
When our heads hit the pillow every night, we tend to think we’re surrendering. Not just to exhaustion, though there is that. We’re also surrendering our mind, taking leave of our focus on sensory cues, like noise and smell and blinking lights. It’s as if we’re powering ourselves down like we do the electronics at our bedside–going idle for a while, only to spring back into action when the alarm blasts hours later.
That’s what we think is happening. But as scientists are now revealing, that couldn’t be further from the truth.
In fact, when the lights go out, our brains start working–but in an altogether different way than when we’re awake. At night, a legion of neurons springs into action, and like any well-trained platoon, the cells work in perfect synchrony, pulsing with electrical signals that wash over the brain with a soothing, hypnotic flow. Meanwhile, data processors sort through the reams of information that flooded the brain all day at a pace too overwhelming to handle in real time. The brain also runs checks on itself to ensure that the exquisite balance of hormones, enzymes and proteins isn’t too far off-kilter. And all the while, cleaners follow in close pursuit to sweep out the toxic detritus that the brain doesn’t need and which can cause all kinds of problems if it builds up.
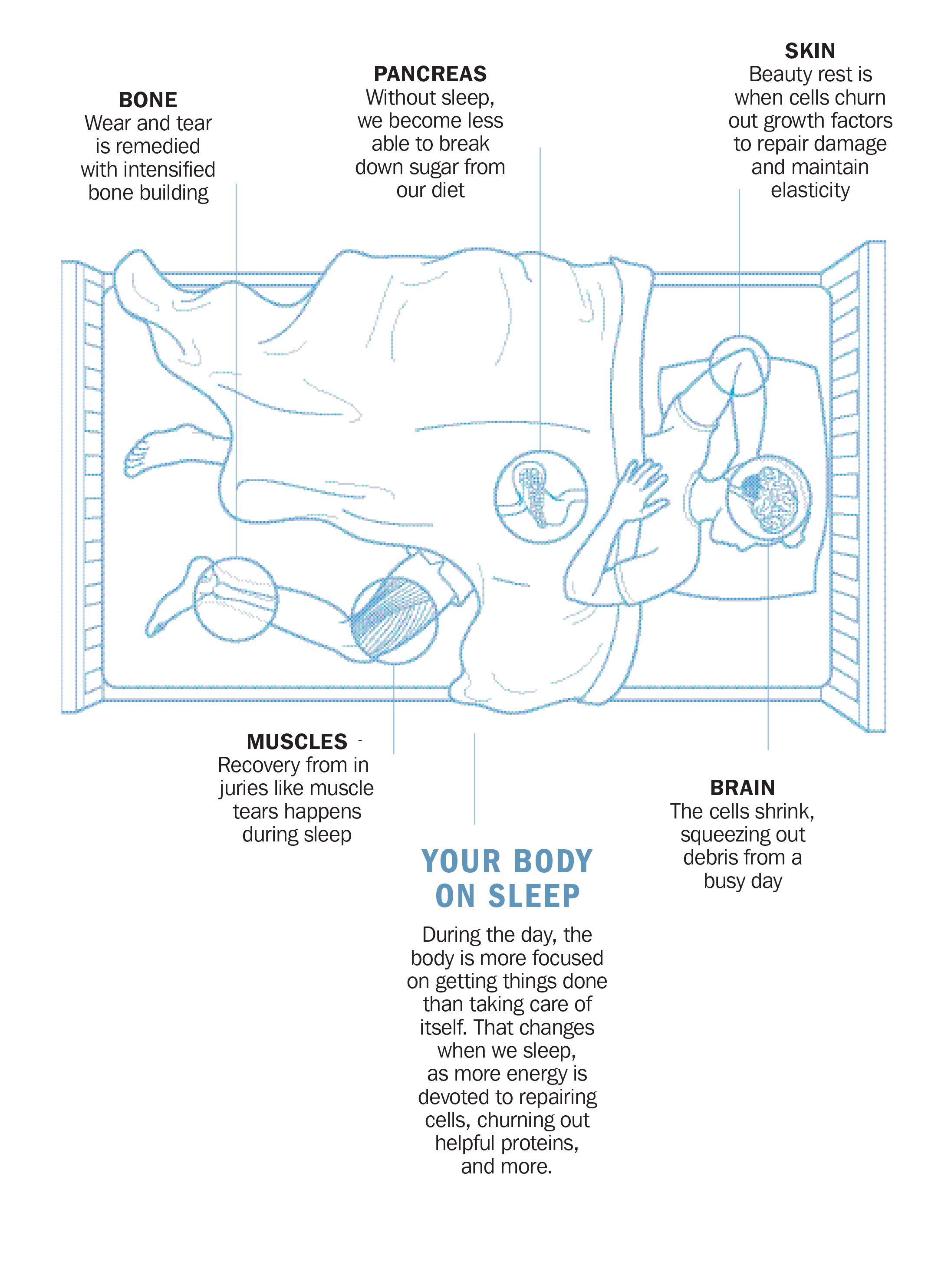
This, scientists are just now learning, is the brain on sleep. It’s nature’s panacea, more powerful than any drug in its ability to restore and rejuvenate the human brain and body. Getting the recommended seven to eight hours each night can improve concentration, sharpen planning and memory skills and maintain the fat-burning systems that regulate our weight. If every one of us slept as much as we’re supposed to, we’d all be lighter, less prone to developing Type 2 diabetes and most likely better equipped to battle depression and anxiety. We might even lower our risk of Alzheimer’s disease, osteoporosis and cancer.
