In September 2017, two weeks after Hurricane Irma pummeled South Georgia, Angela Ammons found her hospital on life support. It was her first day as CEO of Clinch Memorial Hospital. As she walked the halls, past oversized framed photos of the nearby Okefenokee Swamp, she felt relieved that the hurricane had spared the facility, but overwhelmed by the growing list of longstanding problems, from broken equipment to low staff morale. Soon after, an auditor informed Ammons of the hospital’s ninth consecutive year in the red. The hospital had just enough cash to pay for a couple more days of operations. With only two of its 25 patient beds filled and little revenue coming in, Ammons didn’t know if she could make payroll. If nothing changed, she would be forced to close a hospital that had served the 6,650-person Clinch County, including the small town of Homerville, Georgia, for over six decades.
“Rural hospitals are an endangered species,” says Jimmy Lewis, CEO of Hometown Health, a professional association of four dozen rural Georgia hospitals. Clinch Memorial, he thought then, might become the state’s eighth shuttered rural hospital since 2010. Even before the coronavirus pandemic halted elective surgeries and the income streams they produce, rural areas had too few insured patients to sustain the hospitals built to serve them. But their empty beds could be of value, if linked up with city hospitals now facing a different problem: overcapacity, especially during COVID-19.
In 2017, Ammons didn’t know that just yet. She just knew she had to move fast.


Ammons had never before run a hospital. The daughter of a Korean immigrant and Vietnam War veteran, she was raised by her grandparents in Macon, Georgia. But their tumultuous relationship forced Ammons to flee home at age 15. She nearly became homeless, relying on the goodwill of people she hardly knew to offer temporary housing as she cobbled together shifts at Shoney’s. Ammons eventually became the first person on her mother’s side of the family to earn a college degree. For more than a decade, she climbed the ranks from doctor’s receptionist to registered nurse supervising a team. After the four previous CEOs failed at a turnaround, Ammons convinced Clinch Memorial’s board that her experience overcoming hardships would provide a fighting chance at reviving the hospital.
The rookie CEO froze salaries, cut costs and collected payment upfront for elective procedures. It wasn’t enough. “I was scared to death, and I needed help,” says Ammons, aware of the fact that closure would not only force residents to travel outside the county to the next-closest hospital, but also dig a knife deep into the heart of Homerville’s economy. “We had to do something different.”
Clinch Memorial faced the same problems beleaguering many of America’s roughly 2,000 rural hospitals, which serve 57 million Americans – a sixth of the nation’s population. The University of North Carolina’s rural health research program, which has tracked over 170 rural hospital closures since 2005, found last year was the worst year for closures since the Great Recession. Nearly a quarter of those left are near insolvency, according to a 2019 analysis from consulting firm Navigant. Many rural hospitals struggle because a majority of their patients are uninsured, and they often don’t get fully reimbursed for that care by the government. Obamacare gave states the option to cover some of those uninsured by expanding Medicaid: Georgia did not. Rural hospitals are closing at higher rates in such states, while rural areas in states that expanded Medicaid saw sharp declines in uninsured rates, according to a 2018 Georgetown University study.
In states that did not expand Medicaid, such as Texas, Georgia and North Carolina, the rural hospital crisis forced leaders to take extreme measures to save facilities that offer not just the only medical care in miles, but well-paying jobs. In 2014, the mayor of a small North Carolina town marched hundreds of miles to Washington D.C. in a long-shot bid to keep his hospital open. In 2017, the administrator of a Tennessee hospital launched a six-figure GoFundMe campaign to make payroll. Last year, an Oklahoma hospital’s staff kept working even after the paychecks stopped coming to keep the town afloat. Elsewhere, hospitals execs once fighting over patients are now collaborating with each other in finding ways to stay afloat. The devastating spread of COVID-19, leading to large outbreaks in rural nursing homes, meatpacking plants, and prisons, have amplified the need for these hospitals. It has also exacerbated the financial pressures many of those facilities already faced.

