Philosophers and Poets, from their perch on the cutting edge of reason, have always seen the advantage of anxiety. It is the “dizziness of reason,” argued Soren Kierkegaard; “the handmaiden of creativity,” said T.S. Eliot; “the beginning of conscience,” observed novelist Angela Carter. So have actors backstage, summoning eternal energies and edges for the roles they play, and sprinters on the block, finding hormonal springs in the fear of failure that allow them to achieve race times they never managed in practice.
But to the rest of us, when the race is to make it to dinnertime without losing our tempers, losing our jobs, losing our minds over the stresses we juggle, anxiety feels like no friend. Our days are filled with all kinds of personal reasons to get our adrenaline pumping and our minds churning, even before we start thinking about holiday gridlock, double-dip recessions, wars, terrorist threats and weather patterns.
“The presence of unpredictability, uncertainty and uncontrollability all provoke anxiety pretty automatically,” says Sally Winston, co-director of the Anxiety & Stress Disorders Institute of Maryland (ASDI). “It’s a signal of either an internal or an external threat.”
Anxiety disorders–which include generalized anxiety, obsessive-compulsive disorder (OCD), phobias, panic disorder, social anxiety and posttraumatic stress disorder (PTSD)–are the most common mental illnesses in the U.S., affecting about 18%–40 million–of adult Americans. And adults aren’t the only sufferers. Phobias and other clinical conditions can strike in childhood, and students applying to college, preparing for finals or entering a brutally tough job market have as many reasons to be anxious as their parents and grandparents do.
Excess stress hormones wear on the body, nipping away at the DNA that keeps cells dividing and long-lived, constricting the blood vessels and causing blood pressure to rise. Even the immune system is affected, as white blood cells that normally patrol for bacteria and viruses aren’t produced at normal, disease-fighting levels. It’s for these reasons that anxiety and stress have been linked to heart attacks, strokes, immune disorders, obesity, infertility and more.
There are effective psychotherapies for anxiety and plenty of meds that can help take the edge off. But if a share of Americans equivalent to the entire population of Argentina is still suffering, there’s clearly a gap in our medical knowledge. The good news is, science is filling that gap. New scanning technology is revealing how anxiety plays out in the brain–the neurological byways that distinguish one kind of anxious reaction from another and the possible ways each can be stopped. Blood studies are exploring how the chemistry of anxiety drives the nature and severity of the condition. Gene mapping is telling the complex story of where anxiety sits on the genome, providing clues to who may be at greatest risk, which in turn could mean early intervention that could prevent misery later in life.
That’s not to say all anxiety should be battled. Sometimes it should be embraced–even celebrated. In just the right amounts, the hormones that drive anxiety can be powerful stimulants, arousing the senses to function at their sharpest. Psychologists are familiar with a curve–which appears in most of their textbooks–that elegantly captures the relationship between stress and performance. It’s a bell-shaped line that steadily climbs as the tension and worry that accompany a performance rise in lockstep with the quality of that performance. The peak of that arc–where the systems are clicking, the senses are alert and we recall with perfect clarity everything we’ve learned–is precisely where seasoned performers learn to hop off.
The key isn’t not to feel anxious; it’s to learn ways to manage that experience. “Anxiety itself is neither helpful nor hurtful,” says ASDI’s Winston. “It’s your response to your anxiety that is helpful or hurtful.”
