Time and Mic present
Life After Addiction
After video of their overdose went viral, a couple got a chance at redemption
Story by Alice Park | Photographs by Jeffrey Stockbridge for TIME
The video is hard to watch. A middle-aged man is bent backward over a bus-stop bench, eyes closed, head brushing the ground and a cell phone in his outstretched hand. It rings, but the man doesn’t move. A few feet away, dangerously close to the road, a woman lies facedown on the sidewalk, her legs buckled under her. She tries to get up but can’t make it, and collapses back down in a heap.
The pair are in what’s known as the medical district of Memphis, near a major academic hospital, but people walk by without a second glance. Others take out their phones and start recording. “Look, they on the good gas, man,” says one of the people who streamed the scene to Facebook Live. Another starts an impromptu rap: “Percocet, she pop a Percocet, she on the Xanax.”

The footage quickly went viral and was viewed millions of times.
The man in the video is named Ron Hiers and the woman is his wife Carla. They had just picked up heroin and, too impatient to wait until they got home, walked into the bathroom of a nearby Walgreens and shot up. Then they headed for the bus stop and passed out.
It took a dose of naloxone—a drug that paramedics, emergency medical technicians and even law-enforcement officers have started carrying for the ballooning number of narcotic overdoses they see—to revive Ron and Carla. They were taken to the hospital, and then police took Carla to jail for outstanding charges of petty theft. Ron found his way back home.
“I felt sorry for her,” Ron says in his first extended interview, almost one year after the video was shot. “But I also thought, There’s more for me.” Ron says he injected Carla’s portion of the heroin and then took what was left of his monthly prescription of Xanax pills, about four dozen of them, hoping they would put an end to more than four decades of pain and addiction. They almost did.

“That’s what drugs and alcohol will do to you. It’ll take you places you can’t imagine.”
The video of Ron and Carla’s overdose is part of a grim genre that has emerged alongside the deadliest drug crisis in American history. Every day across the country, nearly 100 people die from overdoses of opioids, powerful narcotic painkillers that attach to cells and dull pain, slow breathing and bring on an overall sense of calm and satisfaction. Since 1999, the rate of fatal prescription opioid overdoses in the U.S. has quadrupled. In 2015, drug overdoses claimed more lives than car accidents and gun violence and rivaled the HIV/AIDS crisis at its peak. The toll, as the White House commission on the crisis put it, is the equivalent of the 9/11 attacks every three weeks.
It is an epidemic without boundaries, touching every corner of the nation, every income group and virtually every age, including a baby born in opioid withdrawal every 25 minutes. In a September study on mortality in the U.S., researchers at the Centers for Disease Control and Prevention (CDC) found that opioids contributed to a decline in the life expectancy of Americans from 2000 to 2015. Indeed, in some parts of the country, bodies pile up so quickly that medical examiners have resorted to storing the overflow in makeshift freezers when their morgues are full. In big cities and small towns alike, police officers are responding to more and more overdose calls, limiting their ability to address other crimes.
Even many firefighters now are expected to use naloxone, and are being called out to revive addicts who overdose so frequently they know them by name.
In response to the growing crisis, President Trump declared a national public-health emergency on Oct. 26, which means federal agencies have 90 days to redirect existing resources to fighting the epidemic. It was a broad call to action, but one that failed to allocate much-needed new funding to address the crisis. The President’s Commission on Combating Drug Addiction and the Opioid Crisis, which issued its final recommendations days after the President’s declaration, also stopped short of providing more dollars for the epidemic, while calling for measures such as tightening regulations on opioid prescriptions, expanding the use of drug courts as an alternative to incarceration and enhancing access to addiction treatments and overdose medications like naloxone.
As the epidemic has worsened, it’s become clear that existing strategies and resources aren’t sufficient. Many states already restrict how much opioids doctors can prescribe, and the Food and Drug Administration (FDA) took the unprecedented step last summer to pull from the market medications for which the addictive dangers outweigh the painkilling benefits. The agency, along with the CDC, is pushing for changes in the way opioids are prescribed, including limiting the number of pills doctors can prescribe at one time and restricting the conditions for which opioids can be dispensed. Pharmacies are also addressing the crisis; CVS announced this fall that it will only reimburse its beneficiaries for seven days of a prescription and will only dispense short-acting opioids and not long-acting versions to first-time users. And last month Walgreens announced it will start selling the overdose-reversal drug Narcan over the counter—a move that can be seen as an acknowledgment of just how widespread the problem has become.
