![]()
With her long dark hair flying, Saorla Meenagh, 10, (pictured above) can execute a perfect switch leap, one leg out, one tucked under, her arms glued to her sides in classic Irish step-dancing style. Saorla, whose blue eyes, white skin, and sprinkle of freckles helped win her a modeling contract with a New York agency—on hold until her braces come off —also plays softball and Gaelic football, a soccer-like game her father, Seamus, a contractor, enjoyed when he was growing up in County Tyrone, Northern Ireland.
When asked her position on the team, Saorla wiggles in her seat at the family’s dining room table. “I don’t know—random positions,” she says, as her mother, Kerri, a pediatric nurse practitioner quietly pushes her daughter’s bare foot off the table where it has wandered for what may be the 10th time in half an hour. During that time, Saorla’s actions are as scattered as pool balls in a break. She sits on her knees, then jiggles, then rocks, then circles photos in a stack of food magazines with a pen, turning off the TV, turning up the TV, turning down the TV, and making part of a bracelet on a Rainbow Loom before she finally loses interest. She rarely finishes a task and being with her can be as disconcerting as watching television with someone pressing the channel changer every 10 seconds.
 Along with a gift for math and a love for Gaelic sports, Saorla has inherited something else from her father: attention deficit hyperactivity disorder, ADHD. People just meeting her find her adorably sweet, if quirky. But if she’s not on her medication—which she isn’t at the moment because we met at her family’s home in a Philadelphia suburb during the summer—she is an exhausting ball of boundless energy. (While she’s not at school, her mother gives her a medication holiday in order to boost her appetite, help her gain weight and grow, all things Vyvance interferes with.) “When we had her tested they said that in 20 years she was the most hyperactive child they ever tested,” says Meenagh, gently removing that errant foot from the table yet again.
Along with a gift for math and a love for Gaelic sports, Saorla has inherited something else from her father: attention deficit hyperactivity disorder, ADHD. People just meeting her find her adorably sweet, if quirky. But if she’s not on her medication—which she isn’t at the moment because we met at her family’s home in a Philadelphia suburb during the summer—she is an exhausting ball of boundless energy. (While she’s not at school, her mother gives her a medication holiday in order to boost her appetite, help her gain weight and grow, all things Vyvance interferes with.) “When we had her tested they said that in 20 years she was the most hyperactive child they ever tested,” says Meenagh, gently removing that errant foot from the table yet again.
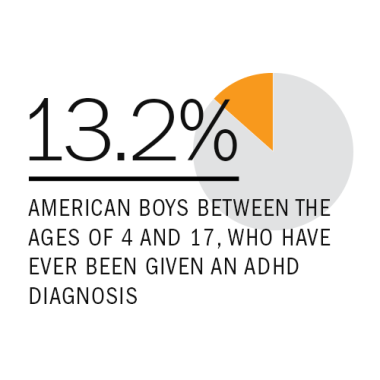
But Saorla’s perpetual motion isn’t what concerns Meenagh the most. Being fidgety and easily distracted are two of the most common and recognized symptoms of ADHD, often leading to poor performance in school, the most recognized fallout of the condition. But the 5% to 11% of American children 4 to 17 years of age who are diagnosed with the disorder—the numbers are up for debate depending on whom you talk to—also face a lifetime of increased risk for accidents, teen pregnancy, drug and alcohol abuse, smoking, and even dying prematurely. Overall, boys (13.2%) are more likely than girls (5.6%) to be given an ADHD diagnosis.
It’s the fear for her child’s future that makes Meenagh bristle when she hears someone—family, friends, strangers, even scientists—say that ADHD doesn’t exist, that the symptoms are caused by poor parenting, food additives, or 21st century life in the fast lane, lack of physical activity, or that they’re just kids being kids, albeit less manageable than most. “A lot of people don’t believe in it,” she says. “I think that’s because they’ve never experienced it firsthand.”
To those naysayers, C. Keith Connors, professor emeritus of medical psychology at Duke University and creator of the Connors Rating Scales for diagnosing ADHD, says he always offers the same challenge: “Take one of these kids on a car trip for a day and see how you feel about it then.”

It’s easy to see why some dismiss ADHD as simply an artifact of modern life. After all, we’re all on the information Autobahn. Most Americans are exposed to an average of 100,000 words a day—about the length of Mark Twain’s The Adventures of Huckleberry Finn—very little of which we’re able to absorb, according to a 2009 study on America’s information consumption from the University of California, San Diego. We’re also asked from a very young age to be still, nearly motionless, except for the tapping of our fingers on the computer keys. Ours is not a society tolerant of perpetual motion or daydreaming. At some point, we’re all like the dog in the Pixar movie, Up, doing one thing and then responding to the real-life equivalent of “Squirrel!”
But ADHD isn’t a disorder of the modern age. It may have been first described in the medical literature in 1763 by Scottish physician Sir Arthur Crichton, who observed patients so unable to focus that “the barking of dogs, an ill-tuned organ, or the scolding of women, are sufficient to distract patients of this description to such a degree, as almost approaches to the nature of delirium.” Those patients, he noted, referred to their own symptoms, including anger “bordering on insanity,” as “the fidgets.”
The argument doesn’t hold up either when ADHD’s worldwide prevalence is factored in. It’s found in developing countries, where the information speed limit is slower and the requirement to be sedentary 24/7 doesn’t exist.
