Majid Fotuhi built his first brain out of wood and foam. It was the best way, he thought, to help his fellow students at Harvard grasp how complex and beautiful the organ is. Fotuhi hired a pair of art-school students for the summer of 1993, and millimeters at a time, they sketched a dead human’s brain that Fotuhi schlepped back and forth between the neuroanatomy lab and the art studio across campus. By the time classes started that fall, they had turned their sketches into a 5-ft.-high replica that hinged open to reveal hundreds of discrete parts, including some purple blood vessels and a peach-colored cortex.
Decades later, Fotuhi, now a neurologist who specializes in the prevention of Alzheimer’s disease, remains intent on the organ. “It’s not this mysterious black box sitting up there, disconnected,” he says. “It’s tightly, tightly connected to the rest of the body, and you can take care of it the same way you can take care of your teeth.”
Fotuhi has long believed that doing just that–taking care of the brain as well as you take care of the rest of your body–can stave off cognitive decline. For most of his career, that thinking put him in the minority; neurologists, stumped by Alzheimer’s, have focused their efforts on trying to find a cure for the disease.
They have made progress, but doctors do not yet have a reliable way to treat dementia with drugs. At this rate, Alzheimer’s disease and other dementias are expected to cost the U.S. $1 trillion in health care costs by 2050.
That projection is dire, but a glut of new research presented at the Alzheimer’s Association International Conference in July suggests that a path paved by reasonable lifestyle choices–including exercise and targeted brain training–may indeed protect the brain as it ages. “I felt like jumping up and down in the middle of the conference hall,” says Fotuhi. “Diet, exercise, sleep and stress: those are generally not considered culprits for a problem as big as dementia. But for the first time, we have evidence that levels of tau”–thought to be a marker of Alzheimer’s–“can change with lifestyle interventions such as exercise. The whole thing is coming together.”
People have long puzzled over what causes some people to lose their mind in old age. In ancient times, dementia was believed to be an inevitable part of aging. Later, people thought it was a punishment from God for sin. Now, it’s mostly blamed on Alzheimer’s disease. Experts still don’t know exactly what causes Alzheimer’s, but in 1992 one idea, called the amyloid cascade hypothesis, took hold. It suggested that the excessive buildup of a protein in the brain–amyloid, which clumps together into plaques–is the main driver of Alzheimer’s. The buildup causes another protein, tau, to twist into tangles and cut off the supply of nutrients to brain cells, ultimately killing them. This hypothesis propelled the search for a pill that can stop these plaques and tangles from forming or undo them once they’re there.
The overproduction of amyloid is thought to be a cause of early-onset Alzheimer’s, which can affect the brains of people in their 40s and 50s. Little if anything can be done to prevent early-onset Alzheimer’s, though it is an active area of current research. But when it comes to the Alzheimer’s that most people think of–a disease of the elderly that causes confusion and memory loss–there is a lot that experts still do not agree on, including whether the single-minded focus on amyloid and tau has been right.
Scientists like Fotuhi like to point out that plaques and tangles are sometimes found in the brains of people who don’t have symptoms of dementia. Researchers in this camp often cite a story about Sister Mary, a tiny, social nun born in 1892 who had a thunderous laugh and taught until her death at age 101. In a late-1980s study of the lives and deaths of almost 700 elderly nuns, an autopsy revealed that Sister Mary’s brain was so full of amyloid plaques and tau tangles that she met the criteria for Alzheimer’s disease. Yet in life, her mind was reportedly sharp until the end.
Other research has suggested that amyloid isn’t enough to explain all–and possibly even most–Alzheimer’s cases. A 2015 article published in the journal Nature Neuroscience made the case for rejecting the entire amyloid cascade hypothesis. Meanwhile, other factors–such as heart health, sleep quality and physical activity–are emerging as potential ways to help prevent dementia in some people.
By taking factors like these more seriously, scientists are forming a whole new Alzheimer’s attack plan: improve the health of the heart and you’ll have a big impact on the brain. Lifestyle changes won’t ever eradicate the disease. But they may be the best prevention we know of right now.
In a 2014 article published in The Lancet Neurology, researchers projected that almost a third of the cases of Alzheimer’s disease worldwide–9.6 million of them–could be prevented by things that are within most people’s power to change: hypertension in middle age, diabetes, obesity, physical activity, depression, smoking and low education were all found to play a role.
Of these factors, heart health seems to be the most important. According to an estimate published in the journal Hypertension, if every middle-aged American with high blood pressure got properly treated for it, about 25% of dementia cases would be wiped out. “Given that we spend almost $200 billion a year dealing with dementia, 25% is a pretty big savings,” says Dr. Lon White, one of the authors of the Hypertension study and a neuroepidemiologist who spent much of his 50-year research career at the National Institutes of Health.
