ebola reminds us, fundamental problems remain. No longer confined to remote rural locations, Ebola has become an urban disease and has spread uncontrollably in some western African nations, in the absence of effective healthcare.
The sheer scale of the present outbreak has brought these problems forcibly to our attention, but it has also revived the Victorian image of Africa as a dark continent teeming with disease. Pity and horror mingle with irrational fear, and have led some governments to introduce illiberal measures that have little or no basis in science. And the dread of Ebola is no longer confined to the West. Indeed, it tends to be more apparent throughout Asia than among Americans and Europeans. In August, Korean Air terminated its only direct flight to Africa due to Ebola concerns, never mind that the destination was nowhere near the affected region of the continent, but thousands of miles to the east in Nairobi! North Korea has also recently suspended visits from all foreign visitors – regardless of origin.
Anxiety about Ebola is more acute in Asia because epidemics, poverty, and famine are well within living memory. Hence, the eagerness to disengage from countries afflicted with infectious disease. But this divisive tendency stems largely from ignorance. As shown in the case of HIV/AIDS, we can find ways of dealing with new infections that are both effective and humane. To do so requires leadership and determination, both of which have been lacking.
The slowness of the international community to respond to the problem of Ebola, and the willingness of some to sever ties with the continent, is a legacy of centuries of conditioning in which health, politics, and prejudice intertwine. The roots of this mentality lie deep in our history. After humans mastered the rudiments of agriculture 12,000 years ago, they began to domesticate a greater variety of animals and came into contact with a wider range of infections. But this happened at different times in different places, and the resulting imbalance gave rise to the notion that some places were more dangerous than others. Persons who moved between settlements were regarded with suspicion in a world in which the vast majority were sedentary.
Well into the 20th century, diseases tended to be associated with other peoples and places. Thus, when the disease we call syphilis was first encountered in Europe in the late 1490s, it was labelled the Neapolitan or French disease, depending on where one happened to live. And, when the same disease arrived in India, with Portuguese sailors, it was called firangi roga, or the disease of the Franks (a term synonymous with “European”). The influenza that spread around the world from 1889 to 90 was dubbed the “Russian Flu” (for no good reason) and the same was true of the “Spanish Flu” of 1918 to 19. It is safe to assume they were not called these names in Russia or Spain.
We are still inclined to think of epidemic disease as coming from somewhere else, brought to our doorstep by outsiders. Moreover, notions of infection first developed within a religious framework – pestilence came to be associated with vengeful deities who sought to punish transgressors or unbelievers. In the European plagues of 1347 to 51 (the “Black Death”), Jews were made scapegoats and killed in substantial numbers. It was said that their presence was an abomination to the Christian god. In later centuries, gypsies, merchants, and practitioners of “unwholesome” trades were added to the ranks of scapegoats.
Remnants of such beliefs endure, as we have seen in claims that Ebola has been sent to rid the world of gays, atheists, and others of whom God apparently disapproves. But the Black Death began a process whereby disease was gradually, albeit partially, secularized. With nearly half the population dead from plague, manpower was precious and many rulers attempted to preserve it, as well as to reduce the disorder which usually accompanied an epidemic. Disease became the trigger for new forms of intervention and social separation. Within states, it was the poor who came to be stigmatized as carriers of infection, on account of their supposedly unhygienic and ungodly habits. They were the object of measures to contain the spread of infection and also to some extent of charitable provision. But the threat of disease, at least in the first instance, appeared to come from without. States used diplomatic intelligence to assess the risks posed by communication with other cities or states. Sometimes an embargo was imposed on all movement from infected places or ships and their crews were placed in isolation, usually for 40 days. This practice was known as “quarantine.” Originating in Italian and Adriatic cities in the 1470s, it gradually spread throughout Europe and large facilities known as “lazarettos” were constructed to house people and merchandise from places suspected of infection.
These precautions flowed from recognition of the fact that disease followed trading routes and that plague emanated from countries in Asia, where it appeared to be endemic. But they were reinforced by a heavy blanket of prejudice, sometimes against the poor, sometimes against “the Turk,” a term which embraced the inhabitants of the Ottoman Empire and the Islamic peoples of Central Asia. The Ottoman lands were the gateway through which plague spread from the east and its rulers were seen as corrupt and fatalistic.