 Yet there’s an undeniable backlash against the diagnosis. Earlier this year, Chicago neurologist and ADHD specialist Dr. Richard Saul published a provocatively titled book, ADHD Does Not Exist, in which he proposes that ADHD is not an entity in itself but a cluster of symptoms that stem from more than 20 other conditions, including depression, anxiety, bi-polar disorder, and obsessive-compulsive disorder. Many of those, along with dysfunctional behavior conditions such as oppositional defiant disorder, characterized by aggression, tantrums and a propensity to argue with adults, and learning disabilities such as dyslexia, are often diagnosed as co-illnesses with ADHD. Saul criticizes the catchall-nature of an ADHD diagnosis, which he believes corrals a lot of real conditions into one.
Yet there’s an undeniable backlash against the diagnosis. Earlier this year, Chicago neurologist and ADHD specialist Dr. Richard Saul published a provocatively titled book, ADHD Does Not Exist, in which he proposes that ADHD is not an entity in itself but a cluster of symptoms that stem from more than 20 other conditions, including depression, anxiety, bi-polar disorder, and obsessive-compulsive disorder. Many of those, along with dysfunctional behavior conditions such as oppositional defiant disorder, characterized by aggression, tantrums and a propensity to argue with adults, and learning disabilities such as dyslexia, are often diagnosed as co-illnesses with ADHD. Saul criticizes the catchall-nature of an ADHD diagnosis, which he believes corrals a lot of real conditions into one.
Saul’s theories hit home with a lot of people who are worried about statistics showing an increase in the number of ADHD diagnoses in the U.S. and the number of prescriptions filled every year for relatively powerful stimulant drugs such as Ritalin, Adderall and a host of new medications. Though these drugs are generally considered safe, they do have side effects, including anxiety—sometimes even paranoia—weight loss, insomnia, and growth retardation (about half an inch, which doesn’t appear to be permanent). In some rare cases they can damage the heart. Since many of the drugs are appetite killers, some parents have to entice their children with small meals all day long. The side effects are why many children like Saorla take medication holidays during summer months or even on the weekends. They’re also why doctors and parents have to carefully weigh whether the problems a child has if he or she goes unmedicated are worth the risk.
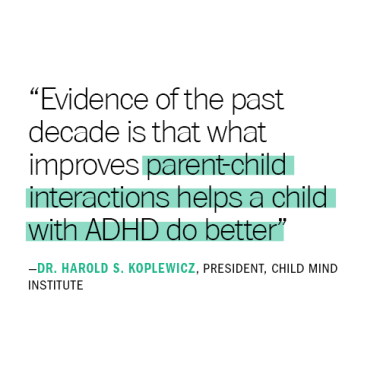
How prevalent has an ADHD diagnosis become? A survey of 76,000 parents conducted by the Centers for Disease Control (CDC) every four years estimates that one in 11 children had been diagnosed with ADHD by a health care professional, an increase of 42% between 2003 and 2014. “[That number] is preposterous,” says Connors, who studied and treated ADHD for 50 years before retiring. “That would make it an epidemic.” (See a map of ADHD prescriptions in the U.S.: What’s With ADHD in the South)
One possible explanation for the frequency of the diagnosis is that the data collection method is imperfect. The National Survey of Children’s Health is a phone survey and the figures on ADHD are collected on the basis of the answers to one question: “Has a doctor or other health care provider ever told you that [your child] had attention deficit disorder or attention-deficit/ hyperactivity disorder, that is, ADD or ADHD?” The type of “other health care provider” isn’t established. ADHD experts say it is often a pediatrician who does not spend the kind of time it takes to make an accurate diagnosis. The gold standard of ADHD diagnosis is an analysis of questionnaires, like those Connors developed, filled out by parents, teachers and other people who interact with the child and observe classroom behavior. Each child can take hours to analyze.
“That’s a luxury a pediatrician doesn’t have,” says Dr. Harold S. Koplewicz, MD, who founded the NYU Study Center and is founding president of the nonprofit Child Mind Institute in New York City. ‘They get seven minutes face to face, [the doctor gives] them a prescription, and then 30 days later they come back to get it renewed.”
(The CDC, however, defends its figures. They say the numbers from their parent survey hold up when they’re compared to their own separate, more scientific study looking at insurance claims and field assessments. In this case, scientists in the field do a full 2.5-hour diagnostic evaluation of students for ADHD and other conduct and mental health disorders in 10,000 schools across the country, says epidemiologist Susanna Visser of the CDC’s National Center on Birth Defects and Developmental Disabilities. “We come up with a similar estimate—8.5 to 10%,” she says.)
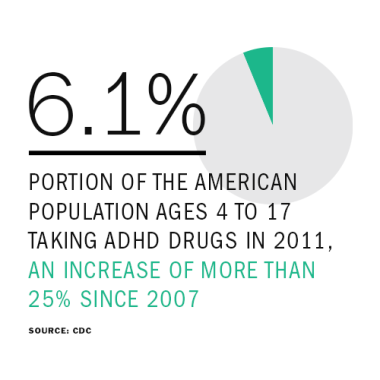
And the drug stats aren’t in question. The percentage of children taking drugs jumped by more than a quarter, from 4.8% of the population between 4 and 17 to 6.1% between 2007 and 2011 according to the CDC’s survey. In fall 2011 and spring 2012, there was even a brief shortage of ADHD drugs, particularly generics, because the demand was outpacing the supply.