These efforts, however, have had unintended consequences. Restricting access to legal opioids has led to an explosion of illegal substitutes that have similar narcotic effects. Drugs such as heroin, fentanyl, carfentanil and U-47700 are cheaper and in many cases more harmful than legal opioids because they are synthetic formulations with no FDA standards for safety and quality control.
From 2002 to 2015, deaths from heroin overdose increased more than sixfold, and in 2016, the Drug Enforcement Administration (DEA) reported more than 30,000 seizures of fentanyl, a dramatic spike from the 5,000 documented in 2014. The man-made formulas are so powerful that police officers participating in drug raids where fentanyl is confiscated have overdosed simply by breathing in particles of the drug released into the air. The opioid epidemic may have been sparked by prescription medications, but it’s now as much a label for a much larger addiction crisis in the U.S., spanning dozens of drugs both legal and not.
The toll has been evident in Memphis, where Ron and Carla overdosed on that sunny fall day. Between 2010 and 2015, deaths from drug overdoses increased by 40%. But statistics can seem like abstractions, numbers to be glossed over rather than felt as actual loss.
Understanding how this crisis is upending lives, devastating families and changing communities requires hearing the stories of those with the most at stake. On Oct. 3, 2016, Ron and Carla Hiers became an official part of the grim record, their overdoses added to the several hundred tallied in the city that year, and to the tens of thousands documented for the country. “That’s what drugs and alcohol will do to you,” says Ron. “It’ll take you places you can’t imagine.”
This is their story.
“I can’t say that I really ever thought that I had a drug problem.”
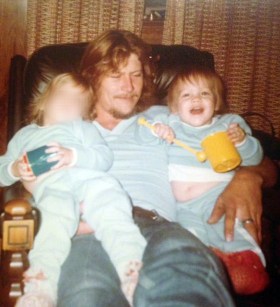
Ron Hiers was born in Memphis in 1955 with a cleft palate. Surgery corrected the birth defect, but left him with a nasal twang that became a target of his classmates’ ridicule. He says he was bullied throughout school and had a knack for finding trouble. He was expelled from high school after a series of incidents, including threatening a teacher, and began drifting across the South, working construction to stay afloat.

After he fell during a construction job and broke his heel, prescriptions for opioids like the pain reliever oxycodone became relatively easy to come by. Even after the bone had healed, Ron found a way to make it seem like the pain had returned—over and over again. “They can take an X-ray but they don’t know whether it bothers you or not, so I could always keep the pain meds going,” he says.
When Ron couldn’t get his hands on opioids, he turned to heroin, which had the same narcotic effect and was less expensive and often less of a hassle to obtain. “It was about as easy [to find] drugs as finding your shoe to put on in the morning,” he says.
It was during a visit back home in Memphis, after Ron called one of his regular dealers to supply drugs for a party, that he met his wife Carla. They quickly bonded over their shared addiction. “I don’t remember [Ron proposing] because I was always medicated,” Carla, 61, says today, more than 20 years after they first met.
Like Ron, Carla says she began using drugs in high school, mostly to fit in, and found she loved the way opioids made her feel. “It’s a euphoric high, everything is O.K. with the world, and you just feel great,” she says. “But as the years went on, the using got more intense, and it got to the point where I had to keep [using] because I was addicted to it, and if I didn’t use, I would get sick.”
Addiction is at its essence a hijacking. Parts of the brain that are dedicated to rewarding behavior and triggering feelings of satisfaction and calm are kidnapped by opioid drugs to induce a temporary state of ease and even euphoria. “The impulsive, reward-driven system of the brain goes into overdrive,” says Dr. Sarah Wakeman, director of the substance-use disorder initiative at Massachusetts General Hospital.
Opioids are particularly adept at such snatching and seizing. The body has its own SWAT team that swoops in when pain erupts: receptors on nearly every cell in the body are primed to sound the alarm when you, say, put your hand on a hot stove or stub your toe. Opioid receptors populate cells not just in the body, but in the brain and spinal cord as well. Their job is to tone down the firing pain signals—the fast breathing, the feeling of panic and the excruciating feeling of ouch!—as quickly as possible. Opioid drugs target these receptors and magnify the body’s natural painkilling response. For people with long-term, chronic pain, that can be essential to getting through the day. But the receptors are also intimately networked with the pleasure and reward areas of the brain. They are supposed to counteract the unpleasant feeling of pain with the opposite sensation. The catch is that for people already at risk for addiction, once the brain and body get a taste of the pleasure override, they want more.
Neurologists now know that drugs like opioids can change the brain in people who develop addiction. Once the opioid receptors are activated in these vulnerable brains, they stay activated, becoming the brain’s bully, demanding all of the energy and all of the attention. The reward-oriented brain, the regions responsible for impulses and emotions, take precedence over the thinking parts that evaluate things like risk, benefit, consequences and delayed gratification.