In Europe, too, plague became intimately associated with misgovernment. Countries began to use the accusation of disease to blacken the reputation of rival nations and damage their trade. Quarantines and embargoes became a form of war by other means and were manipulated cynically, often pandering to popular prejudice. The threat of disease was frequently used to stigmatise immigrants and contain marginalized peoples, especially as populations became more mobile during the nineteenth century. The actual numbers of immigrants turned away at inspection stations such as Ellis Island was relatively small but the emphasis placed on screening certain minorities helped shape public perceptions. During an epidemic of cholera in 1892, President Benjamin Harrison notoriously referred to immigrants as a “direct menace to public health,” singling out Russian Jews as a special danger. Chinese migrants were similarly branded when they arrived in California.
The 1800s were an unusually volatile period. Industrialization and urbanization strained social relations and brought enormous sanitary problems. Seemingly new diseases – like cholera – emerged out of nowhere. Ancient ones – like plague, which had been confined for many years to isolated pockets in Asia – returned with a vengeance. The appearance of both these diseases was regarded by some as a form of divine judgment. Others blamed ignorance, squalor, and superstition in their places of origin (India for cholera and China for plague). These prejudices were based partly only older ideas about the dangers of the orient but also reflected a new disdain for non-Western cultures, borne of the age of empire. These “Asiatic” diseases followed the contours of the new global economy, eased by modern technologies such as steamships and railways. They were the consequence not of oriental corruption but of the transformative powers of commerce, science and industry.
The response of Western nations to this maelstrom of disease was to erect barriers to infection. They tried to create a kind of sanitary “buffer zone” in the Middle East and imposed strict quarantines against ports in Africa and Latin American which were regularly infected with yellow fever. But as the global economy matured constraints such as quarantine and embargoes became cumbersome. The panicky response to the re-emergence of plague in the 1890s, in cities such as Hong Kong, Bombay, Sydney and San Francisco, created enormous disruption. Trade came to a standstill and many businesses were destroyed. Great Britain and the U.S. proposed a different way of dealing with disease based less on stoppages and more on surveillance and selective intervention. Combined with sanitary reform in the world’s greatest ports, these measures were able to arrest epidemic diseases without disrupting commerce. The international sanitary agreements of the early 1900s marked a rare example of cooperation in a world otherwise fractured by imperial and national rivalries.
In a globalized world, it is simply not feasible to isolate places which appear to present a higher risk of infection. To do so would devastate their economies and detrimentally affect ours. The spill over of refugees and political instability from imploding states likewise has ramifications far beyond the afflicted countries themselves. We should also remember that an effective response to plague and cholera depends not only on the containment of these diseases, but also on environmental and social improvements. The West was able rid itself of epidemic disease in precisely this way. The European powers also began to clean up their colonies, while the U.S. and the Rockefeller Foundation took similar measures in Latin America and the Philippines. Few would advocate a return to “sanitary imperialism,” but the risk of disease is heightened by a laissez-faire attitude to the welfare of other countries.
The present effort to contain Ebola will probably succeed now that more personnel and resources have been sent to the afflicted countries. But our long-term security depends on the development of a more robust global health infrastructure capable of pre-emptive strikes against emerging infections. If there is one positive thing to note about the reaction to Ebola it is that governments have responded, albeit belatedly, to growing public demand. A more inclusive, global identity appears to be emerging, with a substantially recalibrated understanding of our cross-border responsibilities in the realm of health. Whether this awareness and improvised crisis management translates into a long-lasting shift in how we tackle fast-spreading contagions remains an open question – a life-and-death one.
Mark Harrison is Professor of the History of Medicine and Director of the Wellcome Unit for the History of Medicine, Oxford University. He is author of Contagion: How Commerce has Spread Disease (Yale University Press, 2013). He wrote this for Zocalo Public Square.
More Must-Reads from TIME
- Donald Trump Is TIME's 2024 Person of the Year
- Why We Chose Trump as Person of the Year
- Is Intermittent Fasting Good or Bad for You?
- The 100 Must-Read Books of 2024
- The 20 Best Christmas TV Episodes
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- Merle Bombardieri Is Helping People Make the Baby Decision
Contact us at letters@time.com