 Along with quickie diagnoses in a pediatrician’s office, part of the problem seems to stem from a misunderstanding of ADHD symptoms and the methods used to diagnose the disorder. The diagnosis is based on a checklist, found in the “bible” of mental health, the Diagnostic and Statistical Manual of Mental Disorders (DSM-V), of 18 possible symptoms, any of which could describe the average child—even the average adult—some of the time. They include acting before thinking, being unable to delay gratification, staying motived to finish a boring task, keeping strong emotions in check, remembering an assignment and how to complete it, or planning ahead.
Along with quickie diagnoses in a pediatrician’s office, part of the problem seems to stem from a misunderstanding of ADHD symptoms and the methods used to diagnose the disorder. The diagnosis is based on a checklist, found in the “bible” of mental health, the Diagnostic and Statistical Manual of Mental Disorders (DSM-V), of 18 possible symptoms, any of which could describe the average child—even the average adult—some of the time. They include acting before thinking, being unable to delay gratification, staying motived to finish a boring task, keeping strong emotions in check, remembering an assignment and how to complete it, or planning ahead.
But three other factors play a pivotal role in determining whether a child has a disorder or is just quirky, inattentive, or high-spirited. To be diagnosed with ADHD, children must have most of those 18 symptoms, most of the time, in most areas of their lives, from home to school to the neighborhood playground.
“And, most important, there must be impairment,” says leading ADHD expert Russell Barkley, PhD, clinical professor of psychiatry and pediatrics at the Medical University of South Carolina in Charleston. “They must be unable to function as well as others—and in fact, are often well below normal—in any of those domains.”

Fourteen-year-old Zoe Williams “is just a fireball,” says her mother, Monnica Williams, a Louisville, Kentucky, psychologist who has five children, three of whom have been diagnosed with ADHD. “She’s the kid in the middle of the dance floor that all the other kids are watching, And she talks and talks and talks. Sometimes I have to say, ‘Zoe, it’s not that I don’t want to hear what you have to say, but Mom needs a little talking timeout.’”
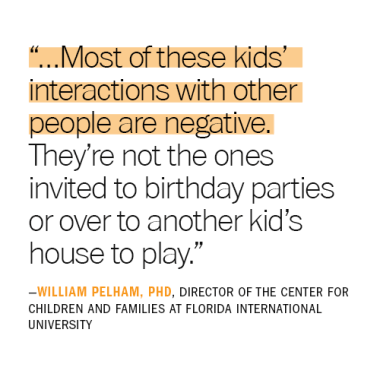
While kids with ADHD can be gregarious, their impulsiveness can create problems, often alienating others, including siblings, teachers, and classmates. They don’t wait their turn, interrupt others, are easily frustrated, take wild risks, and their emotions can spill over like water at a rolling boil: They may be hot-headed, lash out violently, or have temper tantrums. All of this carries enormous social cost in school and on the playground.
Like autism, ADHD symptoms fall along a spectrum from mild to severe, so it’s difficult to define what’s typical. But, in general, for a child with attention deficits, trying to focus on one thing is akin to trying to discern the chirping of crickets in Times Square. They’re forgetful, tend to procrastinate, and are disorganized. They have a hard time putting in the time and effort to achieve a goal, particularly if it’s something like finishing a school project on a topic that doesn’t interest them. (Paradoxically, they can also hyperfocus at times, confusing parents who can’t understand why a child who can reach the 60th level of World of Warcraft can’t remember homework assignments or follow a simple set of instructions.)
Some are chronically late. “People with ADHD are blind to the future, which is why they never have anything done on time,” says Barkley. “If you have an ADHD practice, a third of your patients are late or never show.” (Those practices usually include adults; most ADHD symptoms persist into adulthood, though they may be milder.)
ADHD is divided into subtypes—children just with attention problems, those with impulse control and hyperactivity issues, and a group with a combination of the two. The latter is the most common, occurring in two-thirds to three-quarters of people, estimates Barkley.
Children with attention problems can have any or all of these symptoms, but may not be any more fidgety than the average child. Sometimes they’re labeled merely ADD. On the other hand, children who are hyperactive as well as distractible may not be able to stop moving or even to stop talking, including to themselves. An internal conversation for most people can become a conference call on speakerphone for a child with ADHD.
So it’s no surprise that the average ADHD-afflicted child has one to two negative interactions per minute with the people in their lives, says William Pelham, director of the Center for Children and Families at Florida International University who has authored or co-authored more than 300 papers on ADHD. “What that means is that most of these kids’ interactions with other people are negative. They’re not the ones invited to birthday parties or over to another kid’s house to play.”
 That kind of rejection can be damaging to a child’s self-esteem and heartbreaking for parents. “Saorla is such a good kid, such an empathetic kid, but if she’s tired, she becomes ‘Hurricane Saorla,’” says Meenagh. The minute Saorla learned to walk she climbed—everything, and not skillfully. She was impulsive, fearless and, probably as a result, accident-prone. The Meenaghs once had to call the police and fire department to get Saorla, then a toddler, out of a bathroom where she had barricaded herself behind a locked door and a drawer she pulled out.