As Ammons desperately searched the Internet for answers in the fall of 2017, she stumbled upon a story about a hospital on the other side of Georgia. Two and a half hours west in Colquitt, a town even smaller than Homerville, a CEO seemed to have found an innovative approach that exploited an inefficiency within America’s bloated health care system. Now those hospital beds were full of patients from large southern cities, pumping new life into a hospital once in peril. Ammons didn’t fully understand how it worked, so she picked up the phone and dialed the 229 area code on the Miller County Hospital website.
A lifeline for rural communities
When MCH CEO Robin Rau picked up, Ammons wasted no time asking for help. She sought mentorship from Rau on how to turn around Clinch Memorial. Rau could hear the desperation in Ammons’s voice. It resembled hers just a few years earlier.
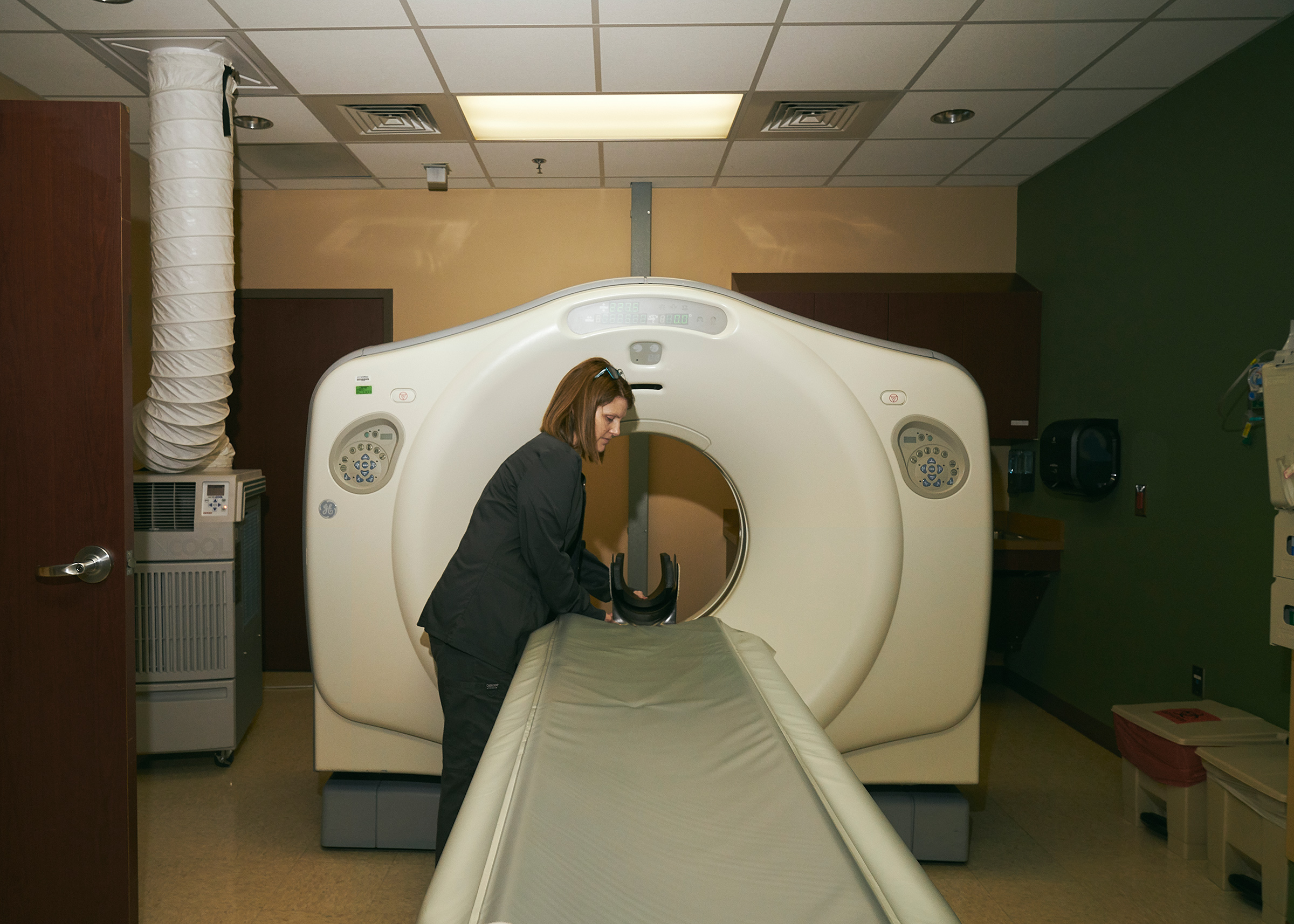
A seasoned hospital administrator, Rau joined MCH just as the Great Recession started. At her first board meeting, Rau says, a lender called due a note worth over $3 million. Rau only had $100,000 in the hospital’s bank account. To cut losses, Rau tried a counterintuitive solution: offer free primary care to uninsured emergency department patients. Though the strategy required spending money upfront, it ultimately lowered expenses for patients who came to the emergency department with minor ailments. She then drove the more than 200 miles to Atlanta’s Grady Memorial Hospital, which was cutting costs during a financial crisis of its own. While the public hospital was overcrowded with patients, Rau’s beds were mostly empty. Rau convinced Grady to transfer uninsured patients who were intubated and required ongoing ventilation following car crashes, gunshot wounds, and traumatic brain injuries – but no longer needed intensive care – to MCH.
Grady benefitted because it could offload post-acute patients for which it received a lower reimbursement rate. In return, Rau could bill the federal government for offering care to patients in MCH’s once-empty beds. She could do this because MCH is a critical-access hospital – a classification that allows small hospitals located in remote areas to be eligible for federal reimbursement so long as they treat any patient regardless of their ability to pay. Under that designation, Rau could also “swing” her beds from only patients in need of acute care to those who no longer require the emergency department but still needed more treatment before a nursing home. Though many rural hospitals employed “swing beds,” Rau was one of the first to use it as a major revenue driver.