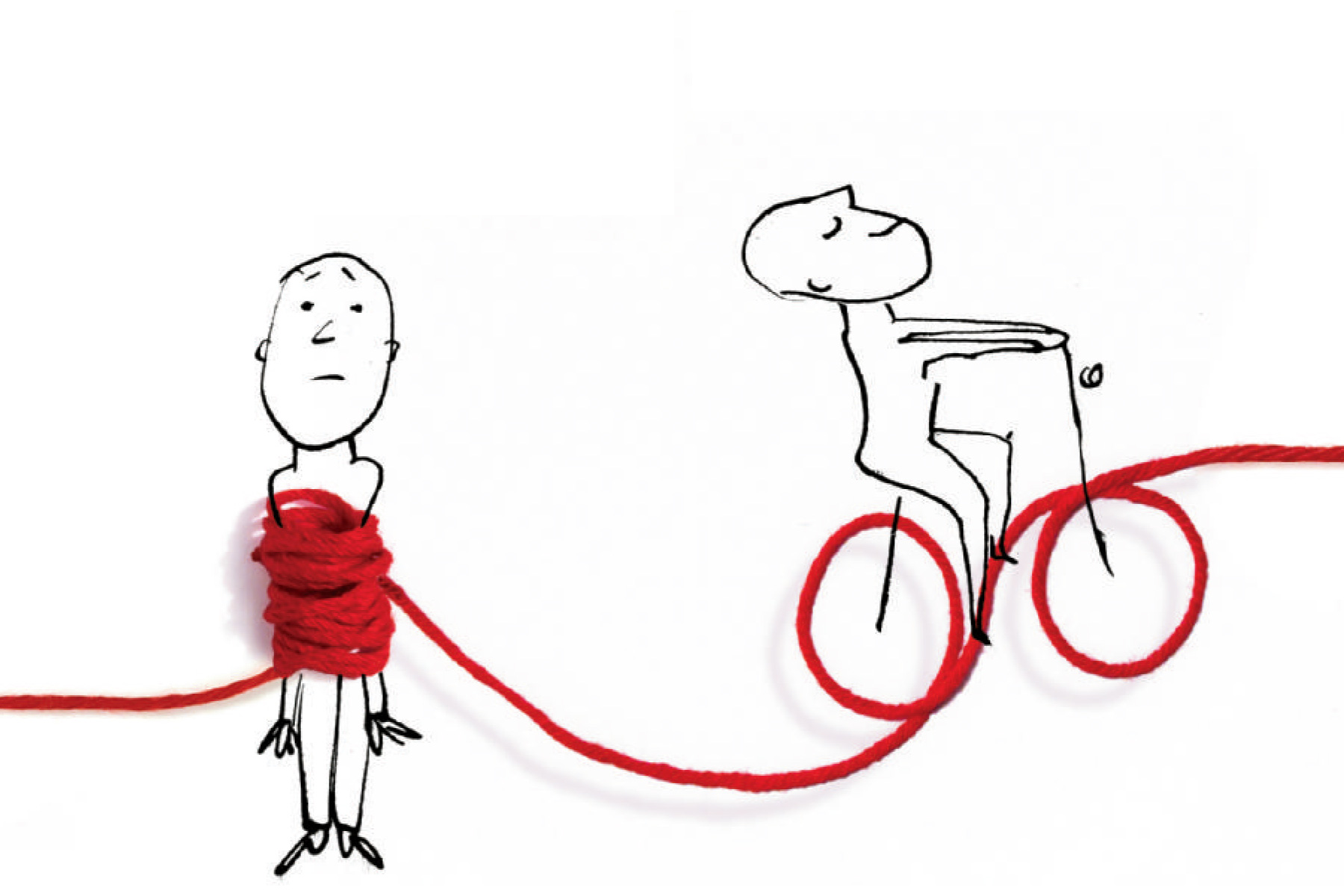
Psychologists refer to this very straightforward idea as the difference between a challenge stress, which can light our competitive fire, and a threat stress, which can douse it fast. Most of the time, it feels as if our brain makes that choice by itself, without ever consulting us. What we want to learn–need to learn to stay calm and well–is how we can take charge.
The Balancing Act
For all the suffering anxiety causes, the fact is, the species would not be better off without it–and we might not be here at all. At its core, anxiety is a reaction, an arousal to a stimulus that we perceive as dangerous or threatening. The fabled saber-toothed tiger springs at the primitive human, and the human reacts with a biological red alert, bypassing the relatively time-consuming thinking centers in the brain in favor of a shortcut directly to the deeper-seated hypothalamus. This awakens the nervous system to release hormones that instantly rev up heart rate and respiration, feeding fresh blood and oxygen to the muscles, which need the boost to carry the human as quickly and as far away from the danger as possible.
Even the mere possibility that the tiger may be out there gets the system going, as the senses become more acute, picking up on every smell, every sound, every change in the air. It’s a nifty response, one that produced a lot of people who would live to see another day and, more important, sire new generations of babies who would inherit their hair-trigger reflexes.