That kind of rejection can be damaging to a child’s self-esteem and heartbreaking for parents. “Saorla is such a good kid, such an empathetic kid, but if she’s tired, she becomes ‘Hurricane Saorla,’” says Meenagh. The minute Saorla learned to walk she climbed—everything, and not skillfully. She was impulsive, fearless and, probably as a result, accident-prone. The Meenaghs once had to call the police and fire department to get Saorla, then a toddler, out of a bathroom where she had barricaded herself behind a locked door and a drawer she pulled out.
During a class visit to the zoo, Saorla, who has trouble transitioning from one activity to another, balked at moving from one exhibit with the rest of the children and threw a classic “big blowout” tantrum—kicking and screaming—while her mother hauled her away. It’s not unusual, says Meenagh, for those outbursts to go on for an hour.
“I was very aware that everyone was looking at us,” she says. “I was mortified, but mainly I was scared that she was going to be labeled by the other parents as a kid other kids shouldn’t be friends with.”
Saorla does have friends, Meenagh is quick to note, but they’re not her 10-year-old classmates at the local K-8 Catholic parochial school she attends. “She operates more at a seven-year-old level so her friends tend to be younger,” says Meenagh. “She can be very silly—silly to the point that her classmates say she’s too silly for them.”
As much as Meenagh frets over her child’s feelings now, she worries even more about Saorla’s future. “I’ve read a lot about teenage girls with ADHD, how they don’t fit in socially, how they have four to five times the rate of teen pregnancy and are four to five times more likely to be in car accidents. I worry about how this is going to play out.”
Meenagh’s fears are well-founded, says Barkley, author of Taking Charge of ADHD and several other books on raising difficult children and teens. “This is a very serious disorder.” He rattles off a catalog of scary statistics: “As adults, people with ADHD are five times more likely to speed and three times more likely to have their licenses revoked than other people. They’re more likely to experience accidental injuries—burns, poisoning, traffic accidents, all kinds of trauma—than other people. In fact, having ADHD makes you three times more likely to be dead by the age of 45.”
Barkley is aware that he sounds alarmist, but he has good reason. ADHD struck close to home, and with tragic consequences. “I lost my twin brother, Ron, to it,” he says. His brother was killed in a one-car accident after drinking. He was not wearing a seatbelt. “This isn’t just professional for me, it’s personal.”
To say that ADHD is sometimes misdiagnosed—even over-diagnosed—is likely true, say many experts. But to say that it doesn’t exist, as some critics claim, is “like saying the world is flat,” says Edward Hallowell, a psychiatrist who treats ADHD at The Hallowell Centers in Cambridge, MA, and New York City and who has ADHD himself. “Those days are over. Today we have brain scans, genetic studies, twin studies that show that this is a highly inherited neurobiological disorder, not some made-up condition.” Most of the doctors who treat people with ADHD agree that of course the condition exists, even if others like Richard Saul dispute it.
Sophisticated neuroimaging technology has allowed us to see what Crichton’s 18th century patients called “the fidgets” in the brain. Today, scientists believe most ADHD can be traced to a malfunction that develops in brain circuitry that controls what is broadly known as “executive functions” like planning, inhibition, and self-control. This master control board is located in the prefrontal cortex, the forward of the brain just below the forehead, and in the basal ganglia, the clusters of nerve cells found far deeper in the brain’s gray matter.
Those regions work like the brain’s filter; they regulate, among other things, impulse control, attention, the ability to resist distractions, rein in the emotions, think before acting, awareness of time, motivation and motion. If the filter is too porous, too many stimuli get through. “The way I describe it is that it’s like having a Ferrari engine for a brain, but with bicycle brakes,” says Hallowell.
Scans show that those brain regions in children with ADHD are smaller than they are in children in the general population. In one 2007 study done jointly by the Child Psychiatry Branch of the National Institute of Mental Health and McGill University in Montreal, brain scans of 223 children with ADHD showed that the thickening of cortical tissue was delayed by about three years compared to scans of a control group of equal numbers of normally developing youngsters. Size doesn’t matter when it comes to intelligence—many children, like Saorla, have above average IQs—though it clearly has a major impact on behavior.
The ultimate source of these brain differences is likely genes—perhaps thousands of them. The heritability of ADHD is striking. Studies have found that children who have one parent with ADHD have up to a 50% chance of also having it and siblings are between five to seven times more likely to share it. (Saorla’s older sister, Aisling, 12, beat those odds.) A large, British twin study, found that the heritability of ADHD approaches 80%. That means that 80% of the time, ADHD is an inherited (not an environmentally caused) condition, making it slightly less heritable than autism, around 90%, but about as genetically programmed as height.
“There are anywhere from 25 to 45 genes that are considered high-candidate genes for ADHD,” says Barkley. “But there are several we’re reliably sure of, and some of those are the genes related to dopamine regulation in the brain.”
 Dopamine is the brain’s chemical messenger that is probably best known for its role in addiction to drugs, alcohol, sex, even, arguably, chocolate. But this chemical that carries information between nerve cells plays a far more important function in human life than providing us with a cocaine or cupcake high. It uses reward—the pleasurable feelings it supplies—to motivate us to pay attention, avoid distraction, to pick out the most relevant information circulating in short-term memory when solving a problem or completing a task. It also governs motion. The uncontrollable tremors in Parkinson’s patients, for example, are caused by lack of dopamine. Without dopamine, we might starve to death: It’s what motivates us to eat.