The link between the heart and the brain is logical when you think about it. “The brain is a sea of blood vessels,” Fotuhi says, and because neurons require a lot of oxygen to fire properly, the brain uses 20% of the blood pumped by the heart. “For that reason, anything that affects blood flow affects the brain.” When people have hypertension, obesity or Type 2 diabetes, the blood vessels don’t work as well, the flow isn’t as good, and the neurons become thirsty for oxygen.
Because heart disease is the No. 1 killer of Americans, doctors and public-health experts have focused their advice on heart health for the past 30 years, and today the rates of death from heart disease and stroke have declined. Researchers are now beginning to see a link outside the lab between stronger hearts and healthier minds. One study published in February in the New England Journal of Medicine dug into data from 5,205 people ages 60 and older who are part of the Framingham Heart Study, which has tracked dementia in its participants since 1975. Over the 30 years of data, the incidence of dementia in people with at least a high school diploma fell by 44%.
“We think heart-disease risk factors have a big effect on brain health,” says Dr. Kristine Yaffe of the University of California, San Francisco, who is a leading researcher on predictors of dementia. “Lifestyle factors are so important, even though they sound sort of soft, and a lot of people therefore think they can’t possibly be that effective. But I’m not so sure. They’re not expensive, they don’t have side effects, and they’re good for the rest of the body too. So why wouldn’t you make lifestyle changes?”
These natural interventions appear to have powerful effects on some parts of the brain that are vulnerable to aging. Consider the hippocampus, which is crucial to memory. It’s one of the first regions of the brain to shrivel when people age, shrinking by about 0.5% each year after age 40. A smaller hippocampus helped researchers predict who would develop Alzheimer’s disease in some studies. This brain region can also grow, however. When older adults without dementia were assigned to do aerobic exercise or light stretching for a year, the people in the stretching group lost 1.4% of their hippocampus, but those in the exercise group grew their hippocampus by 2%–the equivalent of reversing cognitive loss by about two years. Meditation has also been shown to increase the size of the hippocampus.
Dementia appears to plant its roots in the brain decades before a diagnosis, which is why many leaders in the field are looking for ways to detect it at the onset of the disease, not after problems start. Similarly, Fotuhi and his colleagues think that the earlier that people begin preventive measures, the better.
That said, it’s never too late to adopt a healthy lifestyle. A randomized controlled trial presented at the Alzheimer’s Association conference showed that even sedentary elderly people with mild cognitive impairment can improve their brains by starting to exercise.
With a trainer, half of the 70 adults in the study did 45 minutes of high-intensity aerobic exercise four times a week, while the control group did light stretching. After just six months, the active adults improved in tests of executive function, which rules tasks like organization and attention, compared with those in the control group. “It says that aerobic exercise is potentially antiaging, in a sense,” says lead researcher Laura Baker of Wake Forest Baptist Medical Center. The study also found that tau protein was significantly reduced in the oldest people in the aerobic group. “To us, this is a phenomenal finding, because there is no drug trial that’s ever been conducted to show that any drug now can reduce tau protein in cerebrospinal fluid,” Baker says.
At Fotuhi’s neurology practice in Virginia, the NeuroGrow Brain Fitness Center, he gives each patient a battery of cognitive tests to see their strengths and weaknesses, then puts them through a three-month boot camp that costs $6,000 to $7,000, depending on insurance coverage. People learn how to exercise, meditate, eat a Mediterranean diet, reduce stress and improve their sleep. They also play brain games that are tailored to their individual weaknesses, go through cognitive behavioral therapy and have hours-long sessions of neurofeedback, a technique that allows patients to see their brain activity in real time and modify their reactions with the help of a practitioner.
Fotuhi and his colleagues tallied the effects in the Journal of Prevention of Alzheimer’s Disease. Of 127 older patients with mild cognitive impairment, 84% showed significant improvement in at least three areas of cognitive function. Of the 17 who had an MRI both before and after the study, eight had some shrinking or no growth in the hippocampus, but nine saw theirs grow by at least 1%. Fotuhi says he’s taking his program nationwide.