In fact, it’s this dual face of anxiety that has made it such a permanent part of the evolutionary recipe for the human species. Richard Lewis, the famously neurotic comedian, delivers his stand-up without a fixed script–the comedic equivalent of driving with your eyes closed–yet surfs the performance curve deftly, insisting that he needs his anxiety to make it through his time onstage.
“Before I go on, I’m a nervous wreck,” he says. “But ultimately I feel more comfortable being uncomfortable. I feel I’m a better artist without a set list, so I never had one and never will.” The actress Sarah Bernhardt once told a young protge who claimed not to have stage fright, “Don’t worry. It comes with talent.”
Non-performance-related anxiety can have a certain buzz at first too. “The adrenaline rush I get is extremely powerful,” says Nathan (not his real name), 55, an artist who suffers from paralyzing panic attacks that strike in the night. “It’s this feeling where I’m wide awake and I can see things behind me, in front of me and all around me, and it’s a really cool feeling. But if it stays at that high level and I can’t calm myself down, I feel like I might explode.”
The metabolic jujitsu that Lewis has learned–turning anxiety back on itself–is a skill that we all possess but are not all adept at using. Professional performers, by contrast, learn to call on this trick almost at will. Watching how they work is what revealed to psychologists the dichotomy of challenge and threat stresses, and they’ve worked since to define the precise characteristics of the two states. “Challenge stress [occurs when] you feel like you can cope with the situation, that despite its high demands, you have the resources to handle it,” says Elissa Epel, a psychologist at the University of California, San Francisco. “With threat stress, you feel less capable of handling the situation, and that can lead to a more unhealthy response.”
The problem with all this is that our ancient systems have not quite kept up with the modern world and aren’t terribly good at distinguishing between a jungle full of killer cats and a conference room full of nothing but other people. If we can’t make the distinction, mortal terror can quickly consume us in decidedly nonmortal circumstances. And while our moments in the spotlight may not come all that often–certainly less often than for professional performers–there are also the constant, subtler worries and pressures that grind at us every day, sometimes leaving us staring at the ceiling deep into the night. Collectively this creates a kind of chronic anxiety condition, with a nonstop series of stressors leaving us struggling with one crisis even as we’re worrying about the ones to come. That can lead to overload and paralysis.
“Worry is supposed to be Step 1 of problem solving, but it can be problem-generating instead,” says Reid Wilson of the University of North Carolina at Chapel Hill, director of the Anxiety Disorders Treatment Center. “If it gets going too long, it actually overrides your ability to problem-solve.”
Teasing apart how these stresses work is not easy, and multiple mechanisms start to emerge when researchers focus on the biological processes that drive our varied experiences. Michael Davis at Emory University was the first to map how fear and anxiety–including stage fright–play out in the brain in very different ways. When we’re startled, the klaxon in the hypothalamus sounds, signaling the pituitary gland to release a hormone that in turn instructs the adrenal gland to pump out the 30 other hormones that get the body’s respiratory, cardiac and other systems crackling. Principal among these chemicals is cortisol, commonly called the stress hormone because it’s found in such high concentrations in the blood of very anxious or stressed people. It’s cortisol that does most of the cellular damage when it hangs around in the body too long.
Also involved in the fear reaction is the amygdala, the emotional hub of our brain, which regulates not just fear but also anger, pleasure, desire and more. In a series of experiments that investigated how mice who were fearful reacted to being startled, Davis showed that while anxiety may be related to fear, it is a more prolonged and diffuse response that involves a broader network of brain circuits.
That makes sense, since anxiety is not just a fear of imminent danger but also a broader prospective reaction to possible dangers. This plays a critical role in certain types of clinical anxiety such as phobias, panic attacks and PTSD that are often consequences of having lived through or learned about a threatening experience–and coming to dread its recurrence. Awful as that is to go through, it’s also highly adaptive. The fight-or-flight response wouldn’t be useful, after all, if we didn’t learn from each near death event by making a powerful mental record of whatever signals alerted us to the impending threat–the shadow of the approaching tiger or the footsteps that once signaled a mugger and could again. People with panic disorders thus fret over what could trigger their next attack, always on the lookout for any potential catalyst that could set them off; obsessive-compulsive patients tend to focus on one possible negative outcome–being robbed, say–and compulsively work to prevent that from happening, perhaps by repeatedly checking the lock on their door.