The trouble is, sleep works only if we get enough of it. While plenty of pills can knock us out, none so far can replicate all of sleep’s benefits, despite decades’ worth of attempts in high-tech pharmaceutical labs.
Which is why, after long treating rest as a good-if-you-can-get-it obligation, scientists are making the case that it matters much more than we think. They’re not alone in sounding the alarm. With up to 70 million of us not getting a good night’s sleep on a regular basis, the Centers for Disease Control and Prevention considers insufficient sleep a public-health epidemic. In fact, experts argue, sleep is emerging as so potent a factor in better health that we need a societal shift–and policies to support it–to make sleep a nonnegotiable priority.
The consequences of skimping
Despite how great we feel after a night’s rest–and putting aside what we now know about sleep’s importance–we stubbornly refuse to swallow our medicine, pushing off bedtime and thinking that feeling a little drowsy during the day is an annoying but harmless consequence. It’s not. Nearly 40% of adults have nodded off unintentionally during the day in the past month, and 5% have done so while driving. Insomnia or interrupted sleep nearly doubles the chances that workers will call in sick. And half of Americans say their uneven sleep makes it harder to concentrate on tasks.
Those poor sleep habits are trickling down to the next generation: 45% of teens don’t sleep the recommended nine hours on school nights, leading 25% of them to report falling asleep in class at least once a week, according to a National Sleep Foundation survey. It’s a serious enough problem that the American Academy of Pediatrics recently endorsed the idea of starting middle and high schools later to allow for more adolescent shut-eye.
Health experts have been concerned about our sleep-deprived ways for some time, but the new insights about the role sleep plays in our overall health have brought an urgency to the message. Sleep, the experts are recognizing, is the only time the brain has to catch its breath. If it doesn’t, it may drown in its own biological debris–everything from toxic free radicals produced by hard-working fuel cells to spent molecules that have outlived their usefulness.
“We all want to push the system, to get the most out of our lives, and sleep gets in the way,” says Dr. Sigrid Veasey, a leading sleep researcher and a professor of medicine at Perelman School of Medicine at the University of Pennsylvania. “But we need to know how far we can really push that system and get away with it.”
Veasey is learning that brain cells that don’t get their needed break every night are like overworked employees on consecutive double shifts–eventually, they collapse. Working with mice, she found that neurons that fire constantly to keep the brain alert spew out toxic free radicals as a by-product of making energy. During sleep, they produce antioxidants that mop up these potential poisons. But even after short periods of sleep loss, “the cells are working hard but cannot make enough antioxidants, so they progressively build up free radicals and some of the neurons die off.” Once those brain cells are gone, they’re gone for good.
After several weeks of restricted sleep, says Veasey, the mice she studied–whose brains are considered a good proxy for human brains in lab research–“are more likely to be sleepy when they are supposed to be active and have more difficulty consolidating [the benefits of] sleep during their sleep period.”
It’s the same thing that happens in aging brains, she says, as nerve cells get less efficient at clearing away their garbage. “The real question is: What are we doing to our brains if we don’t get enough sleep? If we chronically sleep-deprive ourselves, are we really aging our brains?” she asks. Ultimately, the research suggests, it’s possible that a sleep-deprived brain belonging to a teen or a 20-year-old will start to look like that of a much older person.
“Chronic sleep restriction is a stress on the body,” says Dr. Peter Liu, professor of medicine at Harbor-UCLA Medical Center and L.A. Biomedical Research Institute. And the cause of that sleep deprivation doesn’t always originate in family strife, financial concerns or job-related problems. The way we live now–checking our phones every minute, hyperscheduling our days or our kids’ days, not taking time to relax without a screen in front of our faces–contributes to a regular flow of stress hormones like cortisol, and all that artificial light and screen time is disrupting our internal clocks. Simply put, our bodies don’t know when to go to sleep naturally anymore.