And because opioids can release more dopamine, the feel-good sensations triggered by the drug overpower any positive feelings from things like food, love and even sex. “Opioids causes a higher rush of dopamine to the brain that cues the mind to pay attention to that,” says Wakeman.
That’s how opioid drugs become so addictive; they suppress pain with impressive efficiency, but they also prime neurons to seek and stay in that state of pain-free bliss. “It takes you to a state of nirvana,” says Ron. “I can describe it best by saying that if you and your wife are in a house and your wife runs in the room and says, ‘I just ran over the dog,’ your response is ‘We’ll get another one.’ Nothing matters. Absolutely nothing. There’s nothing you can say to me that can get me upset or alarmed. It buries your feelings so deep.” In pursuit of that feeling, Ron and Carla took to forging prescriptions. They described their routine as if it were scripted: the pair would visit a hospital and Ron would pose as the patient, signing in with a made up name and Social Security number, and spin a yarn about a toothache. He asked for antibiotics, not painkillers. “That would throw the doctor on easy street, because I’m not in there asking for something for pain, like he generally hears,” says Ron.
Eventually, a sympathetic doctor would ask if he were also in pain, and prescribe an opioid. It didn’t matter which drug he prescribed, or how many pills. What Ron and Carla really wanted was his DEA number, which is required for filling any prescription medication. While Ron was seeing the doctor, Carla would scope the nurses’ station for the other critical part of their scheme: unattended prescription pads.

Carla got pregnant in 1995, and the couple used the doctor’s visits as a way to fuel their addiction. While in the hospital, the Hiers managed to steal more prescription pads, before urine and blood tests revealed Carla’s opioid abuse.
The hospital called Child Protective Services, but their daughter was born with a congenital heart defect that required her to be airlifted to a specialized children’s hospital. After a court case, they say they ultimately gave up custody to a family that adopted their daughter as an infant.
Even being deemed incapable of keeping their child wasn’t enough to jolt Ron and Carla to sobriety. “I can’t say that I really ever thought that I had a drug problem,” says Ron. “Your addiction don’t let you think like that. Your addiction wants you to think that, Man, this is fine. You’re doing O.K. This is normal; this is the way to live life. You’re not doing nothing wrong.”
Ron had three children before he married Carla, and while he has reached out to all of them since he became sober, not all of them have welcomed him into their lives. He says that the daughter he had with Carla does not want a relationship with him. And he doesn’t blame her. He recalls coming home with his first child to a ransacked house and a warrant stuck to the door for drug possession. When his second child was born, he says he left his wife while she was in labor to visit a strip club across the street from the hospital. He wasn’t even aware he had a third child until a teenaged boy called him and told him he was his son and asked to meet. Ron says he gave his son Xanax before sending him back home.
“No decisions that you make on drugs or alcohol are right, none.”
Paris Hardee was one of the millions of people who watched the video of Ron and Carla’s overdose. It was her birthday, and she was on her way to a celebratory dinner when a relative called to say that her father had been on the news. She Googled the video and saw Ron sprawled across the bus stop. Paris wasn’t surprised by what she saw. “I made fun of him like everybody else,” she says. “I was like, ‘There’s Ron’s 15 minutes of fame.’”
Paris, 35, is Ron’s second child with his first wife. She was raised by Ron’s parents when he proved too unreliable. She only remembers her father when he was high, always asking her and his parents for money.
When she was around 8, Paris says Ron was arrested in front of her and her friends. “We lost all of our friends,” she says. “Nobody’s parents would let us play with them after that and we had to move. That’s really hard when you’re in the third grade. I lost every friend I had, but I still thought he was a good guy.”
Ron’s parents worked hard to maintain their granddaughter’s perception. They bought and wrapped birthday and Christmas presents for Paris and her sister in their father’s name, and never openly discussed his problems. Still, Paris couldn’t help but worry about her dad, particularly when he called her from jail. “I was scared for him,” she says. “I thought somebody would beat him up, and when I went to bed, I would worry about him a lot.”
For a while Paris tried to help. She wrote motivational notes on pieces of paper that she would stick in his wallet, hoping they would remind him to not drink.
“It was like, ‘Dad you can do it. I love you, and you’re strong.’ Just these little pieces of paper that I wanted him to pull out and read,” she says.
Her father repaid her by stealing the birthday money and allowance she got from his parents. “He was always going to choose drugs over health, over family, over friendships,” Paris says. “He was going to choose drugs no matter what.”

Paris cut off contact with her father, keeping him out of her life for 13 years, including her college graduation and her wedding. She started referring to him as Ron rather than Dad.
