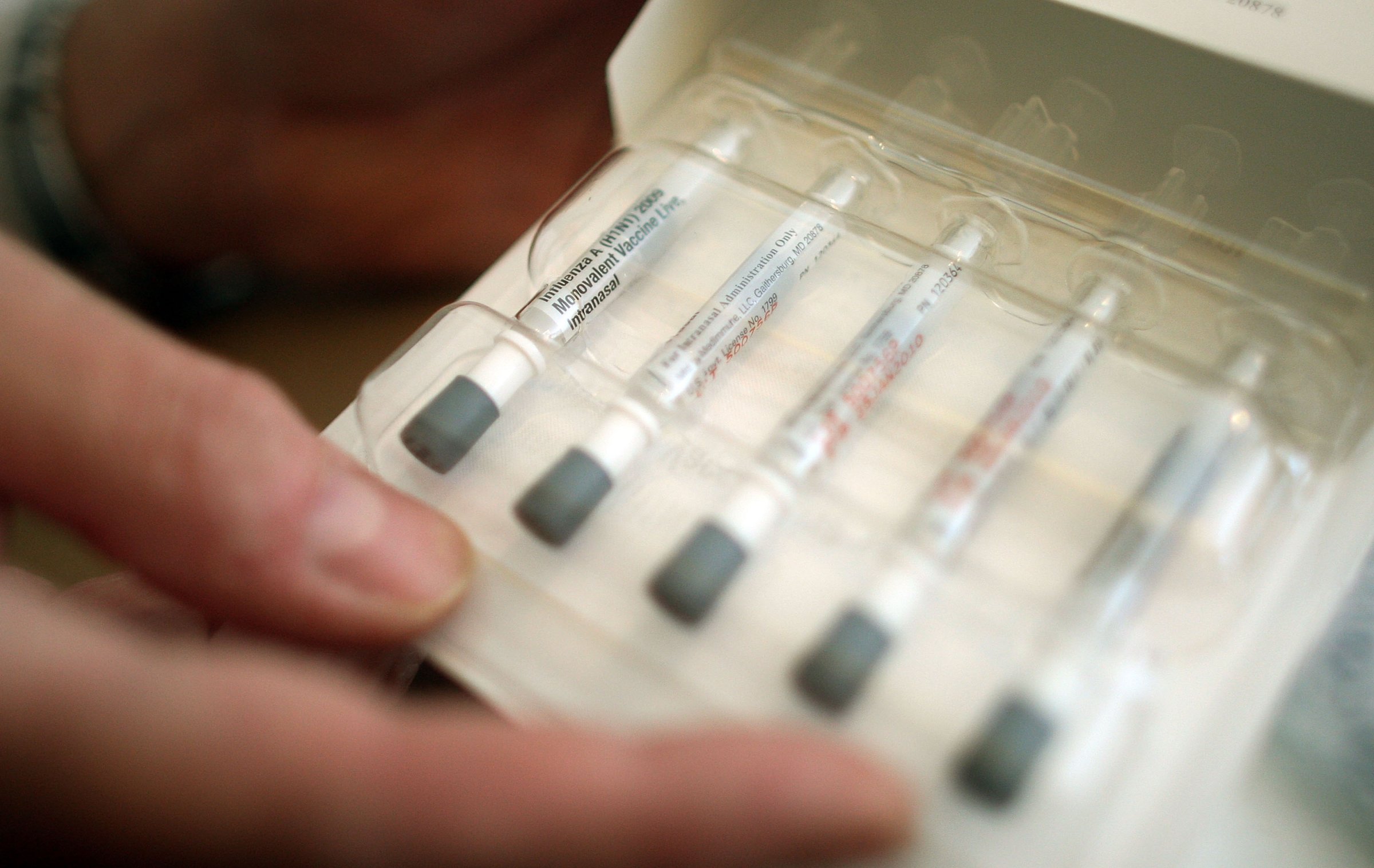
After a two-year hiatus, the nasal flu vaccine is set to return to doctors’ offices next year.
The Advisory Committee on Immunization Practices (ACIP) voted 12 to 2 on Wednesday to return the nasal spray to the CDC’s list of recommended vaccines for the 2018-2019 flu season. Pending final approval from the CDC director, the vote would greenlight the spray for widespread use and compel insurance companies to cover it. The committee stopped short of explicitly recommending the nasal spray, however, and will instead let providers and patients decide if they’ll use it instead of traditional flu shots.
There is one catch. Even though this year’s flu season is still in full swing, many providers have already purchased their supplies for the next one, STAT reports — so it may be too late for the spray, which is sold under the brand name FluMist, to make much of an impact next year.
Here’s what to know about the nasal flu vaccine.
How does the nasal flu vaccine work?
Unlike traditional flu shots, which do not contain live influenza virus, FluMist delivers a dose of influenza that helps the body mount an immune response, but is weakened to the point that it won’t cause infection, explains CDC Medical Officer Dr. Lisa Grohskopf.
And because FluMist is administered nasally, it may cut off disease transmission at the source, Grohskopf says. “One of the main mechanisms through which flu is thought to be spread is though respiratory droplets,” Grohskopf says. “One thing that you would be anticipating you’d get more of with the live virus vaccine is antibody production in your nose.”
Is the nasal flu vaccine more effective than the shot?
It’s hard to say. Grohskopf stresses that the CDC has not released any guidance as to whether the nasal spray or the flu shot is a better option. Still, she says some studies have suggested that the traditional flu shot is equally or slightly more effective than the nasal spray, at least in adults.
The picture is a little more complicated for children. Prior to the 2009 swine flu pandemic, research suggested that FluMist might be the better option for kids younger than six, Grohskopf says. But in the following years, the nasal spray failed to protect many children from the flu, and it was dropped from the CDC’s list of recommended vaccines after 2015-2016 data showed only 3% efficacy among children ages two to 17. For context, this year’s flu shot was 59% effective in children younger than eight.
“Something clearly changed with the pandemic, and we don’t know completely why,” Grohskopf says, though she adds that a failure to target the H1N1 strain of influenza seems to be the culprit. “The live virus vaccine did not work well against H1N1.”
AstraZeneca, the parent company of FluMist’s manufacturer, has since rejiggered the drug’s formulation to better target H1N1, and says early data suggests it will be more effective moving forward — though only time will tell.
“The specific question about H1N1 viruses won’t be answerable until we have another H1N1 season, and we can’t really predict when those will happen,” Grohskopf says.
Who should get the nasal flu vaccine?
Although FluMist is often seen primarily as an option for kids, “there isn’t a preference for one group to get one vaccine over another at this point,” Grohskopf says.
The needle-free option is approved for most people between ages 2 and 49. The only people who should steer clear are those with severe egg allergies, people who have had past life-threatening reactions to flu shots and kids who are also taking aspirin, AstraZeneca says. Grohskopf adds that live-virus vaccines are in general not recommended for pregnant women and those with suppressed immune systems.
Why is it so hard to make effective flu shots?
Many consumers were dismayed — and confused — to learn that the flu shot was only 36% effective this year, but that’s largely because the flu is difficult to predict. Different strains circulate each season, the season begins and ends at different times from year to year and certain areas and age groups may be hit much harder than others. Experts must assess these many moving parts when developing a vaccine in advance of flu season. That guesswork, combined with the imperfect science of actually making flu shots, leaves some room for error.
Efforts to make a universal flu vaccine are underway, but there’s a long way to go before they reach the public.
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Write to Jamie Ducharme at jamie.ducharme@time.com