This is why researchers hope their new discoveries will change once and for all the way we think about–and prioritize–those 40 winks.
Garbagemen for your brain
“I was nervous when I went to my first sleep conference,” says Dr. Maiken Nedergaard, the chatty and inquisitive co-director of the Center for Translational Neuromedicine at the University of Rochester. “I was not trained in sleep, and I came to it from the outside.” In fact, as a busy mother and career woman, she saw sleep the way most of us probably do: as a bother. “Every single night, I wanted to accomplish more and enjoy time with my family, and I was annoyed to have to go to bed.”
Because she’s a neuroscientist, however, Nedergaard was inclined to ask a seemingly basic question: Why do our brains need sleep at all? There are two competing evolutionary theories. One is that sleeping organisms are immobile and therefore less likely to be easy targets, so perhaps sleep provided some protection from prey. The time slumbering, however, took away from time spent finding food and reproducing. Another points out that sleeping organisms are oblivious to creeping predators, making them ripe for attack. Since both theories seem to put us at a disadvantage, Nedergaard thought there had to be some other reason the brain needs those hours offline.
All organs in the body use energy, and in the process, they spew out waste. Most take care of their garbage with an efficient local system, recruiting immune cells like macrophages to gobble up the garbage and break it down or linking up to the network of vessels that make up the lymph system, the body’s drainage pipes.
The brain is a tremendous consumer of energy, but it’s not blanketed in lymph vessels. So how does it get rid of its trash? “If the brain is not functioning optimally, you’re dead evolutionarily, so there must be an advantage to exporting the garbage to a less critical organ like the liver to take care of it,” says Nedergaard.
Indeed, that’s what her research shows. She found that an army of previously ignored cells in the brain, called glial cells, turn into a massive pump when the body sleeps. During the day, glial cells are the unsung personal assistants of the brain. They cannot conduct electrical impulses like other neurons, but they support them as they send signals zipping along nerve networks to register a smell here and an emotion there. For decades, they were dismissed by neuroscientists because they weren’t the actual drivers of neural connections.
But Nedergaard found in clinical trials on mice that glial cells change as soon as organisms fall asleep. The difference between the waking and sleeping brain is dramatic. When the brain is awake, it resembles a busy airport, swelling with the cumulative activity of individual messages traveling from one neuron to another. The activity inflates the size of brain cells until they take up 86% of the brain’s volume.
When daylight wanes and we eventually fall asleep, however, those glial cells kick into action, slowing the brain’s electrical activity to about a third of its peak frequency. During those first stages of sleep, called non-REM (rapid eye movement), the firing becomes more synchronized rather than haphazard. The repetitive cycle lulls the nerves into a state of quiet, so in the next stage, known as REM, the firing becomes almost nonexistent. The brain continues to toggle back and forth between non-REM and REM sleep throughout the night, once every hour and a half.
At the same time, the sleeping brain’s cells shrink, making more room for the brain and spinal cord’s fluid to slosh back and forth between them. “It’s like a dishwasher that keeps flushing through to wash the dirt away,” says Nedergaard. This cleansing also occurs in the brain when we are awake, but it’s reduced by about 15%, since the glial cells have less fluid space to work with when the neurons expand.
This means that when we don’t get enough sleep, the glial cells aren’t as efficient at clearing the brain’s garbage. That may push certain degenerative brain disorders that are typical of later life to appear much earlier.
Both Nedergaard’s and Veasey’s work also hint at why older brains are more prone to developing Alzheimer’s, which is caused by a buildup of amyloid protein that isn’t cleared quickly enough.
“There is much less flow to clear away things in the aging brain,” says Nedergaard. “The garbage system picks up every three weeks instead of every week.” And like any growing pile of trash, the molecular garbage starts to affect nearby healthy cells, interfering with their ability to form and recall memories or plan even the simplest tasks.
The consequences of deprived sleep, says Dr. Mary Carskadon, professor of psychiatry and human behavior at Brown University, are “scary, really scary.”
Rightsizing your sleep
All this isn’t actually so alarming, since there’s a simple fix that can stop this nerve die-off and slow the brain’s accelerated ride toward aging. What’s needed, says Carskadon, is a rebranding of sleep that strips away any hint of its being on the sidelines of our health.
