In a small new study published in Science Translational Medicine, researchers who are pioneering an immune-based treatment for cancer report encouraging results among people with otherwise untreatable non-Hodgkin lymphoma, a blood cancer.
Led by Dr. Cameron Turtle from the Fred Hutchinson Cancer Research Center, the scientists gave a group of 32 people different chemotherapy regimens and then introduced immune cells specifically designed to target and destroy cancer cells. All of the patients had been given at least one traditional treatment, including some who had had stem cell transplants, but none had good responses to these approaches. After the immunotherapy, however, seven people in one treatment group went into complete remission, while another four saw their disease progress more slowly.
The treatment, called CAR-T cell therapy, is targeted toward blood cancers, where doctors can eliminate cancer cells and replace them with healthy blood and immune cells. The strategy hinges on two important steps. First, doctors need to remove as much of a patient’s cancer-ridden blood cells as possible — they do that with chemotherapy — in order to make room for a new population of healthy blood and immune cells. If too many of the cancer cells remain, then they could outcompete the new cells and simply destroy them. To ensure that doesn’t happen, Turtle and his team tested a two-drug chemotherapy regimen and compared it to a single drug chemo strategy. Those getting the combination showed the best results, amounting to a 64% complete remission rate; by comparison, only one of the people getting the single chemotherapy agent went into complete remission (an 8% rate).
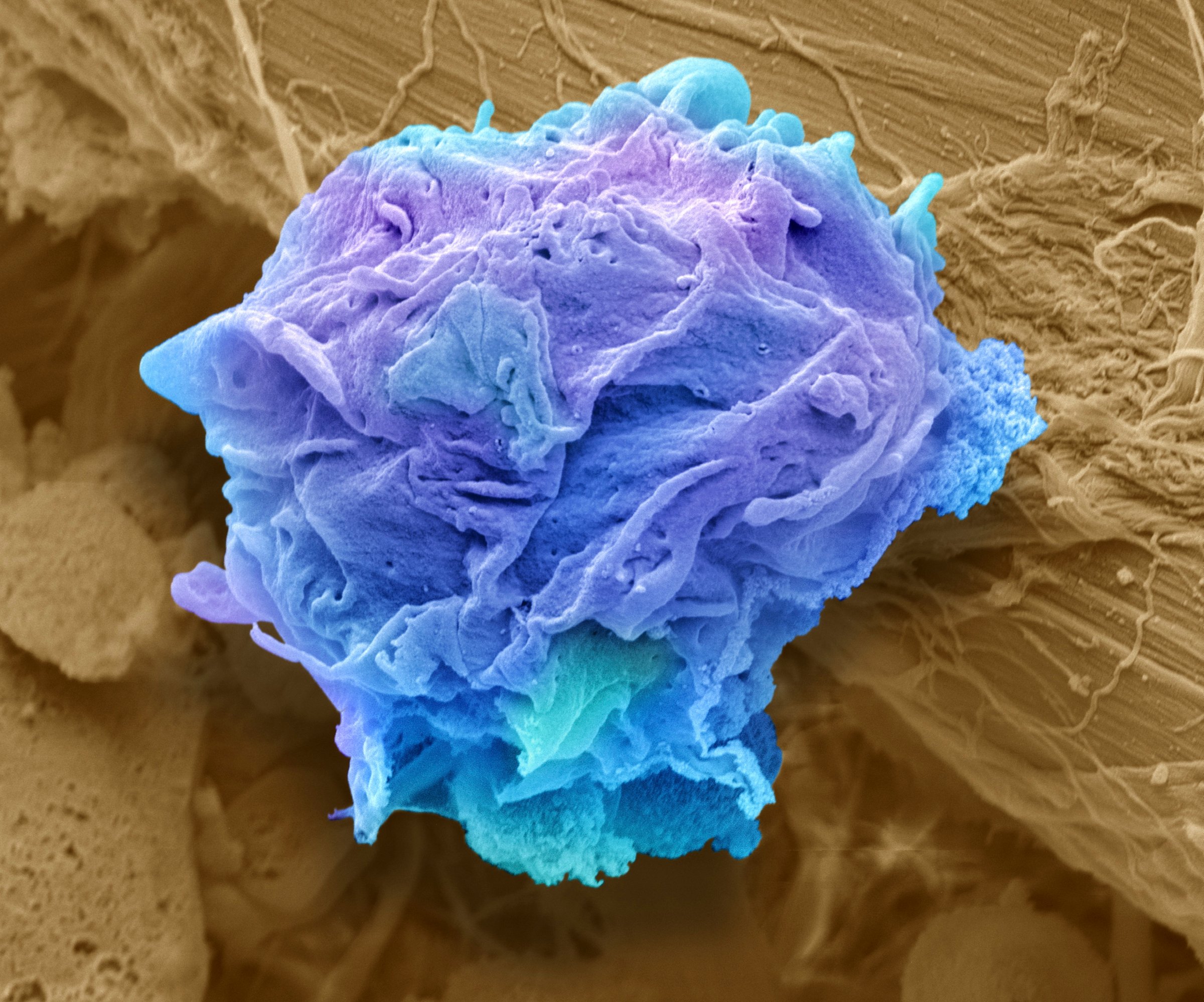
Next, the researchers need to re-introduce the right amount of the right immune cells that can fight cancer. Known as T cells, these contain specific receptors that allow some of them to recognize and bind to cancer cells and others to destroy them. To enhance the potency of the therapy, the scientists coaxed these cells to grow in the lab and genetically engineered them to express the tumor-specific receptor. The idea is to then reintroduce these cells back into patients and give them new, healthy blood cells that are cancer-free.