Dopamine is the brain’s chemical messenger that is probably best known for its role in addiction to drugs, alcohol, sex, even, arguably, chocolate. But this chemical that carries information between nerve cells plays a far more important function in human life than providing us with a cocaine or cupcake high. It uses reward—the pleasurable feelings it supplies—to motivate us to pay attention, avoid distraction, to pick out the most relevant information circulating in short-term memory when solving a problem or completing a task. It also governs motion. The uncontrollable tremors in Parkinson’s patients, for example, are caused by lack of dopamine. Without dopamine, we might starve to death: It’s what motivates us to eat.
There are dopamine receptors on certain neurons (nerve cells) to which dopamine delivers its various messages, such as pay attention, control yourself, feel good, and do that thing that made you feel good again, the latter reflecting its role in promoting both addiction and learning. Dopamine transporters also protrude from the neurons that produce dopamine. Barkley describes them as “little vacuum cleaners” that absorb the unused dopamine in the brain so it can be used again.
One particular gene, DAT-1, has been implicated in both ADHD and bi-polar disorder and is very active in the basal ganglia and pre-frontal cortex, the brain regions that are smaller in people with ADHD. “DAT-1 genes build the dopamine transporters,” explains Barkley. “A certain version of that gene that’s longer than normal produces too many of those transporters—those vacuum cleaners—that are sucking up dopamine like there’s no tomorrow before it even has a chance to bind to dopamine receptors. ” Without dopamine, a personmay have difficulty learning and focusing, might have low motivation and become depressed.
There may also be mutations in dopamine-related genes that make neurons less receptive to dopamine’s effects, he says. What that means is that in people with ADHD, there’s less motivation—and pleasurable reward—for focusing, remembering, learning, planning ahead, and sitting still.
Other genes recently linked to the disorder strengthen the idea that ADHD is a fundamental communication system gone awry, a short-circuiting of the transmission between cells.
There are some non-genetic risk factors for ADHD: premature birth, maternal smoking and alcohol use, lead exposure, frequent maternal infections during pregnancy, and brain injuries. A 2009 German study found a significant link between having eczema, a rash caused by allergies, and developing ADHD symptoms, giving more credence to a controversial theory that at least some ADHD is the result of allergies or sensitivities to certain foods, food additives, or other environmental chemicals. Organophosphate pesticides—the kind used on most of the U.S. food supply—were linked to an increased risk of ADHD in a 2010 Harvard School of Public Health study which found that higher concentrations of pesticides in a child’s urine doubled the child’s chances of being diagnosed with the disorder. The takeaway: eat organic produce or at least wash your veggies. (See other approaches to try)
At most, however, these nongenetic factors only account for about 20% to 30% of cases, says Barkley. Ultimately, he believes, it will be genetic research that leads to more accurate diagnosis and treatment of ADHD, “telling us what caused a particular case and what drug to put someone on.”
Perhaps more important, both the brain and gene research has given parents like Monnica Williams a way to fight back against the ignorance they encounter from the strangers in the supermarket who tell them they must be feeding their children too much sugar or, in Williams’ case, the pastor who recommends regular spankings.
“I got lots and lots of advice from friends and family and well-meaning busybodies telling me that all they needed was more discipline, more structure, a change in diet. My kids have structure, discipline, and they’re all eating natural organic food,” says Williams, whose oldest son has ADHD and at the age of four, drew up an escape plan to get out of his daycare center. He made it to the front office before he was stopped. He recently graduated from Penn with a degree in physics. “ADHD is not just another word for bad parenting.”
One of the clues that lead researchers to look at the dopamine genes as possible markers of ADHD is the effect of methylphenidate—the drug known as Ritalin, a central nervous system stimulant and one of the early drugs used to treat ADHD. “Ritalin blocks those transformers that remove dopamine from the brain,” says Barkley. “That increases the amount of time that dopamine has to bind to neuron receptors.”
And in 70% to 90% of children who take Ritalin or one of the other stimulant drugs prescribed for ADHD, there’s an instant behavior change: They can focus, control their emotions, keep internal conversations from becoming constant babble, and sit still long enough to learn. The meds aren’t perfect though. “Their attention is still shorter than average with medication,” says Koplewicz. “They’re closer to average but not better than average.”
But the drugs work so well on symptoms that sales barely slowed in 2006 when the FDA—briefly—required them to carry a black box warning because of a small number (less than 50 over 10 years) of reported deaths, mostly related to heart damage. Another FDA panel withdrew the black box warning within a month.
So why does stimulant medication given to high-energy kids calm them down? That’s what baffled physician Charles Bradley in 1937 when he gave benzedrine, the only stimulant available at the time, to neurologically impaired kids for the severe headaches they suffered as the result of neurological exams during which most of the cerebrospinal fluid around their brains was drained. Benzedrine—known in ‘60s drug parlance as “bennies”—did nothing for their headaches, but it did improve their behavior and school performance and in some even tamed their fidgeting and emotional outbursts.
Today we know that stimulants such as Ritalin, Adderall and Vyvanse, like other drugs, have the opposite effect on children than the one they have on adults. For adults, they’re “speed”; in children with ADHD, they act more like a powerful new set of brakes for that racing Ferrari engine. (There’s no conclusive evidence that amphetamine drugs do anything beneficial for kids who don’t have ADHD.)