That changed once she saw the overdose video. She couldn’t shake the image of her father splayed across the bench, limp and unconscious. After pushing him out of her mind for more than a decade, she now couldn’t stop thinking about the father who had never really been one.
The clip that had aired on the local news contained the number for Addiction Campuses, a for-profit drug-addiction recovery company with four locations around the country. Paris dialed. “I was crying and I said to whoever answered, ‘The man who OD’d in Memphis—that’s my dad.’”
“Addicts can say anything, addicts are great actors, you know.”
On the other end of the line, the dispatcher for Addiction Campuses called Stacy Dodd, director of operations for their facility just over the Tennessee border in Mississippi. A former addict, Dodd saw an opportunity to help Ron and help the center. He offered to bring Ron in for a 30-day treatment program and waive the typical fee, which can run up to $25,000.
Ron may have been at rock bottom, but he wasn’t yet ready to look up. Several months before his overdose, Ron was diagnosed with tonsillar cancer. He says he continued to get high during his chemotherapy treatments, which he completed in July 2016, according to his medical records, snorting before and after his appointments.
On the first day of every month, Ron filled a prescription for Xanax that his doctor had written to help with his anxiety. There were nearly four dozen pills left in the bottle, and, he says, on Oct. 3, 2016, after being revived from the overdose that millions witnessed online, he took them all.
“I’d like to have died from the cancer,” Ron says. “I was tired. I was sick of living. I got tired of waking up. I got tired of putting my shoes on. I got tired of reaching for my syringe. I got tired of going and getting money for dope, and I knew I just couldn’t live without dope.” It wasn’t a new feeling for Ron. In his wallet, he carried a weathered scrap of paper on which he had scrawled his own obituary. He left the date of his death blank.
Like many recovery and rehabilitation facilities, Turning Point, an Addiction Campuses facility, relies on a combination of medications and behavior therapy to help people overcome their addiction. Medication-assisted treatment, or MAT, involves using another opioid, such as buprenorphine, to gradually withdraw an opioid addict from his dependence on the drugs. Unlike methadone, which is also used to treat opioid addiction, physicians can prescribe it without the need for a rigid clinical program for monitoring the recovering addict. It’s less likely to trigger the addiction and reward cycles that morphine and opioid drugs do, but its use is controversial. Law-enforcement officers in particular have been skeptical of buprenorphine’s usefulness, worrying that it amounts to replacing one drug for another in an addict’s downward spiral.
Many doctors, on the other hand, see MAT as an essential part of stopping the addiction cycle, a way to break the brain’s relentless search for more opioids. “The goal of medication is to relieve that mental obsession, the feelings of craving,” says Wakeman, who believes MAT is the best way to help addicts on the road to sobriety. “We need to get people stabilized, and restore their brain to normal function so they are able to think normally.”
When Ron woke up on his first morning at the center, he wasn’t sold on the idea of recovery. “My first thought was to get out of this damn place, and get on back to that boardinghouse,” he says. But when the elevator doors opened in the lobby, he saw that the center was coed. “I’m not trying to be funny. That’s what my mind actually thought: there were good-looking girls there, so I was not leaving.”
However shallow his reason for staying, Ron did. One day turned into two, and eventually he completed the 30-day program. The therapy included learning skills to help him and his fellow addicts divert their urge to act out of emotion, which often leads to reckless and compulsive behavior like drug use that ends up with their harming themselves or others, and instead to adopt skills to control and turn those emotions and urges into positive reactions rather than negative ones.
After a few weeks in jail, Carla was released and called Paris, looking for Ron. Paris told her he was in a recovery program, and Carla, too, reached out and was offered a similar arrangement as Ron, but at the company’s facility in Massachusetts. Because they had used together, the center thought they needed to recover separately. “I had to relearn my thinking, I had to relearn my dealings with people and to listen to people,” Carla says of entering treatment.
Undoing decades of addiction is an ongoing process. For the first few weeks at the center, Ron was telling the counselors what he thought they wanted to hear. “Addicts can say anything, addicts are great actors, you know,” he says.
Across the country, opioid rehabilitation has become a big business—claiming a larger chunk of the $35 billion drug-addiction treatment industry every year.
Recovery facilities typically provide 30-day programs, since that’s what insurance plans tend to cover. It’s enough time to wash the drugs out of the addicts’ system, but often not enough to arm them with the deeper skills they need to confront the forces that drove them to use in the first place. Relapse rates are high—addiction doctors say nearly every addict who enters treatment can expect to relapse.