Davis’ understanding of all this led to a more sophisticated map of anxiety, which many experts now believe involves constant activation of a part of the fear response known as the hypothalamus-pituitary-adrenal (HPA) axis and failure to turn it off when a threat has passed. Keeping that signal alive may be the responsibility of the brain region known as the bed nucleus of the stria terminalis (BNST), which regulates the autonomic part of our nervous system, including heart and breathing rates, and is more active in the brains of anxiety-disorder patients. The BNST is fueled by adrenaline, which means the HPA axis, unlike the fear response, may not always involve cortisol.
Dr. James Abelson, director of the Stress & Anxiety Disorders Program at the University of Michigan, helped confirm this thinking with a study involving people who were anxious about driving and dreaded the next time they had to get behind the wheel. Measuring the cortisol in the subjects’ saliva an hour before they arrived at the lab and again while they were on a test drive, he and his colleague found that the cortisol was the same despite the subjects’ reporting feeling more anxious and worried while they were driving.
Learning from Fear
To patients suffering from either full-blown fear or more-pedestrian anxiety, the perfectly reasonable response to this is, So what? Why does the biological basis matter, since both conditions feel lousy no matter what? The fact is, it matters a lot. The fight-or-flight response, with its surging cortisol and respiratory and cardiovascular hysteria, leaves little room for learning, because it often bypasses the higher regions of the brain. Anxiety, by contrast, engages one more critical region of the brain–the prefrontal cortex, where we collect our thoughts by planning, organizing and reasoning.
Says Abelson: “The neural system that defines what we call anticipatory anxiety–the ability to predict possible negative consequences and prepare for them by worrying–shares circuitry with but also has separate pathways from the circuitry that drives fear itself.” Engaging the anxiety pathway but hitting the brakes before reaching the panic cliff is what allows performers to be nervous before going on and then do just fine once they’re onstage–and store that lesson for all the subsequent times they’ll face an audience. This holds for other, higher-stakes professions too.
“I call it more a sense of excitement, a sense of arousal, than anxiety,” says Dr. Craig Smith, chairman of the department of surgery at Columbia University Medical Center and New York–Presbyterian, who performed former President Bill Clinton’s quadruple-bypass heart operation in 2004–a riskier activity than anything a comedian or actor faces. Smith copes with having a person’s life on the line every time he goes to work by learning to toggle from the initial, uncontrollable limbic reaction that arouses his senses and raises his blood pressure to his cool and deliberative prefrontal cortex, which, for instance, tells him the President’s case is no different from the thousands of bypass operations he has performed already. “I don’t let my brain go far into the supernegative scenarios where I completely fold,” he says.
Who’s at Risk?
Smith no doubt developed his steady surgical hand in large part through simple practice, but plenty of people would never be confident enough to even contemplate taking on such a job in the first place; just as many people would sooner die than stand up in front of an audience. So what distinguishes the steely-nerved from the jumpier types? Experiences, of course, account for a lot. A person with a traumatic childhood is likelier to grow up anxious than is one whose upbringing was relatively free of psychological or physical challenges. And being in one car accident is likely to make you more nervous on the highway than someone who’s never been in even a fender bender. But that’s not everything. Combat troops may all experience the horrors of war, but only about 15% go on to develop PTSD.
Genes are partly to blame as well, and this, like the fight-or-flight response, starts out as a very good thing. Newborn babies separated from their mothers immediately start crying and refuse to eat or sleep through the night, settling down only when they’re back in Mom’s arms–which the people who have been putting up with the crying are happy to accommodate. The instinct to react this way is played out along the HPA axis and encoded in the genes that help regulate that network. But researchers have identified about 150 aberrations in DNA that are associated with increased anxiety of the less adaptive kind. A child with one parent who has OCD, for example, faces a risk of developing the disorder that’s five times as great as one whose parents aren’t affected.
