As a mathematical epidemiologist, I can tell you that — despite the publicity over the first U.S. case of Ebola, in Dallas — there is some good news in the Ebola outbreak ravaging West Africa: Ebola is not spreading nearly as fast as some scourges of the past.
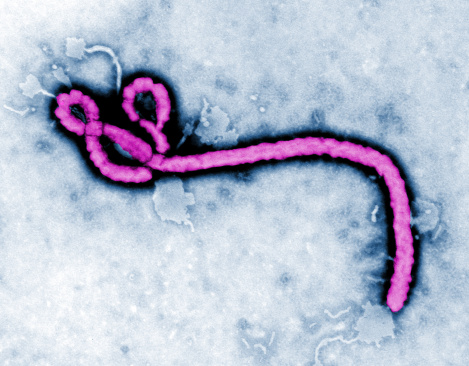
I first worked on Ebola back in 2004 at Cornell University (and in collaboration with the Los Alamos National Laboratory) as part of my doctoral dissertation modeling how the virus is transmitted. Ebola was an interesting case study for our mathematical modeling of the spread of disease, as there were two relatively large and well-documented outbreaks where the impact of efforts to control the virus was evident (the 1995 outbreak in the Democratic Republic of Congo — formerly known as Zaire — and the 2000 outbreak in Uganda). It was intriguing — not to mention scary — to work on a disease that produced such a set of horrific symptoms with a fatality rate above 50 percent.
But I learned then that Ebola isn’t the fastest-spreading disease in human history. That distinction goes to measles. In the era prior to 1963, when children were first routinely vaccinated, each case of measles created 17 new secondary cases, with transmission spreading like wildfire in schools, especially. It was lethal in 1 out of every 3 to 4 cases. At this rate, getting infected with measles during childhood was inevitable and so were deaths.
Of course, this reproductive rate isn’t the whole story of epidemics. Each case of the “Spanish Flu” — which caused the pandemic of 1918 to 1920 that many call the worst in recent history — produced between two and five additional victims. While that’s much lower than measles, Spanish Flu was still able to spread worldwide because of the speed at which it moved, also known as its generation interval. Only two to three days elapsed between the first case and a generation of secondary cases. In other words, it doesn’t take long for the flu virus to settle into a new host and a substantial number of transmissions can occur even before a person realizes that he or she has the flu. An estimated 30 to 50 million people around the world died from the Spanish Flu.
The good news is that Ebola has a lower reproductive rate than measles in the pre-vaccination days or the Spanish flu. Our 2004 work, which produced the first estimates for Ebola’s reproductive rate by using mathematical modeling and epidemiological data from the Central African outbreaks, found that each case of Ebola produced 1.3 to 1.8 secondary cases on average. This ongoing outbreak, a colleague and I recently found, has a reproductive rate that is about the same as the last one. It hasn’t become more transmissible in the more than 10 years it was lying low — and humankind has experience in dealing with it.
What’s more, the time that elapses between the first Ebola case and the generation of secondary cases is about two weeks. This should allow plenty of time to identify those who are sick and protect people who might come in contact with them. Individuals with Ebola are only contagious and able to transmit the virus when they are showing symptoms, which occurs about a week after they are first exposed to the virus.
To break the chain of the current Ebola outbreak, our numbers show that healthcare workers need to halt about 50 percent of infectious contacts by effectively isolating people who are infectious. (Vaccinating at least some of the population would be another option — but there is no licensed vaccine available).
The trouble in West Africa is that the countries suffering from outbreaks have weak healthcare systems — perhaps too weak to halve the number of infectious contacts. These countries lack gloves, gowns, face masks, and other essential supplies to protect nurses and doctors from infection, and they also don’t have an adequate surveillance system to catch and identify Ebola cases in a timely way. The number of doctors and health centers is small as well.
As a result, Ebola has spread with very little resistance and the rate of new infections from month to month has risen in Liberia and Sierra Leone, in particular. The rate for new cases of Ebola in Guinea has not risen as much, which suggests that Liberia and Sierra Leone have missed badly needed opportunities to control the outbreak.
Nigeria’s ability to break the chain of Ebola is also worth noting. Health authorities detected the first Ebola case in their country only three days after that person’s arrival in Nigeria from Liberia by airplane and acted quickly to isolate infectious individuals and trace their potential contacts. Nigeria has observed 20 cases where Ebola was transmitted, with no new cases reported since September 8, 2014.
Up until this year, textbooks have described Ebola as the type of infectious disease that could cause no more than a few hundred cases in hard-to-reach forested areas of Central Africa. Little attention or funding has been focused on Ebola, unfortunately, since health policymakers thought it would never escape its remote home base and infect large numbers of people. But while the virus has not changed much in more than a decade, many parts of Africa are very different. People live in much denser quarters where the introduction of a new disease is now more likely to take off. The population is also much more mobile than ever before. This increases opportunities for the virus to reach new areas where new chains of transmission can grow and become established.
Math and history show us that decisive efforts to isolate those who are infected with Ebola and to follow up quickly with the potential contacts of the infected can help to get an outbreak under control. We’re lucky that we have such capacities in the United States; even with the Ebola case in Dallas, the epidemic should not get much of a foothold here. But our world is interconnected in ways it never was before and diseases that require substantial contact to spread aren’t the only things circulating. If a virus like Ebola can quickly flare out of control, consider the impacts of a novel strain of influenza.
Gerardo Chowell-Puente is associate professor of mathematical epidemiology at the School of Human Evolution and Social Change, at Arizona State University. He is also a research fellow with the Division of International Epidemiology and Population Studies at the National Institutes of Health’s Fogarty International Center.
More Must-Reads from TIME
- Why Trump’s Message Worked on Latino Men
- What Trump’s Win Could Mean for Housing
- The 100 Must-Read Books of 2024
- Sleep Doctors Share the 1 Tip That’s Changed Their Lives
- Column: Let’s Bring Back Romance
- What It’s Like to Have Long COVID As a Kid
- FX’s Say Nothing Is the Must-Watch Political Thriller of 2024
- Merle Bombardieri Is Helping People Make the Baby Decision
Contact us at letters@time.com