The proliferation of prescriptions has alarmed both conventional experts in ADHD who believe the drugs are godsends and their medical opposites who think they’re unnecessary. Moving cautiously is important, they say, not just because the drugs can have serious side effects, but also because they don’t cure ADHD. Diet, exercise, parenting techniques and therapy are extremely important as well.
Yet the majority of children with ADHD are getting only medication. “And we’ve known for 40 years that drugs [alone] don’t change any of the bad outcomes for which ADHD kids are at risk,” says the Center For Children and Family’s Pelham. “It improves the DSM [Diagnostic and Statistic Manual] symptoms, but it doesn’t improve impairment. Giving a child a pill doesn’t change parenting or social skills. Achievement in school is just as bad as if they haven’t had any treatment. The probability of graduating is exactly the same and it’s not good.” In other words, drugs don’t work on outcomes without the other piece of the puzzle—behavioral training that involves good parenting skills. (Drug Guide: Choosing the Right Medication)
Parents turn to drugs alone for a number of reasons. First, most of the pills work almost immediately to reduce the worst symptoms and they’re fairly easy to get. They’re usually covered by insurance, which makes them cheaper and less labor-intensive than going to parenting classes to learn science-based techniques that can change a child’s behavior or chauffeuring a kid to weekly therapy to learn appropriate social skills.
Parenting and behavior therapy is “a much longer term process, but it’s what lays down new neuronal skills based on learning which is much different than taking a pill that lets in a flood of dopamine and changes the child’s brain for a moment,” says Pelham.
Experts such as Pelham, Koplewicz, Hallowell, and Barkley are all proponents of medication, but not necessarily as a first-line treatment.
Pelham was part of the large, federally-sponsored, multi-site Multimodal Treatment of ADHD (MTA) study in the ‘90s which found that medications alone and a combination of drug and behavioral treatment were both superior to both behavioral therapy alone and to management of children with ADHD by a regular, non-specialist pediatrician.
He laments that the takeaway from the MTA research has been that pills alone work. His own research found that just under 40% of children who start with parent and behavioral therapy often don’t need medication, and those that still do, can get by with lower dosages.
Pelham and other experts hold that while bad parenting doesn’t cause ADHD, good parenting can help mitigate it. Research has produced evidence that good parenting can even trump bad genes. For example, in a 2012 study, University of Oregon scientists looked at the effects of parenting styles on children ages 18-21 months and later with children 3-4 years old, with the dopamine-related 7 repeat allele gene, which occurs in about 25% of children with ADHD. They found that children whose parents scored highest in “parent effectiveness”—meaning how supportive they were and how well they interacted with their children—were less likely to have symptoms such as inattention and excessive risk-taking than children of parents who had lower scores.
Pelham’s program—and there are other, similar ones, many community- and school-based—involves eight to 12 weeks of training, and most of it is for parents, not kids. Mothers and fathers learn to use positive reinforcement to encourage good behavior, age-appropriate punishments such as time-outs and loss of privileges to discourage bad behavior and a daily report card prepared by a child’s teacher that emphasizes a child’s successes on that day. They also learn how to give instructions to a child whose short-term (working) memory is impaired and who finds it tougher than normal to keep distractions at bay. Parents practice ways to minimize their responses to minor annoyances—like a 10-year-old who repeatedly puts her feet on the dining room table.
“Evidence of the past decade is that what improves parent-child interactions helps a child with ADHD do better,” says Child Mind’s Koplewicz, who uses similar techniques in his practice. “Parents who focus on the negatives reinforce negative behavior. How many times do you say, ‘Are you deaf? Didn’t you hear me tell you to clean up your room?’ instead of ‘thank you for cleaning up your room’ when they do it? I have kids who come into my office and when you ask them if they’re a good boy or a bad boy they say they’re bad because that’s their experience with the world. This does not help.”
In a column published recently in the New York Times, Richard A. Friedman, director of the psychopharmacology clinic at Weill Cornell Medical College, drew on the Kenya study, to suggest that many children with the genetic version of ADHD might benefit from education plans tailored to their needs for hands-on, fast-paced experiences high in novelty that, while unlikely to reduce their need for medication, could turn their disability into an asset.
Kerri Meenagh was fortunate. She’d learned about ADHD when she was studying for her pediatric nursing degree. But she still needed to spend time with the local school psychologist and a parent group called CHADD (Children and Adults with Attention-Deficient/Hyperactivity Disorder) to remind her how important it was to never consider Saorla a willful and disobedient child. “We need to remember that the way her brain works is different,” she says. “It’s not that she won’t control herself, it’s that she can’t.”
That, she said, changed some of the expectations she and her husband have for their daughter—and themselves.
“We’re both Catholics, so one of our goals was to go to Mass every Sunday. While most kids can find something to occupy them for 45 minutes at Mass, Saorla has to go to the bathroom at least three times. So we go to Mass and Saorla has to go to the bathroom three times. It doesn’t matter—every Sunday we meet our goal,” she says. “You adjust your expectations. I know she’s disorganized and forgetful and will spill her juice or milk every day. If I know that happens because she has a brain disorder, why would I get upset?”