The results mirror those that the same researchers found among patients with other types of blood cell, or B-cell cancers, but are particularly encouraging since previous immunotherapy strategies haven’t been as robust when applied to non Hodgkin lymphoma. The trial provides additional support for the idea that immune cells can be properly trained to recognize and destroy cancer — in this case, with the help of genetically manipulated T cells. The results show that doctors can indeed tip the scales in favor of having the body fight cancer in much the same way it tackles pathogens like bacteria and viruses.
The results also provide much-needed information on how to optimize the strategy for different types of cancer. These findings suggest, for example, that for harder to treat non Hodgkin lymphoma, a combination chemotherapy to eliminate as much of the existing cancer as possible, before the immune cells are re-introduced, might be the key to helping more patients with the condition to slow the progression of their disease or even achieve remission.
While effective, the therapy also comes with a down side. Because the T cells are agents of destruction, they can trigger adverse effects such as fever and inflammation as they tackle the cancerous cells. Twenty of the 32 people in the trial developed signs of inflammation and low blood pressure, with four people getting severe enough symptoms that they required time in the intensive care unit and treatment with steroids. Two people also developed toxic effects from the treatment that resulted in tremor or language problems, but these were reversible. Two people given the highest dose of the T cell therapy died; one of bleeding and another from bleeding due to an intestinal mass.
The scientists are hopeful. however, that more studies will help them figure out the right chemotherapy regimen and the right dose of T cells to achieve the best results with the least adverse effects. “We’re very encouraged by these responses,” says Dr. Stanley Riddell, one of the co-authors from Fred Hutchinson. “These patients all failed conventional therapies; we were treating patients who didn’t have very many options for treatments. Obviously it’s still early days, and we need longer follow up and need to understand more about when in the patient’s disease course is the best time to use this kind of therapy, but we certainly think it’s encouraging.”
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- Coco Gauff Is Playing for Herself Now
- Scenes From Pro-Palestinian Encampments Across U.S. Universities
- 6 Compliments That Land Every Time
- If You're Dating Right Now , You're Brave: Column
- The AI That Could Heal a Divided Internet
- Fallout Is a Brilliant Model for the Future of Video Game Adaptations
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at letters@time.com