The strategy worked: Rau kept open her hospital’s doors, paid off debt and expanded services. But Rau felt wary about divulging her strategy to another CEO. Over a decade’s time, the hospital industry had grown fiercely competitive. Urban health systems not only expanded their patient services, but also increased their footprints into rural regions. Rau watched as larger systems rarely invested in their rural facilities. “I thought, ‘Is this going to end up being competition for me?’” Rau later told TIME. But sensing Clinch Memorial had nowhere else to turn, Rau agreed to help Ammons implement a swing bed program of her own.
They started talking by phone each week, slowly becoming familiar with each other’s hospital operations. When Rau drove to Homerville for a tour of Clinch Memorial, she was shocked and saddened by what she saw. “There were no patients, nobody coming in,“ Rau says. “It was like a daggum ghost town!” By the end of 2017, Rau’s swing bed program that treated intubated patients had a long waiting list. So she offered to send Clinch Memorial some of the patients who were already being transported hours from cities like Atlanta, Jacksonville, and Tallahassee.
One of those patients, Derry Wells from southwest Georgia and in her early 50s, had maxed out the days insurance would pay for her stay at a larger 181-bed hospital. She could no longer speak and required a ventilator due to a worsening rare neurological disorder called corticobasal degeneration. Before she could go to a nursing home, her husband, Randy Wells, a minister with the Church of God, was told about Rau’s program at MCH. Due to the waiting list, he agreed to send Derry to Clinch Memorial, where staffers helped her through a series of respiratory treatments and physical therapy.
“I’d never stopped in Homerville before,” says Randy Wells. “There’s something about small-town hospitals where they build a better rapport with patients and family members. It’s more personable.”

Founded by a doctor in the mid-19th century, the city of Homerville once bustled thanks to the railroad and, later, Clinch Memorial, built in 1957 with funding made available by the Hill-Burton Act, a 1946 law that provided hospitals federal grants and guaranteed loans for construction. But the growth of America’s highway system choked off life to many rural railroad towns. Homerville’s shrinking population—down 26% since 1980—slowly affected Clinch Memorial. When a new hospital was built in the mid-2000s, the board approved a new facility with only half the beds of the original site.