The fact is, she takes delight in her daughter’s exuberance and individualism. “She sometimes puts together some interesting outfits but she really doesn’t care what other people think about her. I’m happy she’s her own person.”
And Saorla seems to gravitate towards activities that channel some of her risk taking and her copious energy, particularly performing. “When they told the third graders this year that they could try out for the school musical, she was one of only two third graders who tried out for the lead,” says Meenagh, laughing. “Her sister was horrified at her audacity. She didn’t get the lead, but she did get a speaking part. And she was a hit.”
When it comes to Irish dancing or performing, Saorla is an audience magnet. Her energy and expression make her a delight to watch. “And she seems to know that this is a way she can have positive experiences with people,” says Meenagh. “They really enjoy her. Performing makes her feel proud of herself and very confident. All that energy is more acceptable on stage and that’s where she feels at home.”
![]()
Nationally, the rates of ADHD diagnoses and medical treatment are on the rise, but the CDC’s map reveals dramatic differences between states, with a prevalence of ADHD diagnosis and drug treatment in the south.
What’s at work here? That’s what Stephen Hinshaw, PhD, vice chair of psychology in the department of psychiatry at the University of California in Berkeley wanted to know when he teamed with Berkeley health economist Richard M. Scheffler PhD, to drill down into the statistics. Here’s what they found:
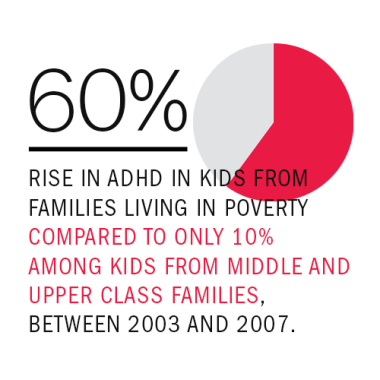
• Policy Change They traced the bump in ADHD diagnosis and treatment to education policies implemented in the south and midwest in the 1990s and the whole country after No Child Left Behind was introduced in 2001. These policies punished schools, usually by cutting their funding, if they didn’t raise their kids’ test scores. That meant there was a payoff if states with increased ADHD diagnoses, says Hinshaw, particularly among the poor where they rose an astonishing 60% between 2003 and 2007, compared to only 10% among kids from middle and upper class families. For one thing, a diagnosis can lead to treatment that could help underachieving students do better in the classroom and, as a result, increase mean test scores.
• Funding But “the more nefarious explanation,” says Hinshaw, is that school districts pick up a get out of jail free card by having more children diagnosed with ADHD. Thanks to a Supreme Court Ruling, kids with ADHD are considered special education students whose test scores are not taken into account when a district’s performance is tallied. Having a lot of students diagnosed with ADHD allows the districts to simply drop the scores of their lowest achievers and not lose any funding. “This was what policy people call an unintended consequence,” says Hinshaw. “I’m sure the authors of No Child Left Behind didn’t plan for this to happen.”
• Poverty Many of the districts with the highest rate of ADHD are also districts with a lot of folks living within 200% of the poverty line. Once ADHD was considered a “white middle class boy” diagnosis,” says Hinshaw, but since the 1990s, it has been a reimbursable condition under Medicaid, the federal health insurance program for the poor. However, Medicaid covers ADHD assessments and medication, but not other therapies which may also explain why rates of drug treatment are also on the rise. “As a result of all these policies and laws, Medicaid kids are more likely to have an ADHD diagnosis than middle class kids for the first time in history,” says Hinshaw. There may be other environmental factors that account for the statistical rise in ADHD, says Hinshaw, “but right now, this is as close to a smoking gun as we’ve got.”
![]()
Parents often go through a period of trial and error as they and their doctor try to find the right medication for their child. Here are some of the pros and cons of the most popular ADHD drugs
Stimulants
How they work: Increase levels of the neurotransmitter dopamine in the brain, stimulating cognition, attention and focus
• Ritalin and Methlphenidate-based Drugs
Ritalin LA, Ritalin SR, Methylin, Metadate, Focalin, Concerta, Quillivant XR
Duration: Lasts from 3-4 hours (Ritalin) to 10 hours (Quivallent XR)
Pros: Effective in 755 of the people who take it. The drug can be safely used in preschoolers. Newer, longer-lasting, once-a-day medications are available, including Ritalin LA, Ritalin SR, Metadate CD and Metadate ER, Concerta, Daytrana (a patch); Focalin XR, (a capsule filled with pellets that can be opened and hidden in food), and Quivallent XR, (a liquid)
Cons: May be habit-forming; can cause slowed growth, loss of appetite and weight, irritability, and surge of ADHD symptoms (called rebound symptoms) as it wears off. Ritalin and generics must be taken 2 to 3 times a day. They can increase anxiety and tics and are not as effective in toddlers as they are in older children; greater risk of side effects for younger children. Very rare side effects include sudden death.
• Adderall (mixed amphetamine)
Adderall XR, Vyvanse
Duration: 4-5 hours (Adderall) to 10-12 hours (Adderall RX, Vyvanse)
Pros: Effective in individuals who need a stronger drug than Ritalin, particularly teens and adults. Adderall XR and Vyvanse wear off more slowly with fewer rebound symptoms. Vyvanse is a once-daily pill for children 6 years and older.
Cons: May be habit-forming; can cause slowed growth, loss of appetite and weight, irritability, and restlessness. Very rare side effects include sudden death.
