
In November 2013, MaryAnn Anselmo—who was on the cover of TIME in March—heard the words that most of us dread the most: she had cancer. Worse, it was stage 4 glioblastoma, a particularly aggressive brain tumor that often takes a patient’s life in a matter of months. Having just recovered from a devastating car accident, Anselmo thought, “Somebody wants me dead here.”
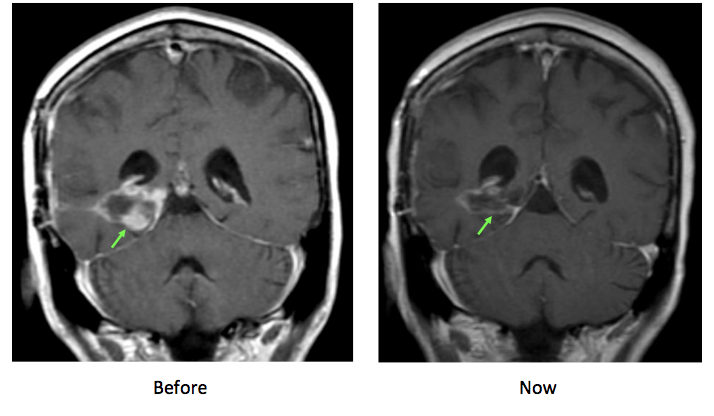
Nearly two years later, the New Jersey resident is receiving some completely different, and more welcome news. “The latest scan doesn’t show any tumor any more,” her physician, Dr. David Hyman, acting director of Developmental Therapeutics ad Memorial Sloan Kettering Cancer Center (MSKCC), tells TIME. The results from Hyman’s most recent study, which Anselmo participated in, is published in the latest issue of the New England Journal of Medicine (NEJM).
“I’m tired all the time,” she says, “but I’m dealing with it, living with it. I feel awesome compared to what this tumor could have done to me.”
MORE: The Cancer Gap
Hyman is reluctant to call it a “cure” for certain cancers—the burden of proof is higher than this one study or this one patient—but Anselmo’s cancer is gone. And for that, Anselmo can thank something called a basket trial, a new way for doctors to test promising cancer treatments that more precisely target the right therapies to the right patients at the right time. This is the first such trial of its kind.
The trial puts the idea of precision medicine to the test. At 23 cancer centers around the world, 122 patients with advanced cancer signed up for a last-resort treatment covered in the new study. All had their tumor genomes sequenced, so doctors could get a better sense of which mutations were driving the cancers, and whether there were any targeted therapies for those mutations.
Anselmo had three mutations fueling the growth in her brain, but she and her doctors at MSKCC decided to focus on one, called BRAF. A recently approved drug to treat BRAF mutations in melanoma helped shrink or halt tumor growth in half of treated patients, so doctors wanted to know whether the drug could help patients with the same mutation but with different kinds of cancer, like Anselmo. But while BRAF mutations occur in about 50% of melanoma cases, they are much rarer in other types of cancers. So creating a trial for patients like Anselmo would take both time and money that researchers couldn’t justify.
A basket trial, however, capitalizes on the growing understanding that cancers should be characterized by not just where they start (in the breast, colon or lung, for example) but also by how they grow — which mutations are driving them. A basket trial collects patients, all of whom have BRAF mutations, for instance, but who might have different types of cancer.
In the NEJM study, patients with non small cell lung cancer, colon cancer, thyroid cancer, multiple myeloma and, glioblastomas, among others, were included. By studying them as a group, Hyman says it’s possible to get a better idea of how feasible it is to target mutations like BRAF among those who don’t have melanoma.
So far, the results are encouraging. Patients with non small cell lung cancer seemed to have the best response rate to vemurafenib, 42%, after a year. More than 70% of the patients with this cancer saw their tumors shrink by at least 30% in length. There were promising signs that patients with the other, untreatable cancers also responded and took longer before their tumors progressed than they would have without the experimental therapy.
Anselmo was among the extraordinary responders. “It is unusual,” says Hyman of the apparent shrinkage of her tumor. “She really is an outlier in any way you measure it.”
But it’s precisely for patients like Anselmo that basket trials are being considered — the possibility that there may be one, two or however many patients who, rather than facing a poor prognosis with existing or non-existent options for treating their disease, may have a chance, however small, of living longer and even controlling their cancer.
“One of the things that gets lost when we talk averages and medians is how many patients benefit and for how long,” says Hyman. “There is a tremendous range and a concern that promoting the best successes sets the bar very high. But it also lets people know that things are not entirely hopeless, that there are people who have tremendous benefit from therapies and not get completely caught up in medians and averages.”
That being said, Hyman cautions that more work needs to be done to better apply the principles of precision medicine to improve patients’ outcomes. Since most tumors have many mutations, how can doctors determine which one, or ones, to target with drugs? Why do some patients respond very well, while others do not?
Another looming question has to do with how cancer doctors can start to incorporate what they are learning about mutations and cancer-causing pathways with their more traditional knowledge based on where tumors start. In the study, for example, patients with BRAF colon cancers did not respond to vemurafenib; but some started to show responses when vemurafenib was combined with another drug, cetuximab. That suggests that knowing where the cancer originates may still be an important part of the puzzle in figuring out which treatments might work best for which types of cancers.
In an editorial accompanying the study, researchers at the T.H. Chan Harvard School of Public Health and Boston University note that basket trials may be just the first step in a precision medicine approach to cancer. Once doctors figure out which types of cancers might respond best to, for example, a BRAF-focused drug, they might conduct additional trials on each of these cancers to determine which patients, like Anselmo, would benefit most.
For her, the trail has provided the chance to sing again. A jazz vocalist, she performed at a friend’s birthday party and attended a song-writing retreat in upstate New York. She makes weekly visits to her doctors — to the dermatologist to monitor any side effects from the drug, to Hyman every two months for a brain scan, and to get lab tests done to check on her immune system. And she’s tired all the time. “But that’s par for the course,” she says. “I’m just lucky to be alive at a time when cancer care is so different than it was years ago. Who would have known that treatments could be so customized? It’s so amazing, and I’m very thankful to be a part of it.”
More Must-Reads from TIME
- Where Trump 2.0 Will Differ From 1.0
- How Elon Musk Became a Kingmaker
- The Power—And Limits—of Peer Support
- The 100 Must-Read Books of 2024
- Column: If Optimism Feels Ridiculous Now, Try Hope
- The Future of Climate Action Is Trade Policy
- FX’s Say Nothing Is the Must-Watch Political Thriller of 2024
- Merle Bombardieri Is Helping People Make the Baby Decision
Contact us at letters@time.com