Scientists have been warning for decades that we use too many antibiotics, both in people to treat relatively mild infections and in agriculture to bulk up farm animals and keep them free of disease. The consequences, they caution, are dire—and already emerging in hospitals with bacteria that can’t be treated with any of our existing antibiotic medications.
But the thinking went that to become resistant to the drugs we use on them, bacteria have to pay a price. They may be able to survive the pharmaceutical onslaught, but they’re less fit and therefore less able to reproduce, less likely to remain for long in their host of choice and otherwise sapped of the energy needed to really wreak havoc on human or animal immune systems.
MORE: Study Links Widely Used Pesticides to Antibiotic Resistance
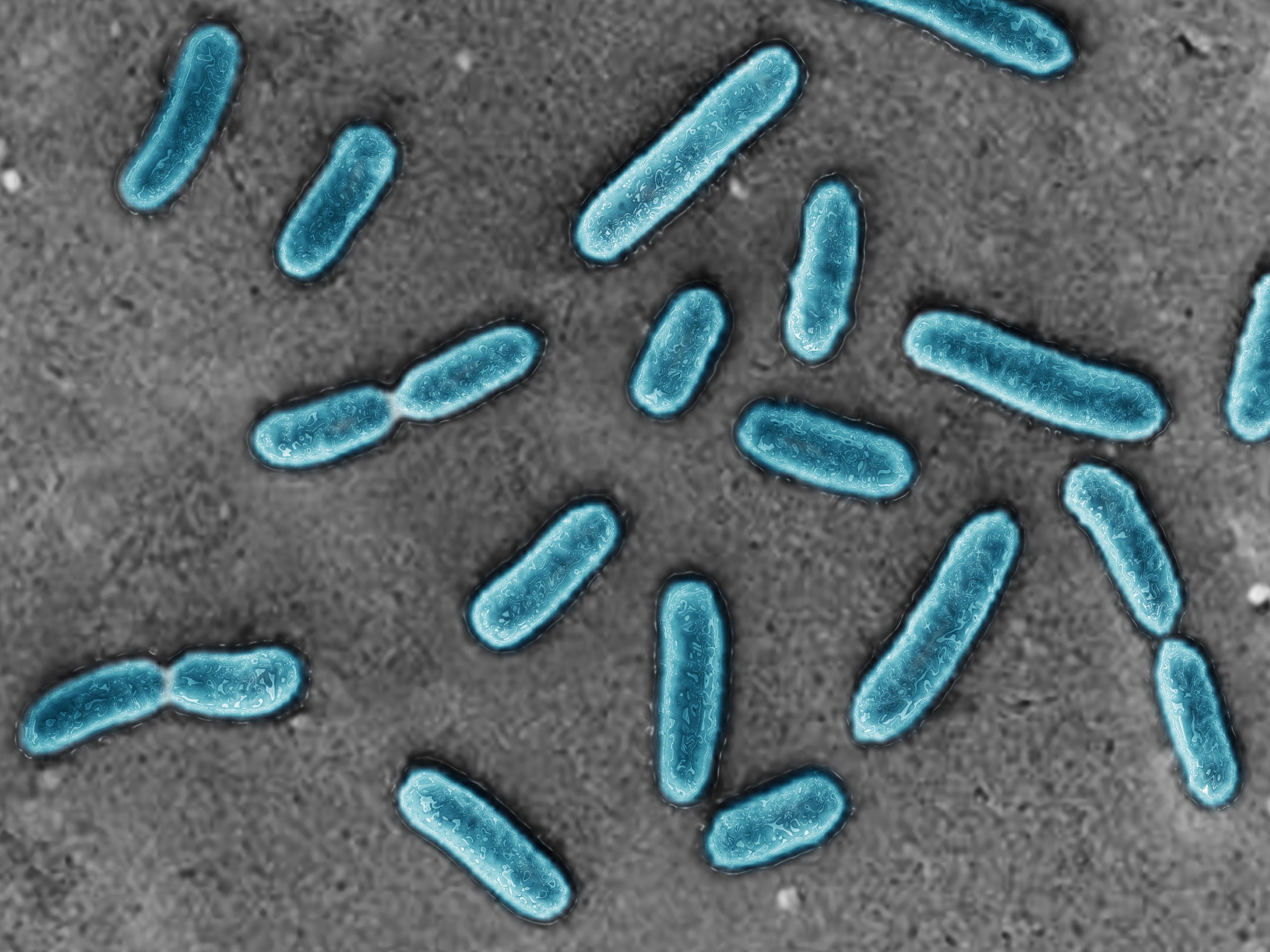
At least, that was the theory (and perhaps the hope) until now. In a study published in Science Translational Medicine, however, researchers show how misguided that belief is. Delving into the genetic code of certain common bacteria such as Pseudomonas aeruginosa and Acinetobacter baumannii — both of which are resistant to multiple antibiotics— and Vibrio cholerae, the researchers identified genes that change in the presence of these drugs. In animal models, they observed how these changes affected the different bacteria’s ability to infect and populate in hosts.
To their surprise, rather than being compromised, the antibiotic-resistant bacterial strains seemed to be stronger, more robust and better able to infect cells than less resistant strains.
MORE: Why Reducing Antibiotic Resistance Is Harder Than It Seems
“With all the possible mutations in the bacteria, there is a battle royale, a competition among all the mutants, and we see that the most fit, the most virulent were the ones that were resistant to the antibiotics,” says Dr. David Skurnik, senior author of the paper and assistant professor of medicine at Brigham and Women’s Hospital and Harvard Medical School. In the case of P. aeruginosa, he says, “the acquisition of antibiotic resistance was associated with the most increased fitness in all the possible mutations in P. aeruginosa.”
That means that the problem of antibiotic-resistant bugs just got more complicated. Overuse of antibiotics increases the number of bacterial strains that have mutations which make them better able to withstand the drugs, and this latest research shows that these strains may also be more adept at infecting hosts and causing disease. “We’ve gotten a double whammy with the acquisition of antibiotic resistance,” says Gerald Pier, a co-author of the paper and professor of medicine, microbiology and immunobiology at Brigham and Harvard Medical School. “Not only does antibiotic resistance make it more difficult to treat infections because we have fewer drugs they will respond to, but it makes the organism better able to cause infection.”
While still important, the conventional solution of cutting back on antibiotic use may not be enough, he says. Using antibiotics more appropriately will certainly reduce the appearance of new drug-resistant strains, but it won’t be enough to tamp down the emergence of these fitter, more virulent bacteria that also happen to be adept at evading the effects of antibiotics. For that, he says, other infection-fighting strategies, including boosting the immune system with vaccines or antibody treatments, may be needed.
That’s what Pier and Skurnik are working on currently, and so far, they’ve developed encouraging options for treating infections that may keep the more robust bacteria at bay. They’re targeting parts of bacteria that many strains have in common and developing new says to recognize these targets and neutralize the bacteria so they can’t cause serious infections and disease. “These results show that, yes, the problem of multi-drug resistant bacteria is more complex than we thought, but there are solutions,” says Skurnik.
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com