From 2007 to 2009, during the Great Recession, the number of nonelderly Americans without insurance increased from 45 million to 50 million, according to a 2010 analysis from health policy journal Health Affairs. As unemployment rose, Americans delayed pricey health care procedures and avoided hospital visits. Between 2008 and 2013, Clinch Memorial’s patient admissions had halved in spite of the fact that Clinch County, where Homerville is located, is home to some of Georgia’s worst rates of smoking, obesity and cardiovascular disease. Those outcomes, coupled with severe doctor shortages and a high percentage of uninsured residents, have contributed to the area’s life expectancy of 72.7, six years younger than the national average.
In the months following, as more ambulances dropped off ventilator patients, Clinch Memorial started showing signs of life. Ammons was relieved to see her daily census grow from two patients to six – some days, it even hit double digits. But the work was just beginning. As more out-of-town patients arrived in Homerville, and dollars flowed in from Medicare, she began to invest in the area’s longer-term needs by planning a wellness center, and programs that urged residents toward healthier lifestyles. Clinch Memorial was able to hire its first full-time staff physician in over five years.
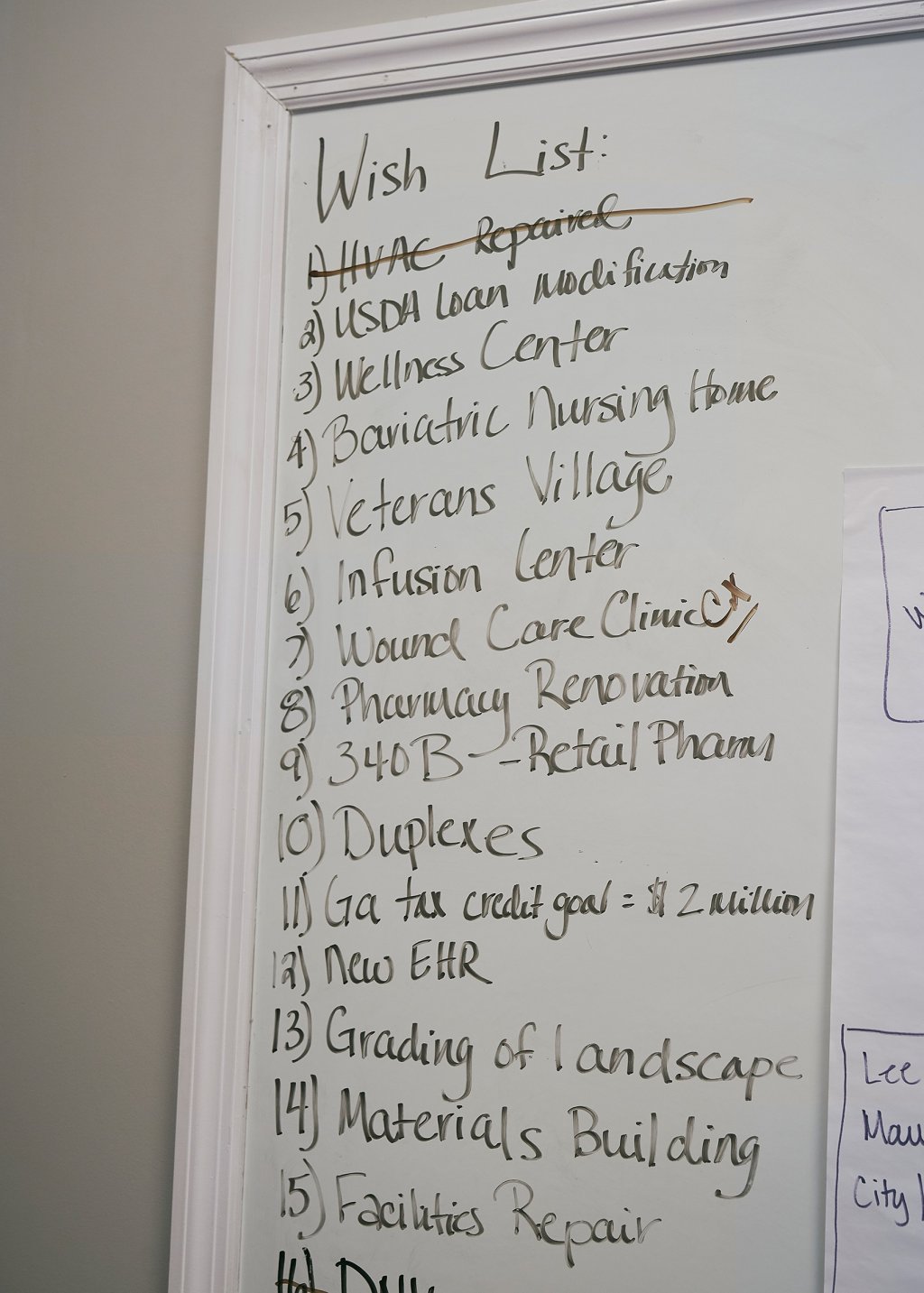
Hopeful as she was, Ammons wasn’t ready to let her guard down. One day last summer, nearly two years after her first day as CEO, Ammons reflected on the hospital’s progress, but minced no words about the work still to be done to ensure its long-term vitality. “We’re not out of the woods,” she said.