•Dexedrine, Dextrostat, Dexedrine Spansul
Duration: 4-5 hours (Dexedrine, Dextrostat) to 5-10 hours (Dexedrine Spansul)
Pros: Approved for children under six, slightly longer-acting than Ritalin. Dexedrine Spansul can eliminate mid-day doses in young children.
Cons: May be habit-forming and has the same potential side effects as other stimulants (see above.)
Nonstimulants
How they work: Increases dopamine circulating in the blood by decreasing blood pressure. Intuniv and Tenex may be combined with a stimulant for children who are very hyperactive, aggressive, and emotionally explosive.
• Strattera
blood pressure drugs Intuniv (time-released guanfacine; Tenex), Clonidine, Catapres, Kapvay; and some antidepressants
Duration: Up to 24 hours
Pros: These nonhabit-forming drugs can be an alternative to stimulants, though they’re usually used with them. They target specific symptoms like extreme hyperactivity and aggressiveness. Blood pressure drugs can also help children sleep and may treat anxiety, nervous habits and tics, and bedwetting.
Cons: Can be sedating. Clonidine drugs have cardiac effects that may make them inappropriate for children. Antidepressants can increase suicidal thoughts and actions in children and teens.
![]()
How much of a role does environment or diet play in ADHD? It’s hard to tell, but some experts recommend a couple of strategies that can augment if not replace medication. But remember: there’s no magic bullet. ADHD is not curable.
Diet:
• Cut down on artificial food-coloring In 2007, a placebo-controlled British study found that a variety of common food dyes and the preservative sodium benzoate cause some children to become much more hyperactive and distractible. The dyes are banned in Britain, but still allowed in U.S. foods, though the FDA has acknowledged that the artificial colorings are linked to behavior problems in children with ADHD and those who don’t have it.
• Try an elimination diet In a 2011 study, nearly two-thirds of the 27 children with ADHD who followed a strictly supervised elimination diet—which ultimately limited their menu choices to rice, meat, vegetables, pears, and water—over the course of nine weeks showed significant improvement in ADHD symptoms and oppositional defiant disorder, a pattern of angry, irritable behavior which often occurs with ADHD.
• Take Supplements Some specialists recommend omega-3 fatty acid supplements which, according to a 2014 German study of 95 children, helped bolster working memory. But the supplements had no effect on other symptoms of ADHD such as attention and the speed at which the children were able to process information.
• Switch to Organic ADHD has recently been linked to pesticides used on most of the U.S. food supply. An all-organic diet may reduce exposure by as much as 90%.
Brain Training:
• Try Neurofeedback Neurofeedback is a type of biofeedback that uses demonstrations of brain activity to teach self-regulation. A person can see in real time how his feelings or thought processes change his physical responses. A 2013 study found that children in 19 Boston-area elementary schools who did 40 sessions with a video-game-like program called Play Attention had increased attention spans, reduced hyperactivity, and fewer impulsive behaviors. The effect lasted for up to six months.
During neurofeedback, children wear headgear with electrodes that measure their brain waves, and play games on the computer aimed at altering those brain waves to make them calmer. They might, for example, have to focus on making dolphin dive into the ocean. After repeating the game countless times, the kids learn how to better control their brain waves, with some lasting effects.
Programs such as Play Attention are available for use at home, but they’re expensive—roughly $180 a month. In some cases, federal funding may be available.

Body Training:
• Exercise: Like stimulants, exercise can help increase dopamine levels in the basal ganglia—shown to be abnormal in ADHD kids—by increasing the number of receptors on nerve cells, at least in animal studies. Exercise also increases norepinephrine, the brain chemical linked particularly to ADHD’s fidgetiness. And it seems to have a calming influence on the amygdala, the “reptile” part of our brains that can make a child discomfited by new experiences and more emotionally volatile.
• Get Outside: Several studies by two researchers at the University of Illinois found that children with ADHD who play in outdoor green spaces like a park have milder symptoms than those who play indoors or in an urban setting.
![]()
Parenting—or working with—a kid with ADHD can be exhausting and tricky. Luckily, help is at hand. Here’s where to go for support, advice and as much information as you can use.
Helpful Organizations and Information
• Children and Adults with Attention Deficity/Hyperactivity Disorder is a national, nonprofit organization that provides education, advocacy and support for people with ADHD. It produces both print and web-based educational material on ADHD, reports on new research, and sponsors community support groups around the country.
• This website on ADHD from the National Institutes of Mental Health which gives basic information about the condition and up-to-the-minute news on scientific research
• The Centers for Disease Control and Prevention’s site on ADHD contains basic information about the condition, plus research, data and statistics, information on conferences and training, scientific articles, and ordering information foe free printed materials; there are also state data profiles and maps
• Charlotte Englehard blogs about the trials and tribulations—and joys—of raising a son with ADHD.
• Ruth Hughes, PhD, CEO of CHADD, writes about ADHD both as an expert in the field and the mother of a child with ADHD; occasional guest experts contribute.
• Brenda Nicholson was diagnosed at the age of 42 when she was having her children evaluated for ADHD. She is a life coach specializing in adults with ADH.
• ADDitude is a magazine for parents and others dealing with ADHD. It contains, articles, blogs, information on treatment, parenting, associated learning disabilities, as well as a resource guide and online support and informational groups.