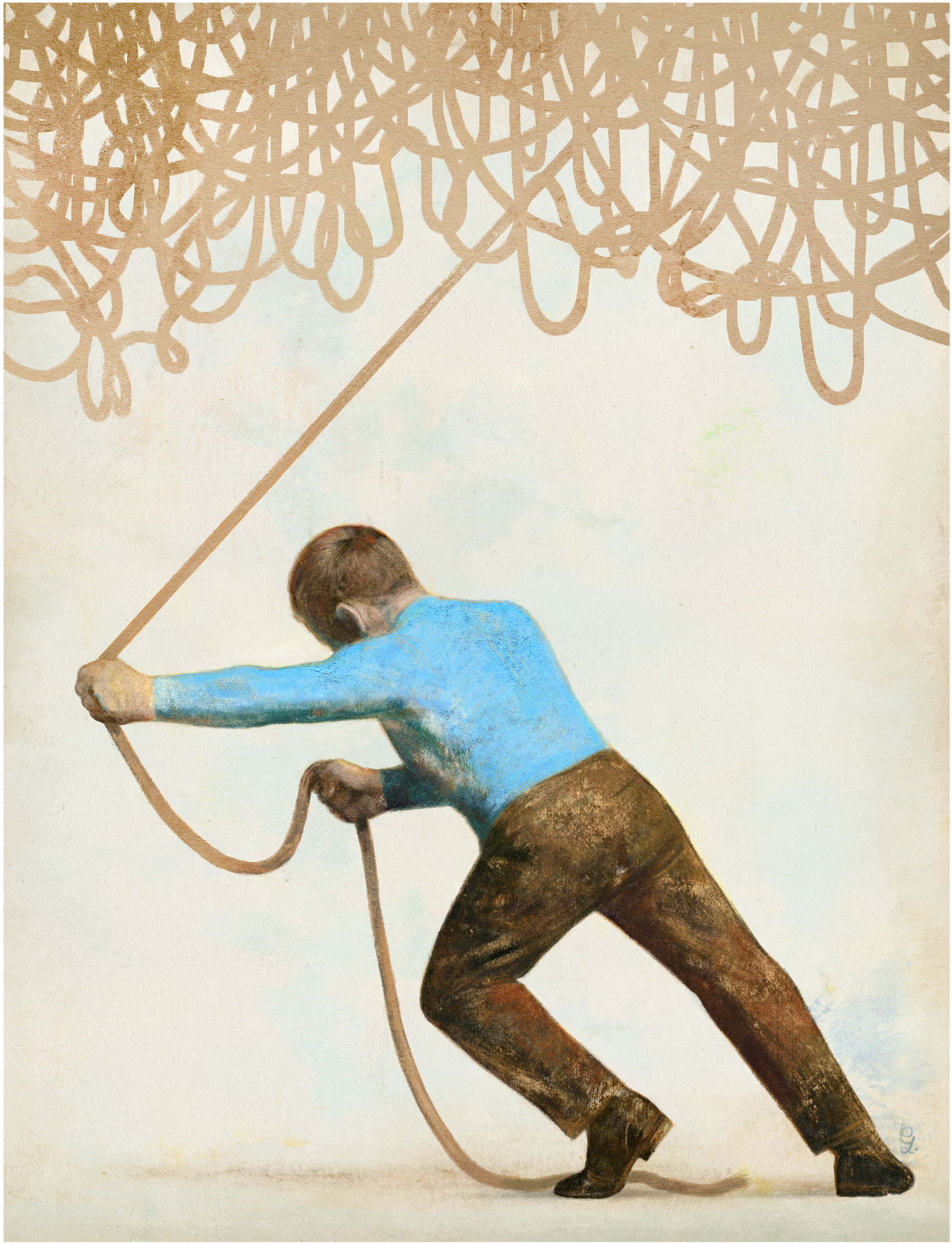
It is still too early to know if interventions like these prevent Alzheimer’s disease in the long run. “The frustrating part to me is we have a lot of treatable conditions in our patients and we’re just focusing on the nontreatable part of their pathology,” Fotuhi says. “We need to change the conversation to be about what causes better or worse brain health.”
The fact that we can’t yet treat it is only one frustrating part of the disease. Just knowing what it is remains another challenge: a March analysis of data from two long-term brain-autopsy studies revealed that what doctors diagnose as Alzheimer’s disease in life looks a lot less obvious in the brain after death. Few people died with brain lesions indicative of pure Alzheimer’s–suggesting that what we presume to be Alzheimer’s may not, in fact, be Alzheimer’s at all but rather a combination of several additional diseases experts know little about.
“It’s like being stuck with cancer but not being able to tell whether it’s liver cancer or pancreatic cancer,” says White, who was an author of the Hypertension study. At this stage, it’s proving difficult for researchers to figure out how many additional brain diseases there may be as well as how to treat them.
But the good news is that there is at least a suggested path. “My prediction is that one day, hopefully, Alzheimer’s will be handled like cardiovascular disease,” says UCSF researcher Yaffe, “with a combination of drugs and lifestyle factors.”
More Must-Reads from TIME
- Why Trump’s Message Worked on Latino Men
- What Trump’s Win Could Mean for Housing
- The 100 Must-Read Books of 2024
- Sleep Doctors Share the 1 Tip That’s Changed Their Lives
- Column: Let’s Bring Back Romance
- What It’s Like to Have Long COVID As a Kid
- FX’s Say Nothing Is the Must-Watch Political Thriller of 2024
- Merle Bombardieri Is Helping People Make the Baby Decision
Write to Mandy Oaklander at mandy.oaklander@time.com