A future beyond better COVID-19 care
As rural hospitals had spent years looking for ways to fill their empty beds, they experimented with a variety of solutions to draw in patients from outside their communities. So far, few hospitals have implemented the specific practice embraced by Ammons and Rau, according to Mark Holmes, director of the University of North Carolina’s Cecil G. Sheps Center for Health Services Research. But he says it fits into a broader trend of critical-access hospitals developing a specialty service line to “release the strain” from larger facilities. Small rural hospitals have increased the number of elective surgeries – knee or hip replacements, for instance – at a higher rate than other medical facilities. By developing that niche, rural hospital administrators are hoping to draw patients away from larger facilities.
“Could every critical-access hospital do [what Ammons and Rau are doing]? No.” Holmes said, noting that there are only so many excess patients to go around. But the broader concept “has the potential to work nationwide,” he said.
This past January, Ammons drove up for a meeting at MCH, bringing good news to share with Rau. Clinch Memorial was now in the black for the first time since the Great Recession. And Ammons’s “swing bed” program had grown nearly seven-fold from revenues of $730,000 in 2017 to over $5 million in 2019. During her visit, Ammons strategized with Rau, in hopes of furthering her turnaround effort. As they talked, Rau spoke freely about the progress she liked, offering constructive criticism wherever she saw fit. “Angela’s got good ideas, different ideas, some that I wouldn’t do just yet,” Rau said, referring to Ammons’s decision to offer holistic services such as spa or massage therapy. “I worry about her spreading herself too thin.”

By the time COVID-19 arrived in Georgia, Ammons was ready to respond. Clinch Memorial could now accept larger hospitals’ patients who were already on ventilators but didn’t have the infectious disease. At the beginning of the pandemic, the swing bed program drew in over $1 million in monthly revenues, which offset losses caused by the state’s temporary ban on elective procedures during its shutdown.
This past summer Georgia’s COVID-19 cases surged to record levels, so much so that hospitals were entirely full. So when Ammons learned a hospital in nearby Waycross had diverted patients, she offered to take some of their non-COVID-19 patients to free up space. They agreed. For the first time since Ammons arrived in Homerville, Clinch Memorial’s beds were now full, and patients who might’ve been left waiting for a bed at other hospitals got admitted sooner.
“I know that many are just trying to survive the day to day, but we can’t forget that we will get past this,” Ammons said. “This pandemic has inspired a lot of innovation that we will use for years to come.”
More Must-Reads From TIME
- The 100 Most Influential People of 2024
- The Revolution of Yulia Navalnaya
- 6 Compliments That Land Every Time
- What's the Deal With the Bitcoin Halving?
- If You're Dating Right Now , You're Brave: Column
- The AI That Could Heal a Divided Internet
- Fallout Is a Brilliant Model for the Future of Video Game Adaptations
- Want Weekly Recs on What to Watch, Read, and More? Sign Up for Worth Your Time
Contact us at letters@time.com