Some recovery programs exacerbate the problem by treating addiction as an acute problem that can be solved with a one-time solution, rather than an ongoing disease. A rise in such programs has led the FBI to investigate centers that defraud addicts and their insurers, allegedly billing for services that aren’t always effective and can set off a cycle of expensive recovery and relapse.

What recovery facilities do provide, however, is a forced period during which opioids are flushed out of the body, and for some, that’s enough to expose some hard truths. It was for Ron. After nearly a month of sober living, Ron says he woke up one morning and asked himself two questions: Are you honestly happy? Do you want to kill yourself? “I couldn’t answer the first with a yes, because I had an obituary in my freakin’ wallet,” he says. “But I also realized I honestly no longer wanted to kill myself.”
That marked a change for Ron. That’s when the skills the counselors were trying to teach him, and the perspective they were hoping he would gain about his life and his relationships, became more than an exercise to fill up the day. Gradually, Ron began to see his life for what it was—a squandered opportunity, a collection of people he hurt and abandoned, a series of delusions. “We’re scared to death of being found out,” he says of clinging to drugs. “I was most afraid of finding out who I was because I never knew. I was scared to find out. I was scared to find out that I was probably not as tough as I thought I was. I was probably not as handsome as I thought I was. I was probably not as well-liked as I thought I was. I was scared to discover the truth about me.”
After a month in treatment, Ron’s first phone call came from Paris. She begged him to stay longer, to continue working on his recovery. She knew that 48 years of addiction couldn’t be wiped away in a month, so she made him promise to stay.
He promised. It was the first promise he made to anyone that he kept in a long, long time.
“I wouldn’t trade any day of recovery that I’ve had for a day of addiction.”
Ron still has that cell phone that rings in the video. He still has the numbers of his “dope boys,” the dealers who, with a push of a button, would send him right back to the drug-fueled nirvana that sustained him for nearly half a century. He also has a new cell phone, with new contacts for people who have reached out since he’s been in recovery. But he keeps that old phone and its numbers as a reminder. “I don’t never want to forget where I came from,” he says. “If I forget that, I could go back.”
After more than a month at the recovery center, Ron moved into a halfway house. He now shares an apartment with people he met during recovery. There, his new talisman—replacing the 40 oz. bottle of beer that he says was “part of my outfit” for decades—is a blue Alcoholics Anonymous book, filled with his notes in the margins.
Paris, whose phone call may well have saved her father’s life, has gradually let him back into her world and introduced him to his grandchildren. Not long ago, Ron texted Paris at 2 a.m., seized with regret. “I just now wept with sorrow having finally realized how much I wouldev [sic] enjoyed loving my children their entire life [sic],” he wrote. He didn’t expect an answer, but the next morning, Paris replied. “Don’t cry, Dad. I was really awkward until about 27. You didn’t miss much. I love you so so much.”
She is cautious, however, since he has been high for nearly 50 years and sober for just one. “I am part of his support system but I have boundaries and I have to maintain those boundaries for my self,” Paris says.
Ron still considers getting high every once in a while. But now his thinking brain takes over and quells the urge that rises from the deeper, baser brain that is ruled by the mission to feel good at all costs. And that, say addiction experts, is how recovery starts. For all the ways opioids can rewire the brain, it can be reversed when the hijacked pleasure networks are freed from the onslaught of drugs.
Close to the first anniversary of Ron’s sobriety, Paris is amazed by his transformation. “I have my father back,” she says in a text message. “It is true that my childhood was rough but now I’m blessed with a father who is growing and changing every day. Someone who did not know how to show love to himself or others is now, through God’s grace, experiencing and giving love for the first time. That’s a miracle!!”
Carla, too, lives on her own, but in an apartment in Massachusetts far from her old haunts. Raised as a Southern Baptist, Carla rediscovered her faith and says she’s committed to building a new life. She continues to go to meetings and shares her story of recovery with others who are struggling with addiction. “I don’t want to go back to Memphis. A lot of bad memories, a lot of bad things happened there,” she says. Ron and Carla talk on the phone and over social media, but they haven’t seen each other since their overdose. Both say they realize they are different people now, and that the things that bound them together before are no longer a part of their lives.
Ron is hoping to become a recovery counselor, helping people like himself by his example. “Life shouldn’t be taken lightly,” he says. “It’s a gracious gift meant to enjoy and not be squandered. I’ve come to the realization that I’ve wasted mine—you only get one, and I wasted it.” It’s a hard-won lesson, but one that is helping him to make the most of whatever life he has left. “I wouldn’t trade any day of recovery that I’ve had for a day of addiction since I’ve sobered up,” he says. “The best thing I have now is peace.” —With reporting by Paul Moakley/Memphis •