As it is, sleep is so undervalued that getting by on fewer hours has become a badge of honor. Plus, we live in a culture that caters to the late-nighter, from 24-hour grocery stores to online shopping sites that never close. It’s no surprise, then, that more than half of American adults don’t get the recommended seven to nine hours of shut-eye every night.
Whether or not we can catch up on sleep–on the weekend, say–is a hotly debated topic among sleep researchers; the latest evidence suggests that while it isn’t ideal, it might help. When Liu, the UCLA sleep researcher and professor of medicine, brought chronically sleep-restricted people into the lab for a weekend of sleep during which they logged about 10 hours per night, they showed improvements in the ability of insulin to process blood sugar. That suggests that catch-up sleep may undo some but not all of the damage that sleep deprivation causes, which is encouraging given how many adults don’t get the hours they need each night. Still, Liu isn’t ready to endorse the habit of sleeping less and making up for it later. “It’s like telling people you only need to eat healthy during the weekends, but during the week you can eat whatever you like,” he says. “It’s not the right health message.”
Sleeping pills, while helpful for some, are not necessarily a silver bullet either. “A sleeping pill will target one area of the brain, but there’s never going to be a perfect sleeping pill, because you couldn’t really replicate the different chemicals moving in and out of different parts of the brain to go through the different stages of sleep,” says Dr. Nancy Collop, director of the Emory University Sleep Center. Still, for the 4% of Americans who rely on prescription sleep aids, the slumber they get with the help of a pill is better than not sleeping at all or getting interrupted sleep. At this point, it’s not clear whether the brain completes the same crucial housekeeping duties during medicated sleep as it does during natural sleep, and the long-term effects on the brain of relying on sleeping pills aren’t known either.
Making things trickier is the fact that we are unaware of the toll sleep deprivation takes on us. Studies consistently show that people who sleep less than eight hours a night don’t perform as well on concentration and memory tests but report feeling no deficits in their thinking skills. That just perpetuates the tendency to dismiss sleep and its critical role in everything from our mental faculties to our metabolic health.
The ideal is to reset the body’s natural sleep-wake cycle, a matter of training our bodies to sleep similar amounts every night and wake up at roughly the same time each day. An even better way to rediscover our natural cycle is to get as much exposure to natural light as possible during the day, while limiting how much indoor lighting, including from computer and television screens, we see at night. And of course, the best way to accomplish that is by making those seven to nine hours of sleep a must–not a luxury.
“I am now looking at and thinking of sleep as an ‘environmental exposure,'” says Brown University’s Carskadon–which means we should look at sleep similarly to how we view air-pollution exposure, secondhand smoke or toxins in our drinking water. If she and other researchers have their way, checking up on sleep would be a routine part of any physical exam, and doctors would ask about our sleep habits in the same way they query us about diet, stress, exercise, our sex life, our eyesight–you name it. And if we aren’t sleeping enough, they might prescribe a change, just as they would for any other bad health habit.
Some physicians are already taking the initiative, but no prescription works unless we actually take it. If our work schedule cuts into our sleep time, we need to make the sleep we get count by avoiding naps and exercising when we can during the day; feeling tired will get us to fall asleep sooner. If we need help dozing off, gentle exercises or yoga-type stretching can also help. Creating a sleep ritual can make sleep something we look forward to rather than something we feel obligated to do, so we’re more likely to get our allotted time instead of skipping it. A favorite book, a warm bath or other ways to get drowsy might prompt us to actually look forward to unwinding at the end of the day.
Given what scientists are learning about how much the body–and especially the brain–needs a solid and consistent amount of sleep, in-the-know doctors aren’t waiting for more studies to prove what we as a species know intuitively: that cheating ourselves of sleep is depriving us from taking advantage of one of nature’s most powerful drugs.
“We now know that there is a lasting price to pay for sleep loss,” says Veasey. “We used to think that if you don’t sleep enough, you can sleep more and you’ll be fine tomorrow. We now know if you push the system enough, that’s simply not true.”
–WITH REPORTING BY MANDY OAKLANDER AND ALEXANDRA SIFFERLIN/NEW YORK CITY
Read next: 5 Tricks for the Best Nap Ever
More Must-Reads from TIME
- Cybersecurity Experts Are Sounding the Alarm on DOGE
- Meet the 2025 Women of the Year
- The Harsh Truth About Disability Inclusion
- Why Do More Young Adults Have Cancer?
- Colman Domingo Leads With Radical Love
- How to Get Better at Doing Things Alone
- Michelle Zauner Stares Down the Darkness
Contact us at letters@time.com