The genetic piece of the puzzle may be even more complex than just the genes your parents were born with and pass on to you. Mom’s and Dad’s experiences with stress and anxiety and how they react to them can leave a genetic legacy in the form of how intensely certain genes are turned on or off. Studies of male mice that had offspring both before and after being stressed (by being socially isolated from their peers) showed that the litters born to the males after the traumatic experience displayed more anxious behaviors than those born before. What’s more, when nervous pups born to a nervous dad experienced some kind of trauma of their own, they reacted to it more negatively than normal baby mice would.
Such partly genetic, partly experiential dynamics may be at play in the human species too–and might explain the 85% of combat troops who are spared from PTSD. “The condition of the brain at the time of a stressful experience probably plays a critical role in whether somebody develops an anxiety disorder like PTSD or not,” says Abelson.
Fixing What Ails You
One happy fact for anxiety sufferers is that the very same system that drives anxiety in our stimuli-saturated world may also be our salvation. Because the anxiety circuits are built to bridge the emotional and cognitive parts of the brain, it’s possible to train ourselves out of a certain amount of anxiety with what therapists call habituation. Babies who cry or become tense when they hear a car horn or a thunderclap eventually learn that nothing dangerous follows the sound and thus learn to acknowledge but not react to it. Cognitive behavioral therapy (CBT) helps patients learn the same lesson.
People with a phobia of, say, spiders will often react with fear and anxiety to a picture of one or simply the thought of one–never mind an encounter with the genuine crawly article. Learning to control the anxiety involves gradual exposure to spiders, from least scary circumstances to most, with the brain–and thus the body–growing sequentially desensitized with each encounter. Similarly, patients with OCD practice what is called exposure and response prevention. If your obsession is germs, your treatment might consist of touching a doorknob or the sole of your shoe and then resisting familiar undoing behaviors like washing your hands. It’s not about feeling anxious but about finding ways to react effectively.
“What is important is your appraisal of the situation and your assessment of your coping strategies,” says Diego Pizzagalli of Harvard Medical School, director of the Center for Depression, Anxiety & Stress Research at McLean Hospital. “If you perceive you can cope, you will not feel as stressed.”
The cognitive part of the CBT protocol can be a powerful tool too, teaching people to face their fears with a sort of existential shrug. “One of the problems of chronic worriers is that they tend to have predictions of catastrophic outcomes that crowd out their consciousness,” says UNC’s Wilson. A better approach is to accept that your performance or presentation might crash and burn and decide that even when such disasters occur, they’re not fatal. It’s how Jenny Allen, an actress currently appearing off-Broadway who used to be gripped by anxiety before every performance, learned to cope with her demons. “I was always thinking, I’m gonna forget my lines. Is the line ‘Where’s the hat?’ or ‘What have you done with the hat?’ I would get onstage clammy, sweating and feeling uptight, with shallow breathing.” Now she takes deep breaths and stays focused on the story she is telling.
Extreme anxiety can be managed in acute moments by drugs like Xanax, Valium and other benzodiazepines, which broadly suppress the activity of brain chemicals, but they can be addictive and do nothing to help sufferers acquire meaningful coping skills. Some antidepressants also have antianxiety properties and can often make people not helped by CBT more receptive to it. Eventually, better understanding of the neural pathways of anxiety will help pharmacologists develop more precisely targeted drugs. And a more thorough mapping of the brain’s genes–along with better epidemiological understanding of the heritability of anxiety conditions–can identify likely anxiety sufferers early on and help them learn coping skills that can make anxiety treatment preventive rather than therapeutic.
Until then, we could do worse than to follow the example of the very savvy, if very unscientific, Lewis. “I spend about 30 to 40 hours looking over thousands and thousands of ideas on my computer before a show, and I tell myself to let it go, have some confidence,” he says. “The anxiety will creep in there really fast, but I eventually embrace it and say enough is enough.”
More Must-Reads from TIME
- Donald Trump Is TIME's 2024 Person of the Year
- Why We Chose Trump as Person of the Year
- Is Intermittent Fasting Good or Bad for You?
- The 100 Must-Read Books of 2024
- The 20 Best Christmas TV Episodes
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- Merle Bombardieri Is Helping People Make the Baby Decision
Contact us at letters@time.com